BONY ORBIT AND EXTRACONAL COMPARTMENT: DEVELOPMENTAL LESIONS
KEY POINTS
- Computed tomography and magnetic resonance imaging are in the critical pathway for evaluating the signs and/or symptoms that are related to an extraconal mass.
- Computed tomography and magnetic resonance imaging are extremely useful for narrowing the differential diagnosis solely to dermoid cyst.
- Imaging with magnetic resonance or computed tomography is less specific for the diagnosis of ectopic brain.
Developmental abnormalities of the eye and orbit and alterations in the size of these structures may be isolated findings. These anomalies may be associated with other findings involving the visual system and may also be seen as part of syndromes and other more generalized genetic errors. Once a potentially developmental abnormality of the orbit is recognized, it becomes important to identify such possible related conditions and their likely origin. The orbital anomalies related to eye development are discussed in Chapter 46. Those associated with craniofacial anomalies are discussed in Chapter 79.
Since venolymphatic malformations are discussed in Chapters 9 and 59 and encephaloceles are primarily related to the midline of the face and sinonasal region, this chapter deals only with orbital dermoid cysts and the very rare occurrence of ectopic brain tissue in the orbit. Neural cysts related to abnormal development of the eye are discussed in Chapter 46.
Any orbital mass or disease process may be approached by first establishing whether it is preseptal (Chapters 70 and 71) or postseptal (Chapters 57–60, 62, and 64). If postseptal, it should be established as a process arising primarily intraconally (Chapters 57–60), extraconally (Chapters 62 and 64), or transcompartmentally. If intraconal, it should be decided whether the mass is of optic nerve/sheath origin or arises from some other structure comprising or within the muscle cone. Orbital dermoid cysts are typically extraconal, but they may be intraconal. The opposite is generally true of ectopic brain tissue.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Embryology
The bony orbit develops from several mesodermal sources, some of which are related to the brain and some to the soft tissues of the orbit. There is ample opportunity for ectodermal elements to get tangled up with these several blocks of mesoderm. There is also potential for rests of neuroepithelium to be trapped during development.
The development of the eyelid with its many functional components also produces ample opportunity for rests of ectoderm to be left where they do not belong. These highly complex developmental circumstances explain why the most common, nonvasoformative congenital abnormality of the orbit in both the pre- and postseptal space, is a dermoid cyst (Chapter 8). Heterotopic brain may present partially in the orbit but is primarily a naso-orbital phenomenon (Chapter 8).
Applied Anatomy
The relevant anatomy of the bony orbit, muscle cone, and related neurovascular structures is discussed in detail in Chapter 44. In particular, the anatomy of the orbital periosteum, orbital septum, and attachments of the muscle cone at the orbital apex should be reviewed. The subperiosteal space within the extraconal, postseptal compartment lies between cortical bone and its adjacent periosteum. The postseptal extraconal space lies between the periosteum and muscle cone and contains fat and small nerves and vessels.
IMAGING APPROACH
Techniques and Relevant Aspects
The orbit is studied with computed tomography (CT) and magnetic resonance (MR) techniques described in detail in Chapters 44 and 45. Specific CT protocols by indications are detailed in Appendix A. Specific MR protocols by indications are outlined in Appendix B. Almost all studies to investigate orbital tumors are done with contrast except if the lesion is of known fibro-osseous origin or if magnetic resonance imaging (MRI) has already been done with contrast and a CT is being competed for bone-related information.
Pros and Cons
Masses of the extraconal orbital spaces are studied with CT and MRI. CT may be done first since it is more definitive in its rendering of bone detail, which is often pivotal in diagnosis. MRI is likely to be more sensitive than CT to related intracranial abnormalities or connections to the central nervous system.
CT may also be done first if the lesion is likely to have an obvious bony component. CT is a reasonable secondary screening tool for identifying intracranial extension of disease and related intracranial findings if for some reason MRI cannot be done.
SPECIFIC DISEASE/CONDITION
Dermoid Cysts and Ectopic Brain Tissue
Etiology
These are generally spontaneous developmental abnormalities.
Prevalence and Epidemiology
Dermoid cysts are by far the most common cystic mass to affect the orbit in children. They may present in young adults. Ectopic brain tissue in the orbit or eye is essentially a curiosity that will be suspected of being some other type of lesion until it is excised and examined histologically. Neural cysts associated with colobomas may be syndromic; those cysts are discussed in Chapter 46.
Clinical Presentation
Dermoid cysts typically present as a painless orbital mass, most typically in the upper outer quadrant in a pediatric patient. Less commonly, a dermoid cyst may rupture and will present with marked orbital inflammation that must be differentiated from orbital cellulitis.
Ectopic brain tissue may present with visual loss, proptosis, or as a mass.
Pathophysiology and Patterns of Disease
Dermoid cysts and ectopic brain tissue grow in a fashion typical of benign conditions as described in Chapter 21. Orbital dermoid cysts are almost always extraconal and may be preseptal, but they are rarely intraconal (Figs. 8.2 and 61.1–61.5). Ectopic brain tissue is more likely to be intraconal and even intraocular but may be extraconal (Fig. 61.6).
Extraconal orbital lesions may involve the postseptal extraconal space, subperiosteal space, and bone. Since dermoid cysts arise from ectodermal cells that become trapped between blocks of mesenchyme forming the various layers in this compartment, they may have components both within the soft tissues and/or bone.
Heterotopic brain tissue arises mainly intraconally since the eye and optic nerve form in large part as extensions of brain development. Theories regarding pathogenesis include (a) herniation of normal embryonic neuroepithelium with subsequent sequestration, (b) transformation of dysplastic neural rests with aberrant differentiation potential, or (c) preferential development of one layer in a teratoma into neural cell lines.1
Manifestations and Findings
Computed Tomography, Magnetic Resonance Imaging, and Ultrasound
The CT and MR appearance of dermoid cysts and ectopic brain tissue are discussed in Chapter 8. In the orbit, these cysts may be as small as from 3 to 5 mm and located in the preseptal soft tissues. At the other end of the spectrum are those that measure several centimeters and are complex, multicystic masses that may contain various ectodermal-derived tissues and cause remodeling of the bone of the lacrimal fossa and/or have tracts extending from a predominantly extraosseous mass into bone.
The cyst contents are variable in their behavior on T1- and T2-weighted images for reasons discussed in Chapter 8.

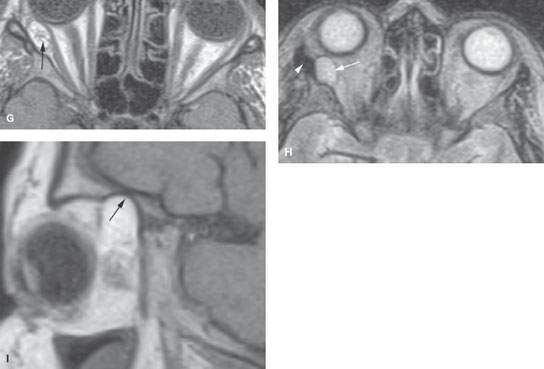
FIGURE 61.1. Computed tomography (CT) and magnetic resonance imaging (MRI) of a patient with a complex dermoid cyst of lacrimal fossa. A: CT shows the orbital mass in the upper outer quadrant containing fat (arrows) and lobulated soft tissue or fluid components (arrowheads). The mass is associated with bony defect in the supraorbital rim (black arrow). B: Bone windows show the tract extending into the bone of the supraorbital rim (arrows). C: Surface coil T1-weighted (T1W) image done show the fatty (black arrow) and fluid/tissue areas within the dermoid cyst (arrowheads). It also correlates well with the CT study showing a portion of the dermoid cyst tethered to the bone (white arrow). D: T1W sagittal image shows the mass (arrow) causing thinning of the orbital roof. E: A second patient believed clinically to have a dermoid cyst in the lacrimal fossa region. In (E), the mass is shown in the upper out quadrant (arrows). A tissue density structure (arrowhead) could have been part of the mass or possibly a displaced portion of the lacrimal gland. F: Mass caused marked regressive remodeling and thinning of bone (arrow) and areas of dehiscence (arrowhead) consistent with its chronic timetable of expansion. (NOTE: This cystic mass actually turned out to be a posttraumatic cholesterol (hematocyst, traumatic) cyst. There was no definitive traumatic event identified by the patient.) G–I: A patient with a dermoid cyst discovered incidentally on MRI done for headaches. In (G), the T1W axial image shows a complex partially fatty and partially tissue mass in the extraconal space (arrow). In (H), the T2-weighted images show the mass to remain roughly equivalent to fat (arrow). There did appear to be some dysmorphic change in the lateral orbital wall (arrowhead). In (I), the T1W sagittal image shows the mass to cause remodeling along the orbital roof (arrowhead).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








