and Clarisse Dromain2
(1)
Department of Radiology, San Giovanni Hospital, Roma, Italy
(2)
Department of Radiology, Institut de Cancerologie Gustav Roussy, VilleJuif – Paris, France
Abstract
The term of carcinoid tumor, first introduced by a pathologist in 1907 to designate tumor thought to be benign that looks like a carcinoma, refers in fact to very different entities. It should no longer be used. The WHO recommendations are to use the term of neuroendocrine tumor (NET) in association with the seat and degree of differentiation of the tumor. Carcinoid tumor usually refers to a well-differentiated NET of the appendix or the small bowel embryologically arising from the midgut most often localized in the ileum. Other locations of NET are the pancreas, the lung, the stomach, and, more rarely, the rectum, the esophagus, and the hypopharynx.
Carcinoid
The term of carcinoid tumor, first introduced by a pathologist in 1907 to designate tumor thought to be benign that looks like a carcinoma, refers in fact to very different entities. It should no longer be used. The WHO recommendations are to use the term of neuroendocrine tumor (NET) in association with the seat and degree of differentiation of the tumor. Carcinoid tumor usually refers to a well-differentiated NET of the appendix or the small bowel embryologically arising from the midgut most often localized in the ileum. Other locations of NET are the pancreas, the lung, the stomach, and, more rarely, the rectum, the esophagus, and the hypopharynx.
Carcinoid tumors account for 25 % of all small bowel tumors, and multiple primary sites occur in 15–35 % of patients. Carcinoid tumors arise in the submucosa and grow very slowly, but all have malignant potential. Malignancy is determined by the presence of local invasion or metastatic spread, rather than histologically. Tumors smaller than 1 cm are rarely invasive, whereas those larger than 2 cm have usually metastasized by the time of diagnosis.
Most of tumors are asymptomatic. However a carcinoid syndrome with flush and diarrhea occurs in 10 % of patients due to relapse of a vasoactive substance, the serotonin. The presence of a carcinoid tumor is a sign of very large tumor, with serotonin secretion that exceeds the capacity of liver metabolism, or more frequently the presence of liver metastases. In more advanced tumor, a mesenteric involvement with an important fibrotic reaction (due to serotonin secretion) may cause König syndrome and small bowel occlusion (Fig. 1). Finally, liver metastases are present in 20 % of patients at the time of diagnosis.
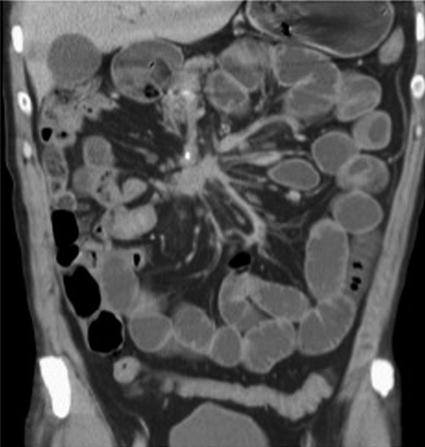
Fig. 1
Mesenteric carcinomatosis from a carcinoid tumor. Coronal reconstruction CT image shows a fibrous mesenteric mass with distorted bowel loops and dilatation of mesenteric vessels very suggestive of a mesenteric carcinomatosis from a neuroendocrine ileal tumor
CT enteroclysis is the imaging method of choice for the detection of the primary tumor allowing a good visualization of the small bowel wall as well as the extraluminal environment. Acquisition techniques must be standardized and optimized, including acquisitions at the late arterial (30 s after the beginning of injection) and portal venous (70–90 s after the beginning of injection) phases. The contribution of arterial acquisition increases sensitivity (20 % up) of the detection of liver metastases.
CT imaging also plays a major role for the staging of the disease in association with somatostatin receptor imaging. 18F-DOPA PET is the scintigraphy of choice, enabling to detect midgut NETs that produce serotonin, with a higher sensitivity than somatostatin receptor scintigraphy.
The liver is the most common site of NET metastases. Accurate liver assessment being crucial for the prognostic and the treatment planning, a liver MRI with diffusion-weighted images is recommended to be performed in the initial morphologic assessment. Liver metastases from NET are typically hypervascularized in the arterial phase with washout.
Carcinomatosis, Peritoneal
Peritoneal carcinomatosis (PC) is the seeding and implantation of neoplastic cells into the peritoneal cavity and represents the advanced stage of some abdominal and pelvic tumors. Ovarian, stomach, and colorectal cancers are the most common primary tumors leading to PC.
Recent aggressive surgical treatment with complete resection of the peritoneal implants associated with intraperitoneal chemotherapy and hyperthermy (ICHP) yields a highly significant increase of overall survival rate of 53 % at 3 years and 48.5 % at 5 years. This new aggressive surgical approach requires accurate intraperitoneal assessment of the presence or the absence of peritoneal carcinomatosis but also of the exact extent of carcinomatosis.
CT is the imaging modality of choice for the detection of PC with an overall sensitivity ranging from 60 to 82 %. This sensitivity is depending on radiologists, tumor size, and the location of tumor deposits with lower sensitivity in lean patient without ascites, in case of infracentimetric tumor deposit and location in the pelvis, in the mesentery, or in contact with bowel loops. Different patterns of peritoneal carcinomatosis on CT imaging include ascites; tiny 1–5 mm nodules (Fig. 2a) most often localized in the greater omentum, lesser omentum, and mesentery; presence of >5 mm nodules with oval shape or a star-shaped appearance; a tissue mass which can reach sizes of several centimeters typically found in the pelvis; and irregular soft tissue thickenings of the abdominal viscera and peritoneal walls. In cases of involvement of the visceral peritoneum over small bowel loops and colonic surface, bowel distortion, bowel wall thickening, and bowel obstruction can be present. The infiltration of the greater omentum can range from increased density of fat anterior to the colon or small bowel to large masses, called omental cakes, separating the colon and small bowel from the anterior abdominal wall (Fig. 2b). Additional sign that may be related to the presence of peritoneal carcinomatosis is the appearance of a ureteral dilatation, ovary metastases, and the presence of cardiophrenic lymph nodes.
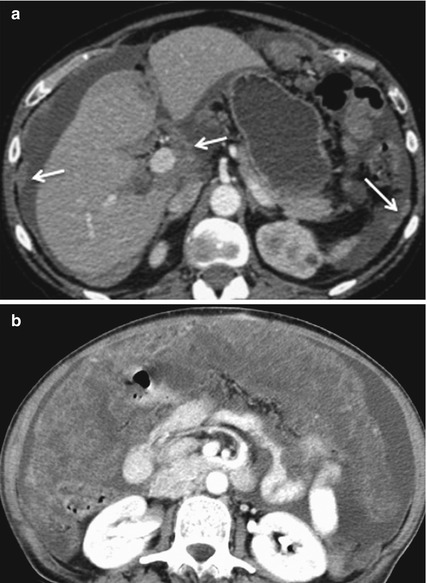
Fig. 2
(a) Peritoneal carcinomatosis: CT image shows ascites and tiny peritoneal nodules at the level of the peritoneal abdominal wall and lesser omentum (arrows). (b) Omental cake. Axial contrast-enhanced CT image shows a diffuse soft tissue density infiltration and thickening of the great omental fat corresponding to an advanced peritoneal carcinomatosis
FDG PET-CT has been reported to be useful for the detection of PC. Indeed, unlike CT, FDG PET has an excellent contrast resolution between the tumoral implant and the background signal allowing a good visibility of PC nodules. The sensitivity of PET scan varies from 63 to 93 % depending to the PC location. However FDG PET has some limitations that are small size nodules, implants with a mucinous histology, and location in the right hypochondrium. Moreover some physiologic tracer uptake into the stomach and the bowel can mimic PC and lead to false positive.
Diffusion-weighted MRI has been also reported to have a high per-lesion sensitivity for the detection of PC. Using high b value, it allows a good suppression of the signal of fat, ascites, and digestive fluid. Its per-site sensitivity ranges from 74 to 90 %. Limits are the physiologic restriction of certain organs (lymph nodes, spleen, adrenal glands) and the T2 shine-through effect as well as low-cell-density tumor and calcified tumors.
Cathartic Colon
Cathartic colon is a functional complication due to prolonged use of stimulant or irritant laxatives resulting in neuromuscular incoordination. Some morphologic findings may suggest together with anamnestic and clinical data of the cathartic colon. Patients present with constipation, and abdominal bloating. Findings at imaging are represented by flattened and smooth colonic surface, diminished or absent haustration, “pseudostrictures” (tapered areas of narrowing due to sustained tonus of circular muscles), and shortened ascending colon. Cathartic colon usually affects elderly patients but may be also seen in younger patients as a possible complication of bulimia.
Cavitary Mesenteric Lymph Node Syndrome
Cavitary mesenteric lymph node syndrome is a complication of celiac disease consisting in the association of enlarged lymph nodes with central cavitation within the jejunoileal mesentery, splenic atrophy, and intestinal changes of celiac disease.
CDAI
CDAI (Crohn’s Disease Activity Index) is a score of inflammatory activity used in Crohn’s disease patient using clinical and laboratoristic data. CDAI is basically a research tool used to quantify the symptoms of patients with Crohn’s disease. CDAI is used in research studies done on medications used to treat Crohn’s disease; most major studies on newer medications use the CDAI in order to define response or remission of disease. Remission of Crohn’s disease is defined as a fall in the CDAI of less than 150. Severe disease was defined as a value of greater than 450. Most major research studies on medications in Crohn’s disease define response as a fall of the CDAI of greater than 70 points.
Cecal Volvulus
Colonic volvulus is a possible cause of colonic obstruction. Volvulus of the cecum is frequently associated with colonic malrotation with a long mesentery resulting in poor fixation of the right colon. Cecum may rotate anteriorly to the ascending colon (type I or “cecal bascule”) or in the left upper abdominal quadrant (type II). The volvulus is triggered usually by sudden colonic distension due to constipation and distal colonic obstruction or by trauma. Cecal volvulus may lead to vascular compromise with strangulation (see mesenteric ischemia) followed by perforation. Cecum caliber >10 cm is at risk for impending perforation or infarction.
Celiac Disease
Celiac disease (celiac sprue or gluten-sensitive enteropathy) is a form of intestinal malabsorption due to intestinal mucosa’s exposure to gluten. It is characterized by a wide spectrum of clinical presentation.
Typical presentation of celiac disease is pediatric onset of malabsorption symptoms. However celiac disease can be diagnosed in adult patients as well. When celiac disease is suspected, lab test (anti-gliadin anti-endomysium antibodies) as well as jejunal biopsy is necessary to confirm the diagnosis. Imaging plays a second role in the diagnosis of celiac disease. Many subjects affected by celiac disease do not have any imaging findings.< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree