Bones and joints
Imaging modalities
1. Plain films. These are cheap, widely available and valuable screening tools in the preliminary assessment of osteoarticular symptoms. Standard views require a minimum of two views perpendicular to each other, e.g. antero-posterior and lateral projections. The pathological processes underlying osteolysis and osteosclerosis, e.g. infection, tumours, articular erosions, etc., are well advanced before they become radiographically visible and radiographs may appear normal despite the presence of significant bone and joint disease. Although there are limitations, plain films are very useful in the characterization and differential diagnosis of disease, e.g. trauma, bone tumours, arthritis. Despite the recent advances in imaging techniques, the radiograph remains the single most important investigation in the characterization of bone tumours.
2. Arthrography. The injection of radiographically positive (iodinated) and negative (air) contrast medium directly into the joint allows radiographic assessment of articular structures in conventional arthrography. The examination can then be supplemented with CT (CT arthrography) which provides more detailed assessment of intra-articular status and structures using bone and soft-tissue window settings. For optimal evaluation, reformatted CT images in three planes with MDCT are obtained. Arthrography using a dilute gadolinium-DTPA solution and imaging with MRI (MR arthrography) is increasingly used in the study of large joint disease, e.g. shoulder, hip and, to a lesser extent, wrist, elbow and ankle.
3. Radionuclide imaging. Bone scintigraphy enjoys a high sensitivity but a low specificity. It is widely used in the detection and follow-up of metastatic disease, characterization of lesions shown by other imaging modalities, and as a sensitive test for the detection of pathology such as infection.
4. Ultrasound (US). Advances in US technology have increasingly been applied to musculoskeletal disorders in both adult and paediatric age groups. Peri-articular structures (capsule, ligaments, and tendons) are optimally imaged. Under US-guidance, therapy to soft-tissue disease can be accurately targeted, joint fluid aspirated and arthrographic agents instilled into joints.
5. Computed tomography (CT). This is very useful in complex bone trauma for accurate surgical planning and also in many applications in assessment of bone tumours and infection. Joint anatomy and pathology in joints which are difficult to image in two perpendicular planes and in which there is bone overlap, e.g. shoulder, hip, sternoclavicular, sacroiliac joints are best depicted using CT. When employed in CT arthrography, the intra-articular status of joints can be optimally assessed.
6. Magnetic resonance imaging (MRI). MRI is the best imaging modality for joint assessment. In many joints, e.g. knee, it can be employed as the first and only means of imaging. In other joints, e.g. shoulder, MRI alone is used to image the rotator cuff, but MR arthrography is required for optimal imaging of the ligaments, capsule and labrum in post-traumatic instability. Direct MR arthrography using intra-articular injection of dilute gadolinium solution is also employed, in the hip primarily to image the labrum and in the wrist to assess the interosseous ligaments of the proximal carpal row and the triangular fibrocartilage. Indirect MR arthrography following intravenous (i.v.) injection of gadolinium-DTPA, which quickly diffuses into the joint via the synovium, is used in the detection and quantification of active synovitis, e.g. rheumatoid arthritis. This is particularly of value in small joints and in the post-operative assessment of large joints. MRI is widely used in the assessment of bone pathology such as tumour or infection.
Musculoskeletal magnetic resonance imaging – general points
1. The large variety of MR sequences provides an opportunity to tailor the sequences to the tissues that need to be optimally imaged. See Table 12.1.
Table 12.1
Optimizing magnetic resonance imaging sequences for musculoskeletal tissues
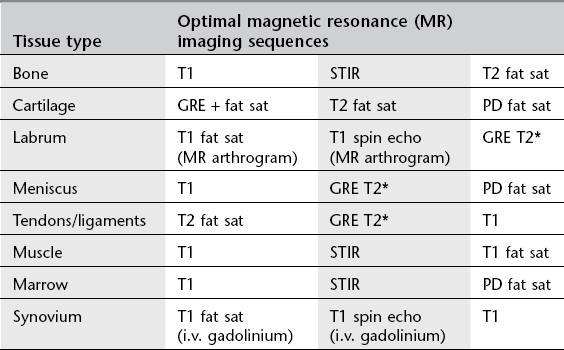
STIR = short tau inversion recovery; GRE = gradient echo; PD = proton density.
2. I.v. gadolinium-DTPA is used in musculoskeletal imaging for:
(a) infections – to differentiate abscess from phlegmon
(b) tumours – to differentiate viable tumour from necrosis – to differentiate solid from cystic components
(c) post-operative spine – to differentiate recurrent disc herniation from scar tissue
(d) synovial disease, e.g. rheumatoid arthritis – to determine activity/response to treatment
(e) avascular necrosis, e.g. Perthes’ disease, scaphoid fracture – to show viable tissue
(f) indirect MR arthrography – to delineate articular cartilage status, meniscal repair.
3. MR arthrography. Direct MR arthrography involves joint puncture and the intra-articular injection of a dilute gadolinium solution (saline and local anaesthetic can also be used). The amount of gadolinium needed to produce contrast by shortening the T1 effect of fluid is very small and too much gadolinium-DTPA results in signal loss of the fluid (‘black out’). Gadolinium-DTPA is, therefore, diluted in a ratio of 1 : 100 with sterile saline solution before use. The joint is distended and the recesses filled, delineating the intra-articular structures and separating them from adjacent tissues. In the lower limb, it allows accurate visualization of the labrum of the hip, the operated meniscus in the knee, and the impingement ankle syndromes, demonstrating associated osteochondral defects, loose bodies and synovial pathology more reliably than conventional MRI. In the upper limb, it is mostly utilized in the unstable shoulder to assess the damaged osteoarticular structures, the elbow and wrist joints. T1 spin echo and T1 fat-saturated sequences are used routinely in MR arthrography along with a T2 sequence in at least one plane to detect cysts, bone and soft-tissue oedema. Traction applied to joints at MR arthrography improves visualization of certain structures, e.g. long head of biceps origin in the shoulder, articular cartilage in the hip. MR arthrography avoids the requirement for diagnostic arthroscopy and aids in the therapeutic plan.
Arthrography – general points
1. The conventional radiographs should always be reviewed prior to the procedure.
2. Aspiration of an effusion should always be performed before contrast medium is injected. The aspirate should be sent, where appropriate, for microscopy, culture (aerobic and anaerobic) and sensitivity, crystal analysis, cytology and biochemistry.
3. Conventional arthrography has largely been replaced by MRI, e.g. knee. It is still the mainstay for diagnosing adhesive capsulitis, and in demonstrating the exact site of abnormal articular communications, e.g. wrist and foot. Most arthrograms are currently carried out as a prelude to either CT or MR arthrography.
4. If a needle is correctly sited within a joint space, a test injection of a small volume of contrast medium will stream away from the needle tip around the joint. However, if it is incorrectly sited, the contrast medium will remain in a diffuse cloud around the tip of the needle. For this reason, it is important that the fluoroscopy-guided needle approach should aim to visualize the needle tip at all times during its trajectory. In the knee, fluoroscopy in the AP plane is used as the needle is advanced from a lateral approach; fluoroscopy of the ankle in the lateral projection allows needle-tip visualization as it is advanced via an anterior approach.
5. Needle placement may be ‘blind’ or under image guidance, e.g. fluoroscopy, CT, CT fluoroscopy or US. Measured effective doses given by an experienced radiologist show significant differences; in shoulder arthrography – fluoroscopy (0.0015 mSv), single slice CT (0.18 mSv) and CT fluoroscopy (0.22 mSv).1
6. The positive contrast medium is absorbed from the joint and excreted from the body in a few hours. However, intra-articular air may take up to 4 days to be completely absorbed from the joint space. Every effort should be made to eliminate air bubbles at injection for MR arthrography as they create artifacts.
7. Arthrography is well tolerated by patients with discomfort rated less severe than general MRI-related patient discomfort.2
8. Arthrography is a very safe procedure with low complication rates. In a major study there were 3.8% minor complications (vasovagal reaction, pain, synovitis) and 0.02% major complications (anaphylactic reaction, infection, vascular).3 This included 13 300 MR arthrograms with only a 0.03% complication rate, all of which were minor.
9. In the scheduling of CT and MR arthrography it is important to ensure that the examination is carried out within 30 min of fluoroscopy-guided contrast medium intra-articular instillation. After this time contrast medium absorption will result in a suboptimal examination with resultant difficulties in interpretation.
Arthrography
Indications
1. Intra-articular structures, e.g. cartilage, labrum and tendons. The exact status of cartilage overlying osteochondritis dissecans (knee, ankle), labral tears (shoulder and hip) and anchor point of the long head of biceps requires CT or MR arthrography for accurate diagnosis.
2. Capsular, ligamentous and tendon injuries. Information regarding the presence, type, extent, gap and edges of torn capsular and peri-capsular structures (glenohumeral ligaments, rotator cuff tendons, lateral ankle ligaments) requires CT/MR arthrography.
3. Loose body. Loose bodies can be solitary or multiple, radiolucent or radio-opaque. CT arthrography using dilute contrast medium solution best depicts radiolucent bodies. Double-contrast CT arthrography using only a small amount of positive contrast medium is best to delineate radio-opaque loose bodies, determine true size and assess articular status of the joint.
4. Para-articular cyst. Synovial cysts and ganglia within para-articular soft tissues and bones can present with space-occupying lesions, which may migrate some distance away from the joint source of origin (popliteal cysts, iliopsoas bursa). Arthrography can demonstrate the articular communication either immediately or on delayed imaging.
5. Prosthesis assessment, e.g. loosening, infection. Arthrography demonstrates abnormal interposition of contrast medium indicating loosening at the cement/bone or metal/bone interface depending on the type of arthroplasty procedure carried out, while joint irrigation and aspiration fluid specimens are needed to confirm associated infection. Subtraction radiographic techniques are employed to facilitate interpretation, as the metal prosthesis and the barium-impregnated cement are subtracted out of the final image.
6. Pain block, e.g. bupivacaine ± steroid therapy. For difficult therapeutic decisions, diagnostic tests to confirm the pain source origin are increasingly being employed by instilling 0.5% bupivacaine intra-articularly. The addition of a steroid preparation can also aid in a longer period of pain control. If required, the injectate may act as the arthrographic agent for MRI done immediately after the pain block.
7. Confirm location of calcified para-articular soft-tissue masses. Calcified or ossified soft-tissue lesions in a para-articular location may or may not be intra-articular (e.g. synovial osteochondromatosis, myositis ossificans) requiring CT arthrography to help in their accurate localization.
8. Diagnosis and distension therapy in adhesive capsulitis. Usually employed in the shoulder in the treatment of frozen shoulder, the combination of anaesthetic, steroid and saline can be used to distend and rupture the joint after arthrographic confirmation of the diagnosis.
9. Intra-articular chemical therapy, e.g. hyaluronic acid, fibrinolysis, radioactive synovectomy. The intra-articular injection of hyaluronic acid in joints suffering from mild to moderate osteoarthritis produces viscosupplementation of joint fluid, reducing pain and increasing the articular cartilage thickness. In fibrin-laden effusions due to chronic rheumatoid arthritis, injected intra-articular fibrinolytic agents aid in the aspiration of the joint fluid.
Contraindications
1. Local sepsis
2. Allergy to iodine or gadolinium
3. Contraindication to MRI (see Chapter 2); consider CT arthrography.
Contrast medium
Conventional/CT arthrography
Low osmolar contrast material (LOCM) is used, the most common of which are iohexol and iopamidol. A higher concentration is needed in larger joints but for the purposes of CT arthrography, especially in tight joints, a dilute solution (100–150 mg iodine/100 ml) has distinct advantages. Volume of contrast medium needed is directly proportional to the capacity of the joint in question, e.g. 15 ml in the shoulder, 6 ml in the elbow and 3 ml in the wrist. Double-contrast examination of the knee for a CT arthrogram to assess the patellofemoral joint requires 4 ml iodinated contrast medium with 40 ml of air.
Radiographic views
1. AP and lateral views are routinely obtained after arthrography.
2. Additional axial (e.g. shoulder) and oblique (e.g. ankle) views may be helpful.
3. Dynamic assessment under fluoroscopic imaging with stress views may be useful, e.g. inversion/eversion in the ankle; abduction/adduction, weight-bearing views of the shoulder.
4. Erect posture with external and internal rotation views in double-contrast shoulder studies.
5. Radial and ulnar deviation views in radio-carpal, midcarpal and inferior radio-ulnar joints.
Aftercare
Driving after the procedure is not advisable. The patient is warned that there may be some discomfort in the joint for 1–2 days after the procedure. It is also necessary to refrain from strenuous exercise during this time. The injected air for a double-contrast procedure precludes air travel.
References
1. Binkert, CA, Verdun, FR, Zanetti, M, et al. CT arthrography of the glenohumeral joint: CT fluoroscopy versus conventional CT and fluoroscopy – comparison of image guidance techniques. Radiology. 2003; 229:153–158.
2. Binkert, CA, Zanetti, M, Hodler, J. Patient’s assessment of discomfort during MR arthrography of the shoulder. Radiology. 2001; 221:775–778.
3. Hugo, PC, Newberg, AH, Newman, JS, et al. Complications of arthrography. Sem Musculoskelet Radiol. 1998; 2(4):345–348.
Andreisek, G, Duc, SR, Froehlich, JM, et al. MR arthrography of the shoulder, hip, and wrist: evaluation of contrast dynamics and image quality with increasing injection-to-imaging time. Am J Roentgenol. 2007; 188(4):1081–1088.
Tehranzadeh, J, Mossop, EP, Golshan-Momeni, M. Therapeutic arthrography and bursography. Orthop Clin North Am. 2006; 37(3):393–408.
Arthrography – site-specific issues
There are various needle approaches using image guidance and the most commonly used ones are described.
Knee
Technique
1. The patient lies supine; either a medial or a lateral approach can be used and it is as well to be familiar with both.
2. Using a sterile technique, the skin and underlying soft tissue are anaesthetized at a point 1–2 cm posterior to the mid-point of the patella.
3. A 21G needle is advanced into the joint space from this point by angling it slightly anteriorly so the tip comes to lie against the posterior surface of the patella. By virtue of the anatomy, the tip of the needle must be within the joint space (Fig. 12.1). A more horizontal approach may result in the needle penetrating the infra-patellar fat pad, resulting in an extra-articular injection of contrast.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






