Melanoma
Todd M. Blodgett, MD
Alex Ryan, MD
Omar Almusa, MD
Key Facts
Terminology
Malignant melanoma (MM)
Imaging Findings
CT
CECT is better than FDG PET for detection of small pulmonary metastases
Less sensitive than FDG PET for bone, skin, lymph node, abdominal metastases
Combination of FDG PET and conventional imaging (CT/MR) more accurate than either one alone
CT generally performed for staging and restaging purposes
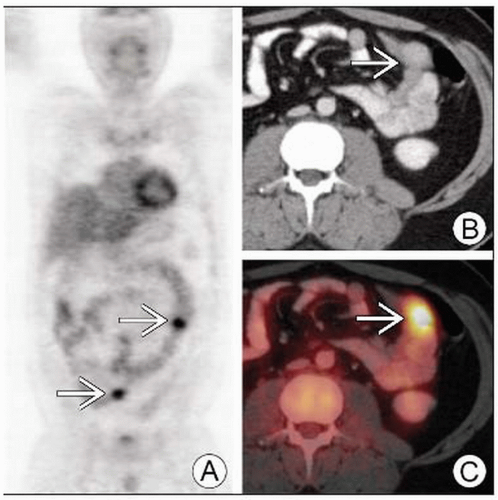
PET/CT
Detects more lesions than CT, particularly intramuscular and other unsuspected metastases
More exact method of determining FDG uptake in a mass
Staging: Sensitivity 83%, specificity 91%
Restaging: 74% sensitivity 74%, specificity 86% for recurrence
In one study, 16% of patients underwent further imaging &/or biopsies that ultimately had no effect on patient care
Top Differential Diagnoses
Other Neoplasms
Inflammation/Infection
Brown Fat
Clinical Issues
Tumor thickness = most important histologic prognostic indicator
TERMINOLOGY
Abbreviations and Synonyms
Malignant melanoma (MM)
Skin cancer
Definitions
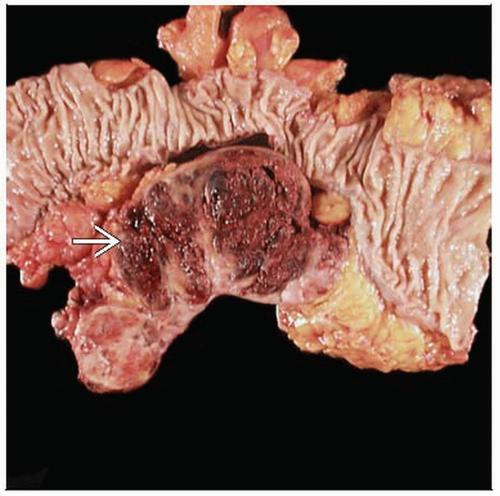
Melanoma: Neoplasm of melanin-producing cells
IMAGING FINDINGS
General Features
Best diagnostic clue: FDG-avid focal uptake on PET seen in primary, satellite lesions, lymph nodes (LN), visceral organs, and bone
Location
Primary melanoma
Men: Torso most common
Women: Upper extremities most common
4-5% of primary melanoma may arise in extracutaneous location
Locations include eye, meninges, mucous membranes of digestive, genitourinary, respiratory tracts
Multiple primaries occur in ˜ 5% of patients
Local spread
At or near previous excision site
Recent biopsy or other inflammation may produce false positive on FDG PET
Sentinal node tumor may alter stage
Metastatic disease
In-transit nodal metastases: Between primary and regional lymph nodes
Regional lymph nodes
Common sites: Spine, brain, lung, liver, spleen, bowel
Clinically apparent brain metastases found in 18-46% of patients with stage IV disease
Conjunctival melanoma may present with systemic metastases in 26% of cases without regional lymph node involvement
Size
Size considerations usually relative to depth of lesion
Stage is dependent on depth
Morphology: Malignant lymph nodes are typically round with absence of fatty hilum
Imaging Recommendations
Best imaging tool
FDG PET
May reveal focal increased uptake in lymph node bed, soft tissue, and organs
More sensitive than CT for skin, LN, bone, and abdominal metastases
CECT
Exclusion of benign structures with FDG uptake
Accurate delineation of primary and metastatic tumor in lymph node bed, soft tissue, and organs
Superior detection of small pulmonary metastases
Inclusion of lymph nodes by size or morphology (round without fatty hilum)
MR
For definition of brain metastases
Protocol advice
FDG PET
Evaluate skin for lesions with non-attenuation corrected PET images
Attenuation correction can smooth data, obscuring lesions
PET scan often extended to true whole-body coverage due to metastatic behavior of melanoma
Clinical history crucial: False positives with recent surgery, biopsy, inflammation
Total lesion glycolysis (TLG) approach
More exact method of determining FDG uptake in a mass
Has failed to show superiority over simpler SUV measurement
Longer FDG uptake times may correlate to better overall sensitivity/specificity
In general, more uptake in malignant lesions and less uptake in benign lesions is seen at 2 or 3 hour time point
CT Findings
CT generally performed for staging and restaging purposes
Not used to evaluate primary lesions
NECT: Less sensitive for detecting metastatic lesions than CECT
CECT: More sensitive for evaluation of organs and non-nodal soft tissue such as muscle
General
After typical search pattern, look again at muscle, gallbladder, and other subcutaneous soft tissues
Brain
Imaging performed for patients with known metastatic disease
Also performed for patients with neurological symptoms in the absence of known metastases
MR with contrast much more sensitive for detecting small brain metastases
Chest
May detect asymptomatic lesions
NECT and CECT approximately equal for detecting small pulmonary metastases
FDG PET less sensitive in general for detecting lung metastases ≤ 6 mm
Abdomen
Organ metastases may show hyperenhancement
Intramuscular metastases will generally show some abnormal enhancement, but may be otherwise undetectable
Pelvis
More likely positive in patients with primary disease below waist
Bone
Some may demonstrate enhancement, making them more conspicuous
Extensive bone metastasis may be missed altogether
Nuclear Medicine Findings
General
Melanoma is almost always FDG avid
True positives have significantly higher SUV than false positives in lesions > 1 cm on PET/CT
PET/CT has considerable but non-significant advantage over PET in characterization of lesions
Possibly due to high avidity of melanoma metastases
Certainty of lesion localization significantly improved with combined modality
Especially in detection of visceral metastases
Accuracy of PET/CT higher when equivocal lesions are considered negative
PET/CT recommended for stage III/IV patients
Thorough physical exam and US of draining nodes for lower stage patients
PET/CT may detect unheralded occult primary malignancy in patients with primary melanoma
Choroidal melanoma reported to have low FDG uptake
Correlated strongly to lesion size
Intra-operative FDG PET/CT
Handheld gamma probe used to find lesions during surgery
Used to verify intra-operative US findings
Used to verify excised tissue as being the FDG-avid lesion
Can evaluate residual sites of hypermetabolic activity immediately post-operatively
Staging
PET established as useful modality for staging and restaging of cutaneous melanoma and for evaluating distant metastases
Large meta-analysis: Sensitivity 83% and specificity 91% for staging
Changes management in 26-50% of patients
In one study, 16% of patients underwent further imaging &/or biopsies that ultimately had no effect on patient care
Local or early disease
PET/CT found to have high accuracy for evaluation of regional metastases
Sensitivity 23% if metastases ≤ 5 mm (e.g., small lung nodules)
One study concluded that PET reliably detects lymph node tumor deposits > 80 mm3
Loses sensitivity rapidly below that volume
Not reimbursable by Medicare for evaluation of regional lymph nodes in stage I/II disease
More sensitive in setting of clinical or radiographic evidence of disease
Distant disease
Sensitivity ≥ 90% for lesions > 1 cm
Reimbursable by Medicare for evaluation of extranodal metastases during initial staging
Sensitivity of 60% with FDG PET for brain metastases due to high physiologic uptake in the brain
Organ-based accuracy in liver, lung, and brain variable
Accuracy of PET/CT for M-staging higher than that of PET or CT alone (98%, 93%, 84%, respectively)
Superior sensitivity for lung metastases compared to MR
PET/CT of node positive melanoma at time of sentinal lymphadenectomy had management change in 31% of one patient cohort
CT/MR in this circumstance shown to yield less than 1%; not clinically indicated
Level of uptake in lymph node metastases correlates with recurrence risk
Restaging
FDG PET detects recurrent disease with sensitivity/specificity 74%/86%
Elevated laboratory markers or clinical evidence of recurrence should prompt re-imaging
Pre-surgical evaluation may detect more extensive disease and alter surgical planning
FDG PET reimbursed by Medicare for pre-surgical evaluation of recurrence
Response to therapy
PET/CT not routinely performed
Likely will play a more significant role in evaluating patients after various immunomodulating therapies
One study showed complete agreement differentiating chemo-responders and nonresponders between CT and PET/CT
Baseline FDG PET very helpful for evaluating response to therapy
Melanoma differs from malignancies such as lymphoma, in which metabolic changes precede morphologic changes
PET/CT has benefit of relative ease of interpretation, but some controversy exists as to cost/benefit ratio
FDG PET pitfall: Cytokine therapy results in diffuse hypermetabolism in normal lymph nodes for months
MR Findings
More accurate in detection of mets to liver and bone
Hepatic metastases ≤ 1 cm and containing melanin have bright signal on T1 weighted MR
DIFFERENTIAL DIAGNOSIS
Other Neoplasms
May appear similar to melanoma in FDG avidity
If suspicion of melanoma recurrence is low, consider
Primary or metastatic disease from second primary
Unheralded second primary malignancies detected in 1.2% of patients (lung most common)
Squamous or basal cell carcinoma
Lymphoma in the presence of lymphadenopathy
Reactive Lymph Nodes
Look for CT evidence of other causes of reactive lymphadenopathy, e.g., colitis, pancreatitis, pneumonia
Inflammation/Infection
Pneumonia
May present with focal FDG uptake that mimics hypermetabolic nodule
CT correlation and follow-up studies are helpful to avoid unnecessary biopsy
Granulomatous infection may manifest as enlarged, hypermetabolic lymph nodes
Mycobacterium avium intracellulare
Tuberculosis
Sarcoidosis
Histoplasmosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree