GROSS ANATOMY
Divisions
- •
Esophagus
- ○
Cervical and thoracic segments
- ○
- •
Stomach
- ○
Hollow muscular organ between esophagus and small intestine
- ○
Location: Intraperitoneal, in left upper quadrant, bordered superiorly by left hemidiaphragm, posterolaterally by spleen, posteroinferiorly by pancreas
- –
Greater omentum attached from greater curvature and drapes over small and large intestines
- –
Lesser omentum attached from lesser curvature to porta hepatis, covers lesser sac
- –
- ○
Function
- –
Gastric acid production for breakdown of large molecules of food into smaller molecules in preparation for small intestinal absorption
- –
Storage of food
- –
- ○
Sections
- –
Gastroesophageal junction/cardia, lower esophageal sphincter
- –
Fundus and body: Delineated by horizontal plane passing through cardia
- –
Antrum/pylorus: Lower section facilitating entry of gastric contents into duodenum
- –
- ○
Curvatures
- –
Greater curvature: Lateral wall of stomach
- –
Lesser curvature: Medial wall of stomach
- –
- ○
Rugae/internal ridges increase surface area for digestion
- ○
Arterial supply
- –
Right and left gastric arteries supply lesser curvature
- –
Right and left gastroepiploic arteries supply greater curvature
- –
Short gastric artery supplies fundus
- –
- ○
Venous drainage
- –
Follow arteries and drain into portal vein and its tributaries
- –
- ○
- •
Small bowel
- ○
Between stomach and large intestine
- ○
~ 4-7 meters in length
- ○
Centrally located in abdomen
- ○
Intraperitoneal, except for 2nd-4th portions of duodenum
- ○
Function: Further breakdown of food molecules from stomach with eventual absorption
- ○
Intraluminal extensions/folds valvulae conniventes increase surface area for absorption
- –
Abundant in proximal small bowel, decrease in number in distal small bowel loops
- –
- ○
Duodenum
- –
C-shaped hollow tube connecting stomach with jejunum
- –
Begins with duodenal bulb, ends in ligament of Treitz (duodenojejunal junction)
- –
Arterial supply and venous drainage: Superior and inferior pancreaticoduodenal artery, pancreaticoduodenal veins
- –
- ○
Jejunum
- –
Connects duodenum with ileum
- –
~ 2.5 meters in length
- –
Begins at ligament of Treitz
- –
Along with ileum, suspended by mesentery
- –
Arterial supply and venous drainage: Superior mesenteric artery and vein
- –
- ○
Ileum
- –
Connects jejunum with ascending colon
- –
~ 3.5 meters in length
- –
Along with jejunum, suspended by mesentery
- –
Arterial supply and venous drainage: Superior mesenteric artery and vein
- –
- ○
- •
Large bowel
- ○
Between small bowel and anus
- ○
~ 1.5 meters in length
- ○
Peripherally located in abdomen
- –
Cecum and appendix, transverse colon, and rectosigmoid intraperitoneal
- –
Ascending colon, descending colon, and middle rectum retroperitoneal
- –
Distal rectum extraperitoneal
- –
- ○
Function: Absorption of remaining water, storage, and elimination of waste
- ○
Sections
- –
Ascending colon: Located in right side of abdomen, includes cecum where appendix arises
- –
Hepatic flexure: Turn of colon at liver
- –
Transverse colon: Traverses upper abdomen
- –
Splenic flexure: Turn of colon at spleen
- –
Descending colon: Left side of abdomen
- –
Sigmoid/rectum: At posterior pelvis
- –
- ○
With taenia coli: 3 bands of smooth muscle just under serosa
- –
Haustration: Sacculations in colon resulting from contraction of taenia coli
- –
Epiploic appendages: Small fat accumulations on viscera
- –
- ○
Arterial supply
- –
Superior mesenteric artery supplies colon from appendix through splenic flexure
- –
Ileocolic branch supplies cecum
- –
Right colic branch supplies ascending colon
- –
Middle colic branch supplies transverse colon
- –
Inferior mesenteric artery supplies descending colon through rectum
- –
Left colic branch supplies descending colon
- –
Sigmoid branches supply sigmoid
- –
Superior rectal artery supplies superior rectum
- –
Middle and inferior rectum supplied by arteries of same name originating from internal iliac artery
- –
- ○
Venous drainage
- –
Superior and inferior mesenteric veins
- –
- ○
- •
Anus
- ○
External opening of rectum
- –
Termination of gastrointestinal tract
- –
- ○
With sphincters for controlling defecation
- ○
Internal anal sphincter
- –
Thin ring of smooth muscle surrounding anal canal, deep to submucosa
- –
Under involuntary control
- –
Continuous with muscularis propria of rectum
- –
Forms incomplete ring in females
- –
- ○
External anal sphincter
- –
Thick ring of skeletal muscle around internal anal sphincter
- –
Under voluntary control
- –
3 parts from superior to inferior: Deep, superficial, and subcutaneous
- –
- ○
Longitudinal muscle
- –
Thin muscle between internal and external anal sphincters
- –
Conjoined muscle from muscularis propria of rectum and levator ani
- –
- ○
Histology
- •
Bowel wall throughout GI tract has uniform general histology, comprised of 4 layers
- ○
Mucosa
- –
Functions for absorption and secretion
- –
Composed of epithelium and loose connective tissue
- –
Lamina propria
- –
Muscularis mucosa (deep layer of mucosa)
- –
- ○
Submucosa
- –
Consists of fibrous connective tissue
- –
Contains Meissner plexus
- –
- ○
Muscularis externa
- –
Muscular layer responsible for peristalsis or propulsion of food through gut
- –
Contains Auerbach plexus
- –
- ○
Serosa
- –
Epithelial lining continuous with peritoneum
- –
- ○
IMAGING ANATOMY
Overview
- •
GI tract extends from mouth to anus
- •
Esophagus, which is intrathoracic, is difficult to visualize with external ultrasound due to rib cage and air-containing lungs
- ○
Endoluminal ultrasound performed to assess mural pathology
- ○
- •
Stomach to rectum lie within abdomen and pelvis
- •
Stomach, 1st part of duodenum, jejunum, ileum, transverse colon, and sigmoid colon suspended within peritoneal cavity by peritoneal folds and are mobile
- •
2nd-4th parts of duodenum, ascending colon, descending colon, and rectum typically extraperitoneal/retroperitoneal
- ○
Retroperitoneal structures have more fixed position and are easy to locate
- ○
- •
Stomach located in left upper quadrant
- ○
Identified by presence of rugae/mural folds
- ○
Prominent muscular layer facilitates identification of pylorus
- ○
- •
Small bowel loops are located centrally within abdomen
- ○
Abundant valvulae conniventes helps identify jejunal loops
- ○
Jejunalization of ileum seen in celiac disease to compensate for atrophy of folds in proximal small bowel
- ○
Contents of jejunal loops usually liquid and appear hypoechoic/anechoic
- ○
- •
Cecum and colon identified by haustral pattern
- ○
Located peripherally in abdomen
- ○
Contain feces and gas
- ○
Haustra seen as prominent curvilinear echogenic arcs with posterior reverberation
- ○
Cecum identified by curvilinear arc of hyperechogenicity (representing feces and gas) in right lower quadrant blind ending caudally
- ○
Not uncommonly, cecum high lying and may be horizontally placed
- ○
Sigmoid colon variable length and mobile
- ○
Junction of left colon with sigmoid colon identified in left iliac fossa by tracing descending colon
- ○
Rectosigmoid junction has fixed position and is identified with full bladder, which acts as acoustic window
- ○
- •
Appendicular base normally located in right lower quadrant
- ○
Length and direction of tip vary
- ○
Retrocecal appendix and pelvic appendix can be difficult to locate transabdominally
- –
Transvaginal ultrasound examination useful to identify pelvic appendix
- –
- ○
- •
Normal measurements of bowel caliber
- ○
Small bowel < 3 cm
- ○
Large bowel
- –
Cecum < 9 cm
- –
Transverse colon < 6 cm
- –
- ○
- •
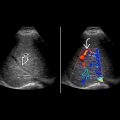
Stratified appearance of bowel wall on histology is depicted by 5 distinct layers on ultrasound as alternating echogenic/sonolucent (hypoechoic) appearance (gut signature)
- ○
Interface of lumen and mucosa: Echogenic
- ○
Muscularis mucosa: Hypoechoic
- ○
Submucosa: Echogenic
- ○
Muscularis propria/externa: Hypoechoic
- ○
Serosa: Echogenic
- ○
- •
Normal bowel wall thickness < 3 mm
Bowel Motility
- •
Bowel is hollow viscus and is constantly mobile due to peristalsis
- ○
Assessing direction of flow of contents often challenging
- ○
When visibility permits, direction of flow can be determined by following long segments of bowel in continuous fashion
- ○
- •
Different bowel pathologies have potential to alter normal gut motility
- •
Real-time dynamic ultrasound provides useful information regarding bowel mobility, which can aid in diagnosis of underlying condition
- ○
Cine function useful to store dynamic images for review
- ○
Imaging Recommendations
- •
Ultrasound is the initial study of choice for gastrointestinal conditions in children and young adults and for select indications in adults
- ○
Focused survey for acute appendicitis, pyloric stenosis, intussusception, and malrotation
- ○
Extended systematic survey in Crohn disease
- ○
- •
5- to 8-MHz curvilinear probe for wider field of view and deeper penetration
- •
7- to 12-MHz linear probe for higher resolution
- •
12- to 18-MHz linear probe for delineation of 5 bowel layers
- •
Fixed points of bowel easy to assess with transabdominal ultrasound: Pylorus, “C loop” of duodenum, and ileocecal junction
- •
Abnormal bowel identified as thickened or dilated segments, ± disturbance of gut signature
- ○
Thickened bowel demonstrates reduced peristalsis, which stands out among normally peristalsing loops of normal bowel
- ○
- •
Optimize settings, evaluate abnormal bowel in 2 planes
- •
Slow, graded compression
- •
Evaluate surrounding tissues for secondary signs: Echogenic fat, fluid, enlarged lymph nodes, tracts
- •
Color Doppler: Increased vascularity in acute inflammation, may be helpful in malrotation
GASTROINTESTINAL TRACT IN SITU