Brain Metastases
Todd M. Blodgett, MD
Alex Ryan, MD
Marios Papachristou, MD
Key Facts
Imaging Findings
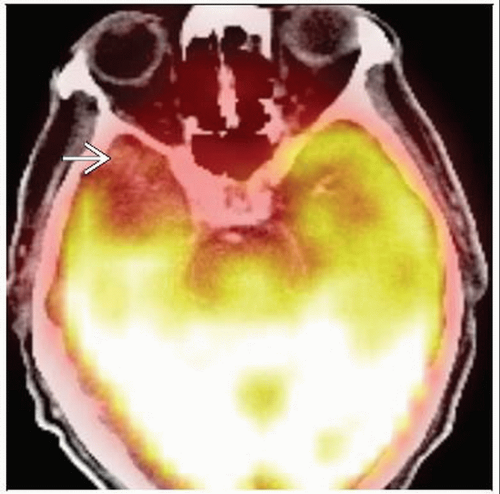
Focal hypermetabolic activity in the brain or spinal cord
Can detect ≈ 1.5 cm metastases
Cannot rule out small metastases with PET (C+ MR gold standard)
Normal brain metabolism of FDG (glucose) can hide small metastases
To increase sensitivity, re-window image to make normal brain activity less intense
CECT
Ring enhancement
FDG PET
Activity in CNS metastases depends on tumor histology
Sensitivity 79-82% specificity, 94% for detection of primary origin
Early studies showed 81-86% sensitivity and 40-94% specificity for distinguishing between radiation necrosis and tumor
Top Differential Diagnoses
Abscess
Central hypometabolism signifies necrosis
Cerebrovascular Accident
Primary Brain Tumor
Post-Treatment Effects
Diagnostic Checklist
Cases have been described in which primary lung tumors showed hypermetabolic foci, but brain lesions are photopenic
TERMINOLOGY
Abbreviations and Synonyms
Central nervous system (CNS) metastases, brain metastases
Definitions
Secondary tumors in brain or spinal cord originating from primary extracranial or CNS malignancy
IMAGING FINDINGS
General Features
Best diagnostic clue: Focal hypermetabolic activity in the brain or spinal cord
Location
Classic
Cerebral hemispheres (80%)
Cerebellum (15%)
Basal ganglia (3%)
Less common
Choroid plexus
Ventricular ependyma
Pituitary gland
Pineal gland
Leptomeninges
Uncommon
Diffusely infiltrating tumors (carcinomatous encephalitis)
Perivascular
Perineural
Rare
Brainstem
Size: Microscopic to several cm
Morphology
Usually discrete, spherical
Infiltrating
Along vascular or neural structures
Number of lesions
One (50%)
Two (20%)
≥ Three (30%)
Imaging Recommendations
Best imaging tool
FDG PET
Protocol advice
Normal brain metabolism of FDG (glucose) can hide small metastases
To increase sensitivity, re-window image to make normal brain activity less intense
Review 3D and tomographic images
Glucose loading can enhance detection of brain tumors, with 27% increase in FDG uptake ratio of tumor to normal gray matter
Difficult to perform clinically; requires IV glucose infusion and blood glucose monitoring
10% glucose 50 mL for 5 minutes IV
FDG imaging 3-8 hours after injection can improve distinction between tumor and normal gray matter
CT Findings
NECT
Iso- or hypodense mass
Peritumoral edema: None to striking
Intracranial hemorrhage (ICH) variable
Mets may cause “spontaneous” ICH in elderly
CECT
Enhancement patterns
Intense
Punctate
Nodular
Ring enhancement
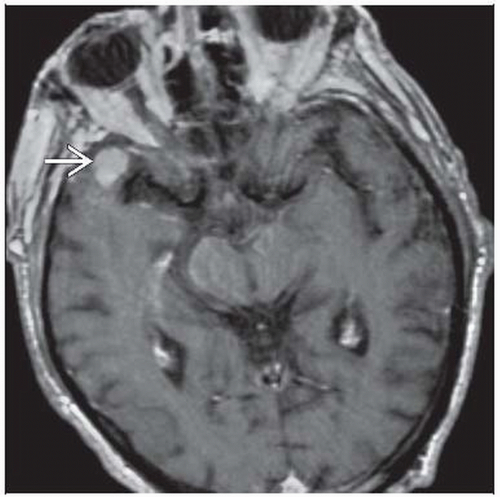
Metastases frequently multiple, seen at the junction of gray and white matter; usually with significant surrounding edema
On noncontrast CT, metastatic lesions may be of a density less than, equal to, or greater than adjacent brain parenchyma
Most of the patterns are variable and nondiagnostic
Noncontrast CT is performed to detect hemorrhage into metastases
Hyperdensity in a metastasis is more likely to be hemorrhage than calcification
Most metastases enhance after a standard dose of IV contrast
Detecting additional metastases has important diagnostic implications
If a solitary lesion is found on routine enhanced CT, an additional lesion may suggest a metastatic process
Particularly true in a patient with no known primary cancer (if the solitary lesion was believed to be a primary lesion)
Detection of an additional lesion may modify or change treatment
Contrast-enhanced CT is effective in detecting major leptomeningeal spread
Contrast-enhancing subdural or epidural metastases may be seen, usually secondary to calvarial lesions
Of breast, lung, prostate, and renal cell neoplasms, 5% metastasize to the calvarium and 15% of these extend into the subdural space
Multiple enhancing solid lesions at the gray-white matter junction and prominent surrounding edema
Can be diagnosed confidently as metastases in a patient with known primary cancer
≈ 90% of patients with a history of cancer who present with a single supratentorial lesion have brain metastases
Patients with multiple lesions are even more likely to have metastatic disease
Prior to definitive therapy, patients with a single metastasis by contrast-enhanced CT should undergo a contrasted MR examination
Contrast-enhanced CT is useful and perhaps the best method to identify calvarial metastases
≈ 20% of patients who demonstrate a single lesion on contrast-enhanced CT may demonstrate multiple lesions on contrast-enhanced MR
Lesions missed on CECT are mostly smaller (< 2 cm in diameter), located next to the bone, & in a frontotemporal location
Dural-based metastases may mimic meningioma
Nuclear Medicine Findings
PET
FDG PET
Activity in CNS metastases depends on tumor histology
Classically hypermetabolic on FDG PET: Lung, breast, colorectal, head and neck, melanoma, thyroid
Classically hypometabolic on FDG PET: Mucinous adenocarcinoma, renal cell carcinoma
Variable uptake on FDG PET: Gliomas, lymphoma
Central hypometabolism suggests necrosis
18-F choline allows differentiation among benign lesions, metastatic tumors, and high grade glial tumors
Metastatic lesions generally show significantly higher fluorocholine uptake than high grade gliomas
FDG PET sensitivity 79-82%, specificity 94% for detecting origin of primary
FDG PET detected few primaries not already detected in standard workup, including CXR or chest CT
Primary benefit: Detection of nodal involvement and extent of metastases to other regions for staging and therapeutic decisions
Uptake in low grade tumors is usually similar to normal white matter
In area of interest, any FDG uptake higher than expected background level in adjacent brain tissue should be considered recurrent tumor
Even if it is same or less than cortical uptake
Early studies showed 81-86% sensitivity and 40-94% specificity for distinguishing between radiation necrosis and tumor
Recurring tumor can occur along same time lines as necrosis
Optimal time for performing FDG PET after radiotherapy is not known
For purpose of evaluating tumor growth, at least 6 weeks should elapse prior to imaging
Discovery of extrathoracic metastases is contraindication for surgery except in specialized circumstances
e.g., solitary brain metastasis
Unsuspected brain metastases in patients with non-CNS cancer found in only 0.4% of patients who had already been worked up w/conventional imaging
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree