SONOGRAM ABBREVIATIONS
AX Axilla
CA Carcinoma
CC Craniocaudal
DCIS Ductal carcinoma in situ
FCC Fibrocystic change
IDC Invasive ductal carcinoma
MLO Medial lateral oblique
SA Subareolar
TDLU Terminal ductolobular unit
KEY WORDS
Antiradial. Is 90 degrees to the radial plane.
Benign. Refers to a condition, tumor, or growth that is NOT cancerous; it does not spread to other parts of the body or invade nearby tissue. Benign tumors usually grow slowly.
DCIS. Ductal carcinoma in situ, or DCIS, is the most common kind of noninvasive breast cancer. It is ductal because the cancer is confined to the milk ducts.
Fibroadenoma. A benign tumor that represents a hyperplastic or proliferative process in a single terminal ductal unit.
Fibrocystic Change. Common, benign changes involving the tissues of the breast. Formerly the term “fibrocystic disease” was used; because this is misleading, many providers prefer the term “fibrocystic change.” The condition is so commonly found in normal breasts that it is believed to be a normal variant. Other related terms include “mammary dysplasia,” “benign breast disease,” and “diffuse cystic mastopathy.
Fremitus. A thrill of the chest wall. The tissues surrounding a lesion will vibrate and fill in with echoes, whereas the lesion itself will be void of power Doppler signal.
Invasive. Invasive ductal carcinoma (IDC) accounts for approximately 80% of all breast cancers. Invasive means that it has “invaded” or spread to the surrounding tissues.
Radial. Scan plane running the same direction as the ducts, similar to the spokes on a bicycle wheel.
TDLU. Terminal duct lobular unit, terminal ductolobular unit. The functional unit of the breast.
Clinical Problem
Breast ultrasound is a valuable tool in the diagnosis of breast disease. Most often it is used as a diagnostic rather than a screening procedure. It is targeted to a specific clinical or focal mammographic finding in the majority of patients. Breast ultrasound should be performed on palpable lumps when the mammogram in the area of the lump is negative or nonspecific.
In addition, it should be born in mind that breast ultrasound is extremely operator-dependent, and therefore it is essential to receive appropriate training and use the appropriate equipment.
Anatomy
SONOGRAPHIC APPEARANCE
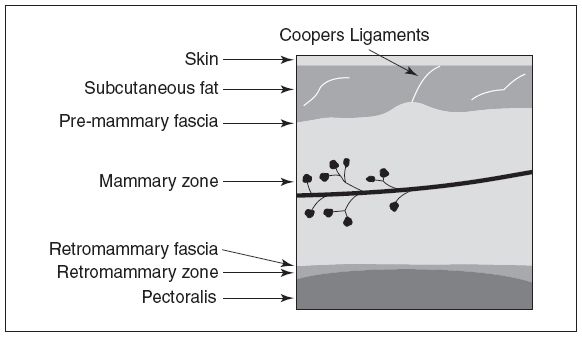
Sonographically, the skin is hyperechoic and approximately 2 mm thick. Subcutaneous fat is seen anterior to the premammary fascia. Cooper’s ligaments may be seen as hyperechoic bands coursing through the subcutaneous fat. The mammary zone is where the majority of breast cancers detectable by ultrasound are located. Posterior to the mammary zone is the retromammary fascia and fat. The most posterior structures are the pectoralis muscle and then the lung (Fig. 28-1).
Figure 28-1. ![]() Layers of breast tissue visualized by ultrasound. (Adapted from Stavros AT. Breast Ultrasound. Philadelphia: Lippincott Williams & Wilkins; 2004, with permission.)
Layers of breast tissue visualized by ultrasound. (Adapted from Stavros AT. Breast Ultrasound. Philadelphia: Lippincott Williams & Wilkins; 2004, with permission.)
NORMAL DEVELOPMENT
During the fifth week of human development, the embryo develops a milk line that extends from the armpit to the groin. Most of the ridge involutes, leaving an upper portion that remains to form the breast bud. If there is failure of involution along any portion of this “milk line,” accessory breast tissue may form. The most common sites for accessory breast tissue are just below the breast and the axilla. By birth, the breast bud has developed a network of small branching ducts. At puberty, the ducts elongate and proliferate, and mature lobules form. Over the next several years, the process continues with growth of connective tissue and the deposition of fat. With the onset of menarche, normal cyclic breast changes begin, stimulated by estrogen and progesterone. These changes are characterized by premenstrual changes in the lobar acinar cells and stromal elements, breast edema, and venous congestion. The hormones of pregnancy cause marked proliferation of both ductal and lobular elements. Normal age-related involutional changes occur at variable rates and can begin before menopause. This change is characterized by atrophy of the ducts and lobules.
BREAST COMPOSITION
The breast is composed of fibroglandular and ductal tissue that is surrounded by and intermixed with fat. It is completely surrounded by superficial and deep fascia and covered by skin. Cooper’s ligaments are supportive fibrous bands that course between the superficial and deep fascial layers. Breast tissue extends from the second to seventh rib but can extend as far superiorly as the clavicle. The sternum and anterior axillary lines mark the medial and lateral boundaries, but breast tissue can extend into the axilla. The glandular parenchyma is composed of approximately 15 to 20 lobes, each with its own excretory duct that terminates in the nipple. Montgomery’s glands are small oil glands that are located around each areola. They release a lubricant that protects the nipples during nursing. Each excretory duct branches into multiple segmental ducts, terminating as the extralobular terminal ducts. It is from this portion of the duct that most breast cancers arise. This duct continues as the intralobular terminal duct and branches into 10 to 100 blind ending ductules called acini. The intralobular terminal duct and acini are surrounded and contained by loose fibrous connective stromal tissue; this unit is called the lobule. There are approximately 20 to 40 lobules per lobe. Connective tissue is present within and surrounding the lobular units (Fig. 28-2).
BLOOD SUPPLY
The arterial supply to the breast is composed of the lateral mammary branch of the lateral thoracic artery, the anterior cutaneous or perforating branches of the internal mammary artery, and the branches derived from the second to the sixth intercostal arteries. The veins describe an anastomotic circle around the base of the nipple, the so-called “circulus venosus.” From the circulus, small veins take the blood to the circumference of the gland before terminating in the axillary and internal mammary veins.
BREAST LYMPHATICS
The lymphatic drainage is particularly important because it is by this route that the spread of malignant disease may occur. There is both a superficial and a deep plexus of lymphatic vessels. The superficial plexus lies beneath the skin anterior to the gland. It receives afferent vessels from the gland and sends its efferent lymph to lymph nodes in the pectoral and infraclavicular chains; other vessels pass to the deep plexus that lies in the deep fascia on which the mammary gland rests. It is this plexus that directly receives most of the lymphatic drainage of the breast.
MISCELLANEOUS ANATOMIC POINTS
Age-Related Changes
In the prepubertal child, the breast contains a few small ducts scattered throughout the fibrous stroma without formation of lobules. With the onset of estrogen secretion by the ovaries, glandular tissue enlarges quickly (thelarche). This breast development occurs before menarche. Occasionally, asymmetric development may simulate a hard subareolar nodule; one should not mistake this for a tumor because excision will remove all of the glandular tissue and prevent the development of the breast.
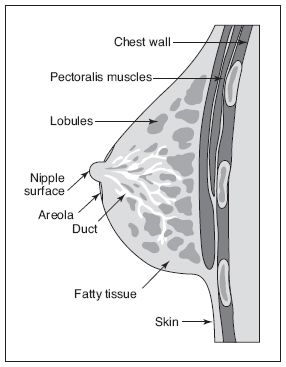
Figure 28-2. ![]() Normal breast anatomy.
Normal breast anatomy.
In the young woman, glandular tissue is relatively thick and the subcutaneous and retromammary fat areas are small.
During pregnancy and lactation, there is considerable increase in the size and numbers of the terminal ductolobular units (TDLUs) at the expense of the breast stroma and epithelial elements. This breast has very little fatty tissue. Occasionally, asymmetric secretory changes may occur in the breast resulting in a palpable abnormality.
Involutional changes occur after full-term pregnancies with progressive thinning of the mammary zone. The parenchymal and stromal atrophy is most pronounced in the area between Cooper’s ligaments. In extreme involution, the parenchymal elements are almost absent and only strands of connective tissue are seen, appearing as echogenic bands between the isoechoic fat.
Anomalies
Amastia, complete absence of one or both of the breasts, absence of breast tissue or the nipple, or a rudimentary mammary gland, is rare.
Accessory or supernumerary breasts occur in approximately 1% to 2% of patients and may involve any of the three components of the breast: the fibroglandular parenchyma, areola, or nipple.
The most common anomaly is an accessory nipple (polythelia), which can occur in both male and female patients. This nipple can develop anywhere along the milk line, but the most common location is just below the normal breast.
Congenital nipple flattening or inversion needs to be differentiated from retraction of the nipple that can be caused by a carcinoma or ductal ectasia.
Accessory breast tissue is often asymmetric from left to right. The axillary segment is most often involved, but accessory breast tissue can occur anywhere along the milk line. Accessory breast tissue can be the cause of mammographic asymmetry or a palpable lump.
Technique
EQUIPMENT
Breast ultrasound must have excellent spatial and contrast resolution. Both the axial and lateral components of spatial resolution must be good. Broadband, high-frequency linear electronically focused probes currently offer the best combination of spatial and contrast resolution for breast ultrasound.
AXIAL RESOLUTION
Excellent axial resolution is important in identifying normal structures that course parallel to the skin (such as the mammary ducts and fascial planes surrounding the mammary zone) and in identifying the characteristics of the capsules around cysts and solid nodules.
LATERAL RESOLUTION
Lateral resolution at all depths within the breast is important to minimize volume averaging of surrounding normal breast tissues with pathologic lesions. Such volume averaging may cause mischaracterization of small cystic lesions as solid and may even cause small solid lesions to be indistinguishable from surrounding tissues. Lateral spatial resolution is also a complex subject. For linear probes, there are two planes that determine lateral resolution, the long axis and short axis (elevation plane focus).
The long axis of the linear probe can be electronically focused. Continuous electronic focusing may be done on receive or transmit phases. The degree of electronic focusing on receive depends on many factors, including the following:
![]() Number of channels
Number of channels
![]() Aperture size
Aperture size
![]() Number of elements
Number of elements
![]() Number of scan lines
Number of scan lines
In general, lateral resolution improves with increasing number of channels, aperture size, number of elements in the transducer, and scan lines. Electronic focusing on transmit depends on many of the same factors as receive focusing but is more limited. It depends on the number of transmit zones. In general, the more transmit zones, the better the lateral resolution. However, increasing the number of transmit zones decreases the frame rate. In general, multiple transmit focal zones in the first 2 cm are very beneficial in breast sonography.
ELEVATION PLANE
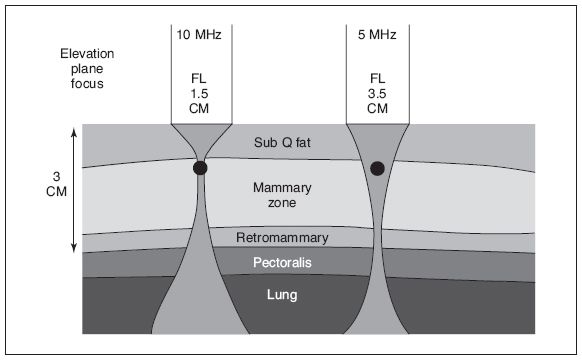
The elevation plane (short axis) of the probe cannot currently be electronically focused. The elevation plane is focused at a fixed depth by an acoustic lens. The manufacturer decides how deeply to focus this plane before the probe is built. Elevation plane focal lengths are usually decided by the application for which the probe will primarily be used. Dedicated small parts or near-field probes should be focused at approximately 1.5 cm or even more superficially (Fig. 28-3).
Five-megahertz linear array probes were designed with peripheral vascular applications in mind and are focused in the elevation plane at approximately 3 to 4 cm. This is too deep for most breast imaging, because the elevation plane for these probes would correspond to the pectoralis muscle in most patients. In general, a 7.5- to 13-MHz transducer, with an elevation plane of approximately 1.5 cm, is the best breast ultrasound transducer currently available (Fig. 28-4).
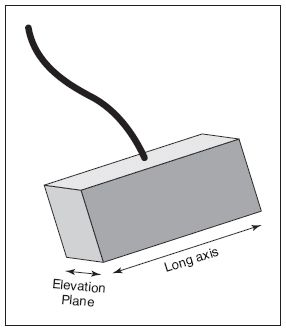
Figure 28-3. ![]() Relationship of elevation plane to the long axis of the transducer.
Relationship of elevation plane to the long axis of the transducer.
Figure 28-4. ![]() If a 5-MHz transducer is used and the lesion of interest is small and superficial, volume averaging of adjacent normal tissues will be a problem. Cysts may fill in and be misclassified as solid. Small solid lesions may be completely missed. (Adapted from Stavros AT. Breast Ultrasound. Philadelphia: Lippincott Williams & Wilkins; 2004, with permission.)
If a 5-MHz transducer is used and the lesion of interest is small and superficial, volume averaging of adjacent normal tissues will be a problem. Cysts may fill in and be misclassified as solid. Small solid lesions may be completely missed. (Adapted from Stavros AT. Breast Ultrasound. Philadelphia: Lippincott Williams & Wilkins; 2004, with permission.)
If a palpable nodule is very small and near the skin, even optimally focused transducers may have difficulty resolving and characterizing the lesion. In such circumstances, a 1-cm standoff pad or a large “glop” of gel should be used to move the elevation plane focus closer to the skin.
ANNOTATION
Most ultrasound departments use the clock method to label breast images. In addition, ABC and 123 notation is helpful to label the exact location of a lesion.
If a lesion is being labeled for the purpose of biopsy, distance from nipple to lesion should also be included.
First a clock position is stated. Second, the location of the lesion is noted. There are five possible choices for the 123 location. One through 3 is divided into 3 concentric rings. A lesion near the nipple is location 1, a lesion midway out in the breast is 2, and a lesion in the periphery is 3. If a lesion is under the nipple, it should be labeled SA for subareolar; lesions in the axilla are labeled AX.
ABC notation: A is used if a lesion is near the surface or close to the transducer. B is used if a lesion is midway down and represents the mammary zone in the breast. C is used in the setting of lesions located against the chest wall (Fig. 28-5).
POSITIONING
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree