Branchial Apparatus Developmental Anomalies
KEY POINTS
- Imaging is central to proper the diagnosis of branchial apparatus anomalies.
- Magnetic resonance imaging and computed tomography are the prime diagnostic tools unless a sinus tract can be injected.
- Ultrasound is cost additive, not definitive, and should be avoided in almost all cases for these reasons.
- There should never be an assumption that “carcinoma arising in a branchial cleft cyst” is a plausible diagnosis.
- A cystic neck mass in an adult should be presumed to be a cystic metastatic node until definitively proven otherwise.
Congenital anomalies of the branchial apparatus affecting the neck come to imaging commonly in both the pediatric and adult population. Their embryologic origin explains the diverse appearance of these anomalies on imaging studies as well as their various clinical presentations. Anomalous branchial apparatus development results in glandular ectopia as well as various cysts, sinuses, and fistulas. These anomalies may be of branchial, thymic, and parathyroid origin. Their anatomic relationships and appearance on imaging studies predicts their embryologic origin and raises related treatment implications.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
General Embryologic Mechanisms
The general mechanism of these developmental errors is incomplete obliteration of the branchial apparatus leaving buried cell rests trapped where they do not belong during the embryologic stage and they later producing branchial apparatus–related problems.1,2 Neck development is so complex that it gives rise to a broad variety of anomalies each with its own possible variations. Branchial cysts, sinuses, and fistulas are the most common and well known; however, ectopic thymic and parathyroid tissue and cysts also occur. Trapped cell rests, regardless of the specific site of entrapment, most commonly form branchial apparatus cysts in later life. Alternatively, a nonobliterated branchial cleft, pouch, or cervical sinus of His most commonly produces a sinus, fistula, and/or cyst.1,2 Lack of obliteration of those portions of the developing branchial apparatus may also produce aberrant migration and ectopias of glandular tissue or cysts related to glandular migration pathways.1,2
Normal Embryology of the Branchial Apparatus
The branchial apparatus has six mesodermal arches separated externally by ectodermal-lined branchial clefts or grooves and internally by endodermal-lined pharyngeal pouches1,2 (Fig. 153.1). The second arch proliferates and increases in thickness, ultimately growing caudally to meet the enlarging epipericardial ridge of the fifth arch. This causes the second, third, and fourth branchial clefts to become enclosed in an ectodermal-lined cavity called the cervical sinus of His (Fig. 153.2). This sinus will be obliterated by the fusion of its walls producing the smooth, uniform surface of the mature neck1,2 (Fig. 153.2).
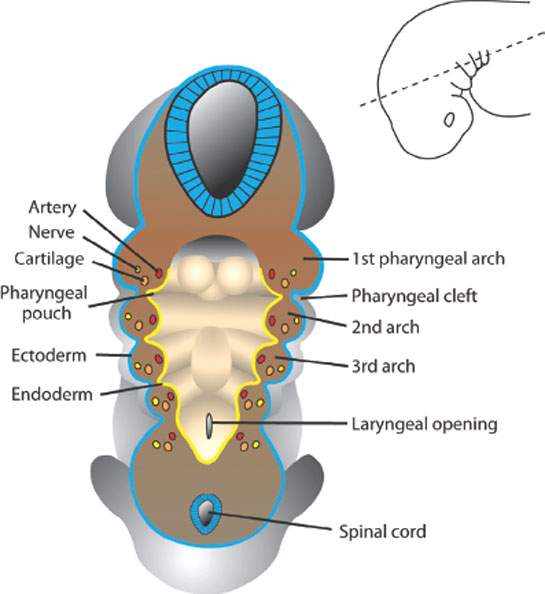
FIGURE 153.1. Illustration of the basic relationship of the first branchial arches, clefts, and pouches in an early embryologic stage. (From Sadler TW, ed. Head and neck. In: Langman’s medical embryology. 10th ed. City, State: Lippincott Williams & Wilkins; 2006: 257–283, with permission.)

FIGURE 153.2. A: Development of the pharyngeal clefts and pouches. The second arch grows over the third and fourth arches and in that extension covers the second, third, and fourth pharyngeal clefts. B: The remnants of the second, third, and fourth pharyngeal clefts form the cervical sinus of His, which eventually become obliterated. Other structures indicate their origin from various pharyngeal pouches. (From Sadler TW, ed. Head and neck. In: Langman’s medical embryology. 10th ed. City, State: Lippincott Williams & Wilkins; 2006:257–283, with permission.)
The thymus, parathyroid glands, and ultimobranchial body are endodermal derivatives of the pharyngeal pouches that eventually migrate to their final position1 (Fig. 153.3).

FIGURE 153.3. The migration of the thymus and parathyroid glands from their pouches of origin and that of the ultimobranchial body are demonstrated. The thyroid development is relatively independent of the branchial arch development. (From Sadler TW, ed. Head and neck. In: Langman’s medical embryology. 10th ed. City, State: Lippincott Williams & Wilkins; 2006:257–283, with permission.)

FIGURE 153.4. The structures developing from cartilage of the various branchial arches are demonstrated. (From Sadler TW, ed. Head and neck. In: Langman’s medical embryology. 10th ed. City, State: Lippincott Williams & Wilkins; 2006: 257–283, with permission.)
The mesoderm of the branchial arches contributes to specific bone, cartilage, and vascular structures, and each arch is related to a specific cranial nerve1 (Fig. 153.4).
The adult structures derived from the branchial arches and related clefts and pouches become the anatomy of interest for identifying and treating anomalies related to the branchial apparatus. The following sections will identify in more detail those derivatives and their related diagnostic and imaging implications.
In summary form (Figs. 153.1–153.5), the first branchial cleft is one that persists as an adult structure providing the epithelium of the external auditory canal.1,2 The other clefts, including the cervical sinus of His, are obliterated as the neck develops.1,2 The first arch contributes to facial development, while the other arches contribute to development of the larynx, pharynx, and face. The first pharyngeal pouch forms part of the eustachian tube and tubotympanic recess. The pouches are lined by endoderm, explaining the origin and migration of glands of the head and neck (Fig. 153.3). The parotid gland, a first pouch derivative, is an epithelial growth starting at the oral cavity and migrating toward the ear. Continuing the glandular theme, the third branchial pouch endoderm forms the superior parathyroid glands and thymus, while the fourth pouch endoderm is the source the inferior parathyroid glands. The second pouch contributes to the tonsillar fossa.
The vascular development of the branchial apparatus is complicated.1,2 It is enough to realize that as the six pairs of aortic arches develop, their elements come and go in time. The artery of the third arch persists as the common and proximal portion of the internal carotid artery. The origin of the external carotid artery is uncertain, but it is known that it connects with the third aortic arch anteriorly and has a complex relationship to second arch development. The right fourth aortic arch forms the proximal portion of the right subclavian artery. The left fourth aortic arch forms part of the aortic arch. The fifth and the sixth pairs of aortic arches are of no interest in the neck.

FIGURE 153.5. The anterior aspect of the pharyngeal arches as they relate to the development of the oropharynx and laryngopharynx at the 5-week (A) and 5-month (B) embryologic stages. The foramen cecum is the focal point of thyroid development. (From Sadler TW, ed. Head and neck. In: Langman’s medical embryology. 10th ed. City, State: Lippincott Williams & Wilkins; 2006:257–283, with permission.)
Classification of Branchial Anomalies
The basic classification of a branchial anomaly is by whether it is a sinus, fistula, or cyst.
A sinus is a tract that opens externally and rarely internally, and it may communicate with a cyst (Fig. 153.6). Sinuses are lined by stratified squamous, ciliated, or columnar epithelium and may have mural lymphoid tissue.1,2
A fistula communicates internally and externally when there is both a persistent branchial cleft and pharyngeal pouch (Fig. 153.3). They are epithelial-lined tracts that connect the skin to the related foregut element—namely, the lumen pharynx.1,2
Cysts do not communicate internally or externally (Fig. 153.3). They are usually lined by stratified squamous epithelium but may be lined by columnar epithelium if of pouch origin.1,2
The branchial anomalies are also classified according to their pouch or cleft of origin. Classification is done mainly to anticipate anatomic relationships that may be important treatment considerations, such as the course and point of pharyngeal communication of a fistula or sinus tract that has become complicated by infection so that it can be treated completely. Bailey et al. have classified both first and second branchial cysts, and this system has persisted in the imaging literature1–6 to help in this regard. All classification systems are limited since these anomalies are protean, and strict adherence to classification is not entirely possible or necessary.

FIGURE 153.6. A: Image shows how an external fistula or sinus tract may develop from the branchial cleft remnant. B: Typical position of periauricular and lateral cervical cysts as they present on the skin surface as a sinus tract or in the neck as a cyst. C: Image shows how a remnant of the clefts creates lateral cervical cysts that may communicate with the pharynx, in this case relating to the oropharynx, as the cyst and fistula develop from the second branchial apparatus. (From Sadler TW, ed. Head and neck. In: Langman’s medical embryology. 10th ed. City, State: Lippincott Williams & Wilkins; 2006:257–283, with permission.)
First Branchial Anomalies
The first branchial apparatus is involved in the development of the maxilla, mandible, eustachian tube, external auditory canal, and portions of the middle ear structures; thus, there is some potential for its derivatives to result in a cyst along the eustachian tube and associated anomalies of the other just-named structures.1,2,4 First branchial apparatus development also includes that of the parotid gland as the gland migrates posteriorly from oral cavity endoderm toward the external ear. The facial nerve and region muscles, which are first arch mesodermal derivatives, migrate anteriorly so that a cell rests or other residua from a first branchial anomaly cross and in that crossing become potentially closely related to the parotid gland and/or facial nerve.1,2 From these areas of origin, a cyst may enlarge to present below the angle of the mandible or within or around the parotid gland1–4 (Figs. 153.7 and 153.8).
Several authors have attempted to classify first branchial anomalies into types4,5,6. It is most important to use such schemes to understand the potential anatomic variations related to the regional embryology than it is to name them.1–3 Bailey type 1 cysts are generally superficial in location relative to the parotid gland and present as a periparotid mass or inflammation (Fig. 153.8). Bailey type 2 cysts run through the gland usually deep to the expected position of the facial nerve main trunk, with the cyst presenting in the upper neck1–6 (Fig. 153.7).
These cysts will present as a periparotid or upper neck mass. If there is a sinus tract to the skin, the presentation may be that of inflammation in these regions or of an infected cyst (Fig. 153.8A–D). Facial nerve dysfunction is rare. A related sinus tract will typically be at the junction of the bone and cartilage portions of the external auditory canal. The canal may be deformed, and a separate epidermoid cyst might be present (Figs. 153.7 and 153.8).


FIGURE 153.7. Three patients with first branchial apparatus anomalies. A–C: Patient 1 presenting with a fistula at the level of the hyoid due to a first branchial apparatus anomaly. A contrast-enhanced computed tomography (CT) study was done. The terminal aspect of the cyst with surrounding inflammation is seen in (A) (arrow). In (B), the cyst (arrow) is seen deep to the retromandibular vein (arrowhead), projecting into the adjacent parapharyngeal space. In (C), there is a deformed tympanic bone (arrows) and a bony tract extending directly into the middle ear cavity (arrowheads). D–F: Patient 2, a young adult presenting with a mass at the angle of the mandible. Contrast-enhanced CT was done. In (D), a cystic mass with an enhancing wall (arrow) is seen to connect in (E) with a tract extending through the deep portion of the parotid gland (arrows) and a somewhat anomalous-appearing retromandibular vein (arrowhead) draining to the pterygoid plexus. This indicates that there is abnormal development likely just deep to the expected course of the facial nerve. In (F), the bony tract associated with this first branchial arch anomaly is shown extending toward the junction of the cartilage and bony portion of the external auditory canal (arrow). (NOTE: At surgery, the facial nerve, while not directly involved, had to be carefully separated from the course of the tract going through the anomalous parotid tissue.) G, H: Patient 3 presenting with signs and symptoms of right eustachian tube obstruction, shown on this study to be due to a cystic mass tracking along the eustachian tube (arrows) and subsequently shown to be an epithelial line and presumed to be a first branchial pouch anomaly.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








