Brain Metastases
 BACKGROUND
BACKGROUND
What is the most common intracranial tumor?
Brain met is the most common intracranial tumor (outnumber primary brain tumors 8:1).
What is the annual incidence of brain mets in the U.S.?
170,000–200,000 cases/yr of brain mets in the U.S., with development in up to 30% of pts with systemic cancer
Why is the incidence of brain mets increasing?
The incidence is increasing due to advancements in systemic therapy (improved extracranial control) with limited penetration of the blood–brain barrier in conjunction with increased utilization of MRI/surveillance imaging.
What cancers are associated with hemorrhagic brain mets?
Hemorrhagic brain mets is associated with melanoma, renal cell carcinoma, and choriocarcinoma.
What do the terms solitary and single brain met connote?
A solitary brain met is only 1 brain lesion and the only site of Dz. A single brain met is only 1 brain lesion in addition to other sites of met Dz.
What cancers are most likely to metastasize to the brain?
Cancers associated with brain mets: lung (40%–50%), breast (15%), melanoma (10%)
In what % of pts are brain mets the 1st manifestation of Dz?
5%–20% of pts present with brain mets from an unknown primary. Pts presenting with brain mets without a prior Dx of cancer most often have a lung primary.
Should Bx or resection be recommended if a new Dx of brain mets is suspected?
Yes. Bx should be considered in pts with a new Dx of brain mets as 11% of pts (6/54) enrolled in the 1st Patchell trial were found to have a primary brain tumor (3 pts) or inflammatory/infectious process (3 pts) despite MRI or CT findings consistent with metastatic Dz. (Patchell R et al., NEJM 1990)
What is the more common type of brain mets: single or multiple?
Most pts have multiple brain mets rather than a single lesion, with increased detection of small, multifocal lesions on MRI typically not appreciated on CT.
How do pts with brain mets present?
Presentation of pts with brain mets: Sx of ↑ ICP (HA, n/v), weakness, change in sensation, mental status changes, and seizure
What is carcinomatous meningitis?
Carcinomatous meningitis is a clinical syndrome caused by leptomeningeal met with widespread involvement of the cerebral cortex. The Dx is associated with a poor prognosis.
Where do most brain mets occur?
Most brain mets arise in the gray/white matter junction due to hematogenous dissemination with narrowing of blood vessels. (Delattre J et al., Arch Neurol 1988)
Are most brain mets infra- or supratentorial?
The majority of brain mets are supratentorial.
What is the distribution of brain mets within the brain?
The distribution of brain mets correlates with relative weight and blood flow:
Cerebral hemispheres: 80%
Cerebellum: 15%
Brainstem: 5%
(Delattre J et al., Arch Neurol 1988)
What is the overall median time from initial cancer Dx to development of brain mets?
The median overall time from initial cancer Dx to development of brain mets is 1 yr.
Do most pts with brain mets die from their CNS Dz?
No. ∼30%–50% of pts with brain mets die from their CNS Dz.
 WORKUP/STAGING
WORKUP/STAGING
Describe the workup of a brain met.
Brain met workup: H&P focus on characterization of any neurologic Sx, evaluation for infectious causes (fever, CBC), careful neurologic exam, MRI brain +/– gadolinium, assessment for status of extracranial Dz, determination of Karnofsky performance status (KPS), and neurosurgery consult
What is the DDx for a new lesion in the brain?
Brain lesion DDx: mets, infection/abscess, hemorrhage, primary brain tumor, infarct, tumefactive demyelinating lesion, and RT necrosis
What imaging features are suggestive of brain mets?
Imaging features suggestive of brain mets include lesions at gray/white matter junction, multiple lesions, ring-enhancing lesions, and significant vasogenic edema
What is triple-dose gadolinium, and why is it used?
Triple-dose gadolinium: 0.3 mmol/kg. It is used to increase the sensitivity of MRI.
 TREATMENT/PROGNOSIS
TREATMENT/PROGNOSIS
Describe the RTOG recursive partitioning analysis (RPA) classes for brain mets. (Gaspar L et al., IJROBP 1997)
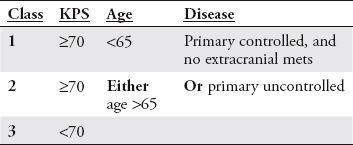
KPS, Karnofsky performance score.
What is the MS time for RTOG RPA classes I, II, and III?
MS according to the RTOG brain met RPA:
Class I: 7.2 mos
Class II: 4.2 mos
Class III: 2.3 mos
What is the Sperduto Index?
The Sperduto Index is a graded prognostic assessment based on age, KPS, # of brain mets, and the presence or absence of extracranial mets developed from an analysis of 1,960 pts in the RTOG database. Criteria is based on a point system:
0 points: age >60 yrs, KPS <70, >3 brain mets, presence of extracranial mets
0.5 points: age 50–59 yrs, KPS 70–80, 2 CNS mets
1 point: age <50 yrs, KPS 90–100, 1 CNS met, no extracranial mets
The sum of points predicts MS in mos:
0–1 point: 2.6 mos
1.5–2.5 points: 3.8 mos
3 points: 6.9 mos
3.5–4 points: 11 mos
(Sperduto P et al., IJROBP 2007)
What is the Diagnosis Specific Graded Prognostic Assessment (DS-GPA)?
The DS-GPA is a graded prognostic assessment developed from a retrospective database of 4,259 eligible pts from 11 institutions with determination of significant prognostic factors based on the primary histology. (Sperduto P et al., IJROBP 2010)
What are the significant prognostic factors?
The significant prognostic factors vary by Dx:
Non-small cell lung cancer (NSCLC)/small cell lung cancer: age, KPS, presence of extracranial mets and number of brain mets
Renal cell/melanoma: KPS and the number of brain mets
Breast/GI: KPS
In pts with untreated brain mets, what is the MS?
MS of untreated brain mets is 1 mo.
What Tx may be used for brain mets?
Brain met Tx: steroids, surgery, fractionated RT (WBRT), and SRS
In pts with brain mets treated with steroids alone, what is the MS?
MS in pts with brain mets treated with steroids alone is 2 mos.
Are there randomized data to support improvement in pt survival or QOL with the addition of WBRT to best supportive care?
No. The ongoing MRC Quartz trial is a randomized, noninferiority phase III trial investigating the role of optimal supportive care (OSC) + WBRT (4 Gy × 5 fx) vs. OSC alone in pts with inoperable brain mets from NSCLC. The primary outcome measure is quality-adjusted life yrs.
How are steroids for brain mets typically prescribed?
Steroid dose for newly diagnosed brain mets: 4 mg dexamethasone q6hrs; may give initial loading dose of 10 mg.
Why are steroids used for symptomatic brain mets?
In pts with symptomatic brain mets, steroids reduce leakage from tumor vessels, therefore decreasing edema and mass effect.
What pharmacologic Tx should always accompany steroid Tx?
When prescribing steroids, also provide GI prophylaxis with a proton-pump inhibitor or H2 blocker.
Should anticonvulsants be used prophylactically?
No. In accordance with guidelines from the American Academy of Neurology, pts with newly diagnosed brain tumors should not be started on prophylactic anticonvulsants. (Glantz M et al., Neurology 2000) The 2010 guidelines from the American Association of Neurological Surgeons/Congress of Neurological Surgeons do not recommend routine prophylactic use of anticonvulsants. (Mikkelsen T et al., J Neurooncol 2010)
Are there any randomized data on the dose for WBRT?
Yes. The RTOG conducted several RCTs from 1970–1995 of WBRT alone, assessing different fractionation schemes. The 1st 2 trials (RTOG 6901 and 7361) included >1,800 pts randomized to 40 Gy/20, 40 Gy/15, 30 Gy/15, 30 Gy/10, or 20 Gy/5. No significant difference was found in response rates, length of response, or OS. The MS in the 1st study was 4.1 mos and 3.4 mos in the 2nd. (Borgelt B et al., IJROBP 1980)
2 ultrarapid fractionation schemes were also tested on these studies and reported separately; 10 Gy/1 (RTOG 6901) and 12 Gy/2 (RTOG 7361) in 26 and 33 pts, respectively. These schedules were associated with worse toxicity and time to neurologic progression than the standard fractionation. (Borgelt B et al., IJROBP 1981)
2 studies showed no MS advantage to giving a higher total dose. RTOG 7606 randomized 255 pts to 30 Gy/10 vs. 50 Gy/20. MS was 4.1 and 3.9 mos, respectively. (Kurtz J et al., IJROBP 1981) RTOG 9104 randomized 429 pts to 30 Gy/10 vs. 54.4/1.6 Gy bid. MS was 4.5 mos in both arms. (Murray K et al., IJROBP 1997)
What dose and fractionation schemes are considered standard for WBRT?
The most standard WBRT dose is 30 Gy/10. Pts with a good KPS and longer life expectancy may be treated to 37.5 Gy/15, 40 Gy/20, or 50 Gy/20.
What % of brain met pts have Sx improvement with WBRT?
WBRT improves Sx from brain mets in ~60% of cases.
What is the rate of CR to WBRT for brain mets?
~25% of pts have a CR to WBRT for brain mets.
What data support surgery + RT rather than Bx + RT for brain mets?
The 1st Patchell study for brain mets randomized 48 pts with 1 brain met and KPS ≥70 to surgery + WBRT vs. Bx + WBRT. WBRT in both arms was 36 Gy in 3 Gy/fx. Pts treated with surgery had a longer MS (40 wks vs. 15 wks, p <0.01), longer functional independence (38 wks vs. 8 wks), and ↓LR (20% vs. 52%, p <0.02). (Patchell R et al., NEJM 1990)
Did the Netherlands trial of WBRT +/- surgery support or refute the Patchell study?
The Noordijk study supported the findings of the 1st Patchell study. It randomized 63 pts to WBRT alone or surgery + WBRT. WBRT was 40 Gy in 2 Gy bid fx. Pts treated with surgery had improved MS (10 mos vs. 6 mos, p = 0.04) and longer functional independence (7.5 mos vs. 3.5 mos, p = 0.06). (Noordijk E et at., IJROBP 1994)
Does adj WBRT after surgical resection of a brain met improve OS?
No. Postop WBRT following resection of a brain met does not improve survival. In the 2nd Patchell study for brain mets, 95 pts following surgical resection of a single met were randomized to no further Tx or WBRT (50.4 Gy in 1.8 Gy/fx). WBRT decreased LR (10% vs. 46%), decreased the rate of any brain failure (18% vs. 70%), and decreased the rate of neurologic death (14% vs. 44%) but did not significantly change MS (48 wks vs. 43 wks). (Patchell R et al., JAMA 1998)
Why did the investigators choose a nonstandard WBRT dose?
The dose and fractionation schedule were chosen to achieve 90% microscopic Dz control probability.
What are the indications for surgical resection?
Single lesion amenable to resection, controlled or absent extracranial Dz, KPS >70, age <60 yo, life expectancy >2 mos, need for immediate relief of neurologic symptoms secondary to mass effect, need to establish a tissue Dx.
Are there any current randomized studies that support the role of adjuvant WBRT?
Yes. EORTC 22952 enrolled 359 pts with 1–3 brain mets s/p surgery or SRS randomized to no further Tx vs. WBRT (30 Gy in 3 Gy/fx). Adjuvant WBRT reduced the 2-yr relapse rate both at initial sites (surgery: 59% to 27%; SRS: 31% to 19%) and new sites (surgery: 42% to 23%; SRS: 48% to 33%) with decreased rates of death secondary to intracranial progression (44% vs. 28%) without improvement in the duration of functional independence or OS. Pts randomized to observation were more likely to require salvage therapy (51% vs. 16%). (Kocher M et al., JCO 2010)
What is the rationale for SRS in the Tx of brain mets?
Spherical/pseudospherical target, generally noninfiltrative lesions (<3–4 cm) located along the gray–white junction (noneloquent regions), ability to deliver a higher dose than can be achieved with WBRT alone (improved LC), Tx of unresectable lesions.
What was the 1st RCT study of WBRT +/- an SRS boost?
The 1st RCT of WBRT +/– an SRS boost was conducted at the University of Pittsburgh. 27 pts with KPS ≥70 and 2–4 mets ≤2.5 cm that were at least 5 mm from the chiasm were randomized to WBRT (30 Gy/12 fx) +/– a 16-Gy boost. The trial closed early b/c of significant difference in brain control. The SRS arm had a longer time to LF (36 mos vs. 6 mos, p = 0.0005) and longer time to any brain failure (34 mos vs. 5 mos, p = 0.002) but no difference in OS (11 mos vs. 7.5 mos, p = 0.11). (Kondziolka D et al., IJROBP 1999)
According to RTOG 9508, which pts had a survival advantage with the addition of an SRS boost to WBRT?
RTOG 9508 randomized 331 pts with 1–3 brain mets to WBRT + SRS boost vs. WBRT alone. WBRT on both arms was 37.5 Gy in 2.5 Gy/fx. The SRS boost dose was dependent on size in accordance with RTOG 9005. On univariate analysis, the addition of SRS improved the MS for pts with a single brain met (6.5 mos vs. 4.9 mos, p = 0.39). On subgroup multivariate analysis (MVA), RPA class I pts had improved survival with the SRS boost, as did pts with a lung cancer primary. (Andrews D et al., Lancet 2004)
What is the main determinant in selecting the Rx dose for SRS Tx of a brain mets?
The SRS Rx dose for a brain met is determined by size in accordance with the results of RTOG 9005, a dose escalation study: 24 Gy if <2-cm diameter, 18 Gy if 2–3 cm, and 15 Gy if 3–4 cm. (Shaw H et al., IJROBP 1996)
In the RTOG SRS dose escalation study, did pts rcv WBRT?
Yes. In RTOG 9005, an SRS dose escalation study, 64% of pts had recurrent brain mets (median prior dose of fractionated radiation 30 Gy) while 36% of pts had recurrent primary brain tumors (median initial dose of 60 Gy).
What retrospective data support the omission of upfront WBRT in pts treated with SRS for brain mets?
Sneed et al. compiled a database from 10 U.S. institutions to assess the effect of omitting upfront WBRT in pts treated with SRS for brain mets. 983 pts were analyzed and excluded pts treated with surgery (159 pts) and pts with a >1-mo interval between WBRT and SRS (179 pts). Of 569 evaluable pts, 268 had SRS alone and 301 had upfront WBRT + SRS. When adjusted for RPA class, there was no difference in survival. 37% of pts Tx with SRS alone rcvd salvage therapy (median 5.7 mos) vs. 7% of pts Tx with RS + WBRT (median 8.0 mos). No local control data were provided. (IJROBP 2002)
What data argue against omission of WBRT following SRS alone?
Regine et al. retrospectively analyzed 36 pts Tx with planned observation following SRS alone (median dose 20 Gy). With a MS of 9 mos, brain tumor recurrence occurred in 47% (17/16 pts) with 71% symptomatic at the time of recurrence and 59% with a neurologic deficit. (IJROBP 2002)
According to randomized data, what is the effect of delaying WBRT after SRS for pts with 1–4 brain mets?
JROSG99–1 showed that the omission of WBRT after SRS for 1–4 brain mets does not affect survival but increases the risk of intracranial relapse (46% with SRS + WBRT vs. 76.4% with SRS alone) and thus increases the need for salvage Tx. (Aoyama H et al., JAMA 2006)
What was the 1st randomized trial to assess the effect of delaying WBRT after SRS?
The 1st trial to assess the effect of delaying WBRT after SRS was JROSG99–1. 132 pts with 1–4 mets were randomized to SRS or WBRT + SRS. The SRS dose was based on size (lesions ≤2 cm to 22–25 Gy; lesions >2 cm to 18–20 Gy) and randomization (30% SRS dose reduction for pts on the WBRT arm). The WBRT dose was 30 Gy in 10 fx. (Aoyama H et al., JAMA 2006)
What prospective data support the omission of WBRT in pts treated with SRS alone?
Chang EL et al. randomized 58 pts with 1–3 brain mets (57% single) with KPS ≥70 to SRS alone vs. SRS + WBRT (30 Gy in 2.5 Gy/fx). SRS + WBRT resulted in a significant decline in 4-mo recall (24% vs. 52%) and median OS (15 mos vs. 6 mos) as compared to SRS alone. Pts treated with SRS + WBRT experience improved 1-yr LC (100% vs. 67%) and 1-yr distant brain control (73% vs. 44%) with SRS alone patients requiring more frequent salvage therapy. (Lancet 2009)
What are some criticisms of the trial?
Utilization of a single neurocognitive metric to assess learning and memory (HTLV-R) at a single time point (4 mos post-Tx); decreased survival in the SRS + WBRT group despite 100% 1-yr LC and improved neurologic DFS (73% vs. 27%); incomplete accrual (stopped early due to worse cognitive outcomes in the WBRT + SRS arm).
Are any ongoing protocols investigating the role of SRS +/- WBRT?
Yes. RTOG 0671 is an RCT of pts with 1–3 cerebral metastases treated with SRS randomized to WBRT. The trial is open to accrual with a primary endpoint of OS.
Are there any data on SRS dosing with planned WBRT?
Yes. Retrospective data from the University of Kentucky showed that optimal control of brain mets ≤2 cm was achieved with SRS of 20 Gy + WBRT. Pts treated with >20 Gy SRS + WBRT had higher rates of grade 3–4 neurotoxicity. (Shehata M et al., IJROBP 2004)
Are there any data comparing surgery + WBRT with SRS alone?
Yes. Retrospective data from Germany comparing RPA class I–II pts with 1–2 brain mets treated either with surgery + WBRT or SRS alone suggests that SRS is as effective. Of 206 pts treated from 1994–2006, 94 pts had SRS alone (18–25 Gy), and 112 pts had resection + WBRT (30 Gy/10 or 40 Gy/20). At 12 mos, there was no difference in OS (∼50% in both groups), LC, or brain control. There was no difference according to the RPA group. (Rades D et al., Cancer 2007)
What is the role for hypofractionated stereotactic radiotherapy (hfSRT)?
Large metastases (>3 cm) and irregular shaped lesions correlate with inferior outcomes and result in increased toxicity with SRS. Martens B et al. retrospectively analyzed therapeutic results in 75 pts with 108 intracranial mets (48% rcvd primary hfSRT while 52% were treated following prior WBRT) with a variety of dose concepts (primary hsFRT: 5 Gy × 6–7 fx and 6 Gy × 5 fx; recurrent hsFRT 4 Gy × 7–10 fx and 5 Gy × 5–6 fx). A cumulative EQD2 (equivalent dose 2 Gy) of ≥35 Gy resulted in improved LC with acceptable toxicity. (Cancer 2012)
Can pts treated with WBRT for brain mets be reirradiated?
Yes. Wong WW et al. reported on a series of 86 pts Tx with reirradiation (median dose 20 Gy) due to progressive brain mets (median initial dose 30 Gy). 70% experienced neurologic improvement (24% complete resolution; 47% partial resolution). (IJROBP 1996)
What dose should be used for reirradiation after WBRT for brain mets?
The optimal dose for reirradiation after WBRT is unknown. 20 Gy in 10 fx is often used.
How are the fields arranged for WBRT?
WBRT is delivered using opposed lat fields; a post gantry tilt of 3–5 degrees is used to avoid divergence into the eyes; and multileaf collimation or custom blocks are used to ensure adequate coverage of the cribriform plate, temporal lobe, and brainstem while protecting the eyes, nasal cavity, and oral cavity. The inf border is generally set at C1-2.
Should surgery be used for recurrent tumors?
Yes. Retrospective data from MDACC have suggested that reoperation for recurrent brain mets can prolong survival and improve QOL. Multivariate analysis revealed several negative prognostic factors: presence of systemic Dz, KPS <70, short time to recurrence (<4 mos), age ≥40 yrs, and breast and melanoma primaries. (Bindal R et al., J Neurosurg 1995)
What is the advantage of tumor bed radiosurgery after brain met resection?
Retrospective data from the University of Sherbrooke in Canada have suggested that SRS to the tumor bed following resection for brain mets achieves LC rates that are comparable to WBRT but does not impact the development of remote brain mets. 40 pts underwent resection → SRS at a median of 4 wks postresection. 73% achieved LC, and 54% developed new brain mets. (Mathieu D et al., Neurosurgery 2008)
Are any prospective trials investigating the role of SRS vs. WBRT for resected metastatic brain Dz?
Yes, RTOG 1270 is an RCT open to accrual investigating the role of postoperative SRS boost to the surgical cavity vs. adjuvant WBRT following surgical resection of intracranial mets.
Are professional guidelines available to provide Tx recommendations for pts with newly diagnosed brain mets?
Yes, ASTRO published an evidence-based guideline of Tx recommendations dependent on the goal of Tx (survival, local control, distant brain control, and neurocognitive function) and estimated prognosis. (PRO 2012)
 TOXICITY
TOXICITY
What are potential acute toxicities of WBRT?
Potential WBRT acute toxicities: alopecia, fatigue, HA, n/v, ototoxicity
What are potential long-term toxicities of WBRT?
Potential WBRT chronic toxicities: thinned hair, decline in short-term memory, altered executive function, leukoencephalopathy, brain atrophy, normal pressure hydrocephalus, RT necrosis
What is the relationship between WBRT-induced brain mets shrinkage and neurocognitive function?
WBRT-induced brain met shrinkage correlates with improved neurocognitive function. This was demonstrated in an analysis of 208 pts with brain mets randomized to WBRT alone on a phase III trial of WBRT +/– motexafin gadolinium. Pts with a good response (>45% tumor volume reduction at 2 mos) to WBRT had a longer time to decline in neurocognitive function. (Li J et al., JCO 2007)
What is the reported risk of severe dementia with WBRT?
DeAngelis L et al. reported an 11% (5 pts) risk of radiation-induced dementia in long-term brain mets survivors (>12 mos) based on a retrospective review of 47 pts Tx with WBRT. 3 pts were treated with nonstandard fractionation, 1 pt rcvd concurrent adriamycin, and 1 pt rcvd 30 Gy in 3 Gy/fx with a radiosensitizer. Of 15 pts Tx with <3 Gy/fx without systemic therapy, 0 developed severe dementia or neurocognitive symptoms. (Neurosurgery 1989)
What is the most important determinant of neurocognitive function?
The most important determinant is brain tumor control/delay of intracranial progression.
What other factors contribute to neurocognitive decline?
Anticonvulsants, benzodiazepines, opioids, chemo, surgical intervention (craniotomy), and systemic progression of Dz
What daily fx size in WBRT is associated with RT necrosis?
WBRT administered in fx sizes >3 Gy/day are associated with RT necrosis. (DeAngelis L et al., Neurology 1989)
Name the potential acute toxicities of SRS for brain mets.
Potential acute toxicities of SRS for brain mets: HA, nausea, dizziness/vertigo, seizure
What is the risk of symptomatic RT necrosis after SRS for brain mets?
There is an ~5% risk of symptomatic RT necrosis secondary to SRS for brain mets. This is usually treated with steroids but may require surgery or bevacizumab for refractory cases.
What are the dose limits to critical structures with SRS?
Brainstem 12.5 Gy, optic chiasm or optic nerves 10 Gy, other cranial nerves 12 Gy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


