Head And Neck Cancer, Squamous
Todd M. Blodgett, MD
Alex Ryan, MD
Marios Papachristou, MD
Key Facts
Terminology
Squamous cell carcinoma of the head and neck (SCCHN), squamous cell carcinoma (SCCA) nodes
Imaging Findings
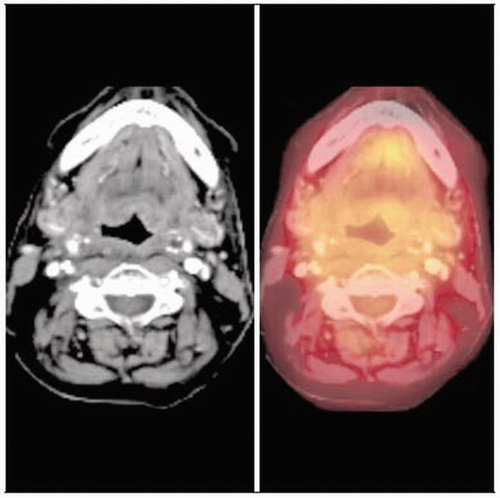
Intensely FDG-avid nodes in the neck on PET or PET/CT
Enlarged or necrotic lymph nodes in the neck ± enhancement on CT
PET/CT key for several clinical scenarios
Delineate extent of regional lymph node involvement
Detect distant metastases
Identify unknown primary tumor
Detect occasional synchronous primary
Combined PET/CT may offer additional localization information and improve interpreting physician’s confidence level
Overall sensitivity and specificity of FDG PET and PET/CT > 90%; PET/CT sensitivity 96% and specificity 98%
Top Differential Diagnoses
Abscess or Suppurative Nodes
Lymphoma
Physiologic Activity
Reactive Nodes
Diagnostic Checklist
Consider PET/CT in patients with primary tumors that are prone to bilateral metastases, which are often less conspicuous on conventional imaging
TERMINOLOGY
Abbreviations and Synonyms
Squamous cell carcinoma of the head and neck (SCCHN)
Squamous cell carcinoma (SCCA) nodes
Unknown mucosal primary
Therapeutic assessment/restaging
Definitions
Primary, regional, and distant malignancy from tumors of squamous cell origin in the head and neck
Primary unknown: Metastatic squamous cell carcinoma of the neck without an identifiable mucosal primary lesion
Undetectable mucosal lesions by clinical exam or
Negative anatomical imaging
Head and neck cancers include those arising from the lip, oral cavity, nasal cavity, paranasal sinuses, pharynx, and larynx
90-95% are squamous cell carcinomas arising from mucosal linings of upper aerodigestive tract
IMAGING FINDINGS
General Features
Best diagnostic clue
Intensely FDG-avid nodes in the neck on PET or PET/CT
Enlarged or necrotic lymph nodes in the neck ± enhancement on CT
Primary unknown
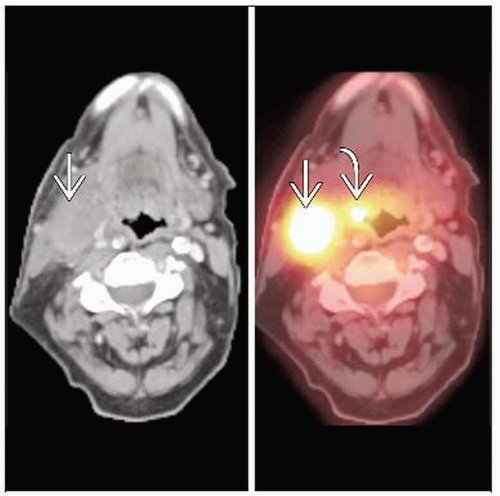
PET shows asymmetrical focal fluorodeoxyglucose (FDG) uptake, with or without an identifiable abnormality on CT
Sensitivity for PET and PET/CT is 26-43% in cases where primary has eluded diagnosis
Fused PET/CT images often helpful for determining whether potential FDG abnormalities are mucosal lesions
Helpful for directing clinicians to areas for directed biopsies
Intense FDG activity in or around treated primary tumor with corresponding CT evidence of residual tumor
Location
Primary squamous cell lesions may involve any mucosal surface
Commonly involve the base of tongue, tonsils, or adenoids
Mucosal surfaces of the oropharynx, nasopharynx, and hypopharynx
Lymph node metastases involve neck nodes in expected drainage pattern based on primary tumor
SCCHN has high propensity to harbor malignancy in small lymph nodes
Most common metastatic sites: Lung, liver, skeletal system
Size
Early primary SCCHN may be undetectable (unknown primary SCCHN)
Lymph node metastases may range in size from normal (< 1 cm) to several centimeters
Morphology
Mass effect, abnormal enhancement, or necrosis may exist in larger tumors
Fatty lymph node hilum usually denotes benign lesion on CT (may be positive on PET if occult malignancy present)
Indistinct borders usually denote extranodal spread
Imaging Recommendations
Best imaging tool
PET/CT key for several clinical scenarios
Delineate extent of regional lymph node involvement
Detect distant metastases
Further evaluate potentially abnormal findings on another exam, such as mediastinal adenopathy detected by chest CT
Identify unknown primary tumor
Detect occasional synchronous primary
Monitor treatment response to select appropriate patients for salvage surgery
Conduct long-term surveillance for recurrence and metastases
Check any patient who presents with clinical evidence of recurrent disease
TNM staging
MR better than CT for specific questions such as presence of perineural spread or invasion of bone marrow
N stage
CT generally superior to MR for detection of regional lymph node metastases
M stage
Only patients at substantial risk of nodal or hematogenous metastases, T3 or T4, should undergo routine PET/CT for staging
Combined PET/CT may offer additional localization information and improve interpreting physician’s confidence level
Overall sensitivity and specificity of FDG PET and PET/CT > 90%; PET/CT sensitivity 96% and specificity 98%
PET/CT more helpful for radiation therapy planning; can lead to changes in gross tumor volume
Extended field FDG PET staging may detect disease outside of the head and neck in up to 21% of patients with head and neck cancer
Sensitivity for PET and PET/CT 26-43% in which primary has eluded diagnosis
Sensitivity for PET/CT better for accurate localization of lesion and directed biopsy recommendations
MR typically initial imaging study of choice for staging
Compared to noncontrast PET/CT, more accurate delineation of tumor extent, perineural involvement, and intracranial extent
Nearly comparable in accuracy in detecting regional LN metastases
Contrast-enhanced CT used only in laryngeal cancer; PET/CECT may be better for this indication than MR or CECT alone
Restaging: Combined PET/CT is more sensitive and specific than CT alone
Protocol advice
High resolution PET/CT from top of head to carina using standard head and neck protocol (especially for unknown primary)
Scan with arms down on PET/CT to avoid beam hardening artifact
Whole-body scan performed with arms above head and shorter acquisition time
Use neck immobilization device
Scan in mask for radiation planning PET/CT
Display images with PET intensity kept low-moderate (avoid “blooming”)
Pre-treatment with benzodiazepines in patients with excessive muscular FDG uptake on FDG PET
Warm patients before and after injection of FDG to reduce brown fat FDG uptake
Restaging
Scan with arms down, CECT, and neck immobilization device
Consider dual-time point imaging to help differentiate between inflammatory and neoplastic FDG activity
CT Findings
CECT: Early enhancement, rim enhancement, central necrosis, indistinct borders
Post-therapy neck difficult to interpret
Accuracy of CT ranges from 50-70%
Loss of fat planes and extensive post-surgical changes reduce the specificity of CT
Distortion of normal anatomy can be due to bony-cartilaginous necrosis, edema, and desmoplastic changes
CT may show enhancement, necrosis, or mass effect with residual/recurrent tumor
Best method of detection using CECT is serial examination
CT and MR may be negative for unknown primary if
Tumor is subtle or difficult to separate from adjacent normal structures (as with lingual tonsillar tissue)
Primary is superficial or very small
Scan is limited by motion or streak artifact
Abnormal size criteria for CT: ≥ 1 cm for most nodes; ≥ 1.5 cm for level I-II nodes; ≥ 8 mm for retropharyngeal nodes
FDG PET can detect smaller positive nodes (limited by spatial resolution)
Central necrosis specific for malignancy, but it is a late marker of metastatic adenopathy
Usually seen only in nodes ≥ 20 mm, which is beyond the typical cutoff of 10 mm for suspicion of malignancy
Contrast enhancement generally improves detection of malignancy
Round morphology more suspicious than reniform
Nuclear Medicine Findings
PET/CT is more accurate than PET and CT separately; PET is more accurate than CT alone
FDG PET sensitivity and specificity for residual disease 90% and 83%, respectively
PET/CT sensitivity, specificity, and accuracy 98%, 92%, and 94%, respectively
PET/CT decreases number of equivocal lesions by ˜ 50% and provides improved biopsy localization information
74% better localization with PET/CT compared to PET in regions previously treated; 58% for untreated regions
Initial diagnosis
Squamous cell carcinoma almost always FDG avid
Look for primary lesion along the mucosal surfaces
Unknown primary: FDG PET typically shows focal asymmetrical FDG uptake in the mucosal primary
5-10% of cases involve primary that cannot be found by physical exam, panendoscopy, or conventional radiographic imaging
PET/CT has been shown to find primary in 40% of patients whose primary was not identified in office or with surgical panendoscopy
False negatives with PET/CT means that this modality is a supplement to, but not a substitute for, endoscopy and biopsy with unknown primary
FDG PET shows no advantage over traditional techniques for identification and characterization of primary head/neck tumors for stage I/II lesions
Rarely adds information regarding initial T staging of primary
Exception is unknown primary
Staging
Screening for distant metastases advised for patients who have
Four or more lymph node metastases
Bilateral positive nodes
Nodes greater than 6 cm
Zone 4 nodes
Recurrent SCCHN
Second primary tumor
In one study, 24% of patients newly diagnosed with SCCA of the oral cavity had distant metastases picked up by PET/CT
However, PET/CT cannot preclude neck dissection in patients with advanced primaries but clinically node-negative necks
PET/CT may alter TNM score in 30-35% of patients by identifying nodal disease not apparent on CT, MR, or clinical exam
PET/CT has advantage in identifying distant disease because it can detect occult metastatic disease (e.g., subtle bone metastases)
Present in as many as 10% of patients with advanced local-regional disease
PET may alter treatment in many patients, decreasing toxic wide-field radiotherapy
Unclear whether PET/CT useful in identification of nodal metastases in patients with SCCHN and N0 necks on exam
Stage III/IV patients have high risk of distant metastases, creating a greater role for FDG PET
PET has a distinct advantage over CT/bronchoscopy, especially in the lung
Target volumes for IMRT and stereotactic radiosurgery may be modified in as many as 20% of cases with PET/CT vs. CT alone
PET/CT used primarily to include normal-sized lymph nodes with increased metabolic activity as part of high dose target volume
Helpful for contouring primary tumors whose borders are difficult to distinguish by anatomic imaging alone, as with some tongue-based tumors
PET/CT limited in staging local lymph node involvement if patient’s disease is clinically stage N0 after physical examination and anatomic imaging
Due to limited spatial resolution
Selective neck dissection or sentinal lymph node biopsy is more definitive
However, even in stage N0 disease PET/CT may be useful
Serves as a baseline to differentiate incidental physiologic FDG-avid foci from malignant foci on subsequent post-treatment exams
Otherwise a significant interpretive challenge if comparison images are not available
Restaging
Following surgery, no detectable tumor should be present
Variable amounts of post-surgical change expected
Post-surgery: Usually wait 4-6 weeks after to reevaluate with PET and PET/CT to avoid false positive studies due to inflammation
Reevaluation following surgery may be particularly helpful in cases where surgical margins are positive
Post-radiation
Positive PET one month after XRT has a positive predictive value of ˜ 100%
Negative PET one month after XRT has a lower negative predictive value (14%) early; fewer false negatives with longer follow-up period
Response to therapy
Following chemoradiation, metabolic response may precede reductions in tumor volume
Post-chemotherapy (approximately 1 month after completion): Sensitivity and specificity of FDG PET 90% and 83%
Little data evaluating early response to chemotherapy
Inflammatory changes seen with radiotherapy are not seen, and PET can be performed at earlier time point, such as 4-8 weeks
Post-chemoradiation
PET/CT has high negative predictive value and allows confident exclusion of residual cancer, thereby deferring planned neck dissection
Pitfalls and limitations
Several structures in the neck with variable physiologic FDG activity
Common muscles with asymmetrical FDG activity: Pterygoids, sternocleidomastoid, strap muscles, and mylohyoid
Glands: Salivary glands (submandibular and parotid); can have intense FDG activity following some chemo regimens
Lymphoid tissue: Lingual tonsils, palatine tonsils, and adenoids (Waldeyer ring)
Brown fat: Can be symmetrical or asymmetrical, can be focal anywhere in the neck
FDG PET may not detect small areas of residual/recurrent disease, leading to early false negative exams after therapy
PET frequently fails to identify hypermetabolism in areas of marrow space infiltration and perineural extension
Cartilage necrosis may be FDG avid indefinitely
Cricoarytenoids typically FDG avid and often asymmetric
DIFFERENTIAL DIAGNOSIS
Metastatic Disease from Thyroid or Melanoma
May look identical to squamous cell carcinoma
Abscess or Suppurative Nodes
Usually has central necrosis; identical in appearance to necrotic lymph node
FDG PET not helpful for differentiation; biopsy required
Often indistinguishable from tumor; correlate clinically
Lymphoma
Difficult to differentiate from SCCHN based on imaging; associated mucosal lesion favors SCCHN
NHL: May mimic tonsillar inflammatory disease
Residual/Recurrent Malignancy
Often indistinguishable from abscess/inflammation
Short-term serial evaluation very helpful
CT may show asymmetrical mass effect
Radiation-Induced Inflammation
FDG uptake from inflammation usually present for 4-8 weeks following therapy
Osteoradionecrosis can cause false positive early (before frank necrosis causes negative PET)
Dual-time point PET imaging at 1 hour and 3 hour post FDG injection may be helpful in differentiating tumor vs. inflammation
FDG uptake from 1-3 hours: Tumor may increase; inflammation may plateau or decrease
Physiologic Activity
Benign tonsil FDG uptake typically will be symmetrical but can be intense
Muscle activity may be focal and asymmetrical
Correlate PET with CT; pre-treatment with benzodiazepines may reduce muscle uptake
Measure Hounsfield units (HU); -50 to -150 compatible with brown fat
Warm patient before FDG injection to reduce brown fat uptake of FDG
PATHOLOGY
General Features
General path comments
Nodal level classification scheme
American Joint Committee on Cancer (AJCC) and American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS)
Level IA: Submental nodes between anterior digastrics
Level IB: Submandibular, lateral to IA anterior to the posterior margin of submandibular gland (SMG)
Level IIA: Upper internal jugular nodes; anterior, lateral, or posterior and touching the jugular vein
Level IIB: Posterior, not touching jugular
Level III: Mid-internal jugular nodes, extend from inferior hyoid to cricoid arch
Level IV: Low internal jugular nodes, extend from cricoid arch to the level of the clavicle
Level V: Spinal accessory group, nodes in the posterior triangle; level VA: Above cricoid; level VB: Below inferior cricoid border
Level VI: Upper visceral nodes; between the carotid arteries from bottom of the hyoid to the top of the manubrium
Level VII: Superior mediastinal nodes; between the carotid arteries from below the top of the manubrium above the innominate vein
Supraclavicular nodes: At or caudal to the level of the clavicle and lateral to the carotid artery
Retropharyngeal nodes: Within 2 cm of the skull base medial to the carotid arteries
Parotid: Nodes within the parotid gland
Initial workup with physical exam, office endoscopy, and MR/CT
If definitive for nodal disease, PET/CT is appropriate for accurate evaluation of nodal metastases
Suggestive PET/CT findings should prompt fine needle aspiration (FNA)
If FNA is negative, definitive treatment is pursued and PET/CT is optional, to serve as baseline prior to therapy
If a focus of unknown primary is suspected on metabolic imaging
Panendoscopy and frozen section biopsy
Panendoscopy includes oropharynx, hypopharynx, nasopharynx, larynx, and upper esophagus
If negative, further biopsy specimens may be obtained from most common sites for primary tumors
Base of tongue
Nasopharynx
Contralateral tonsillar fossa
Pyriform sinus
Ipsilateral tonsillar fossa
Reassessment
Biopsy areas that appear suspicious on PET or PET/CT
Alternatively, short-term interval follow-up PET or PET/CT
Etiology: Smoking, chewing tobacco, alcohol abuse
Epidemiology
SCCHN newly diagnosed in 40,000 patients annually in United States
Mortality is 23%
Average 5 year survival 56%
Associated abnormalities: Risk factors also predispose to esophageal and lung cancer
Staging, Grading, or Classification Criteria
T stage: Assessment requires knowledge of size of primary lesions, depth of invasion, and involvement of surrounding structures
N stage: AJCC characteristics include number of nodes involved, size of nodes, location (laterality and level), and morphology
Staging of SCCHN requires
Complete history and physical
Histologic confirmation
Characterization of primary
Recognition of local/regional nodal disease
Identification of distant metastatic disease
CLINICAL ISSUES
Presentation
Most common signs/symptoms
May present with pain associated with primary mass or neck mass
Symptoms of residual/recurrent tumor overlap with post-treatment complications; pain is most common
Other signs/symptoms: Mass on clinical exam
Demographics
Age: Generally > 40-45 years
Gender: M > F
Natural History & Prognosis
Nodal metastasis is most accurate prognostic factor for SCCHN
Unilateral nodal involvement indicates 50% reduction in expected lifespan; bilateral nodal involvement indicates 75% reduction
10 year survival drops from 85% to 10-40% in patients with positive nodes
Carotid artery involvement or encasement portends dismal prognosis with 100% mortality
Majority of patients do not have metastatic disease within cervical nodes at presentation
20% risk of occult metastasis in patients with clinically node-negative necks
10-15% of patients with SCCHN will present with distant metastases
Unknown primary
PET and PET/CT can help direct biopsy
2-9% of SCCHN patients present with cervical lymph node metastases without clear evidence of primary site
If imaging is negative, patients are usually followed with serial imaging evaluation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree