and Sofia Gourtsoyianni2
(1)
UOC Radiologia BR, Azienda Ospedaliera Universitaria Integrata Verona, Verona, Italy
(2)
Imaging 2, Level 1, Lambeth Wing St Thomas’ Hospital, London, UK
CA 19-9
CA 19-9 is a serum antigen used in the diagnosis and management of hepato-pancreatico-biliary malignancies, although it is non-specific and can rise also in non-malignant conditions such as heavy tea consumption.
CA 19-9 > 100 U/ml may have a sensitivity of 50 % in diagnosing cholangiocarcinoma, while using an upper limit of normal at 37 U/ml achieves approximately 80 % sensitivity and 90 % specificity for pancreatic adenocarcinoma.
Caroli’s Disease
Caroli’s disease is an autosomal-recessive congenital disorder comprising of multifocal cystic dilatations of segmental intrahepatic bile ducts. It was first reported by Todd in 1818, but Jacques Caroli in 1958 defined it precisely with the different types.
The more common form of the disease is associated with periportal fibrosis and may progress to portal hypertension and cirrhosis. The less common “pure” or “simple” form is associated with intrahepatic stones, cholangitis and abscesses. Patients affected by Caroli’s disease have an increased risk of developing cholangiocarcinoma (up to 7 % of cases).
The estimated incidence of Caroli’s disease is 1 in 1,000,000, with no sex prevalence; more than 80 % of patients are diagnosed before the age of 30 years.
Patients with the most common type of Caroli’s disease present with symptoms related to hepatic fibrosis and portal hypertension, while those affected by the pure form present with recurrent attacks of cholangitis.
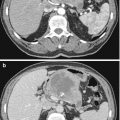
The characteristic CT appearance is multiple hypoattenuating cystic structures of variable size, which communicate with the biliary system. The “central dot sign” is highly suggestive of Caroli’s disease: tiny foci of contrast enhancement within the dilated intrahepatic bile ducts, corresponding to intraluminal portal vein radicles.
On MRI the dilated cystic biliary system appears hypointense on T1-weighted images and hyperintense on T2-weighted images. The central dot sign is appreciated also on post-gadolinium MRI images. MRCP demonstrates continuity of the cystic areas with the biliary tree.
Cavernous Transformation of the Portal Vein
Cavernous transformation of the portal vein consists of the formation of venous channels within and around a previously stenosed or occluded portal vein that act as porto-portal collateral vessels.
This cavernous transformation can occur as soon as 6–20 days after the thrombotic event, even if the thrombus is partially recanalised.
In case of portal vein thrombosis, if the portal vein does not recanalise (e.g. in patients with cirrhosis or chronic liver disease), the collateral paracholedochal veins dilate and become serpiginous. These veins drain into the left and right portal branches, or more distally into the liver parenchyma, forming a porto-portal shunt which however is usually insufficient to bypass the entire splenomesenteric inflow, and portal hypertension occurs.
The initial diagnosis is usually made at US, but CT and MRI can confirm it and better depict the anatomy. The most frequent finding is a characteristic beaded appearance (mass of veins) at the porta hepatis, with vessels that enhance in the portal venous phase. Calcifications can be present in the thrombosed portal vein.
Chemoembolisation
Transarterial chemoembolisation (TACE) refers to the administration of chemotherapeutic agents through selective catheterisation of the hepatic arteries. The chemotherapeutic agent can be mixed with iodised oil or adsorbed onto microspheres. The administration is followed by embolisation to stop arterial flow to the lesions. TACE is used most commonly for intermediate-stage HCC but also for hypervascular liver metastases.
The rationale is based on the fact that HCC and liver metastases receive blood supply from the hepatic artery, while the surrounding healthy liver parenchyma receives it from the portal vein. Chemoembolisation offers the ability to expose tumours to high local chemotherapeutic agent concentrations with minimal systemic drug bioavailability.
Cholangiocarcinoma (CCC)
Cholangiocarcinoma is a malignant tumour that may arise at any point of the biliary epithelium from intrahepatic biliary radicals to the ampulla of Vater. The majority of cases are adenocarcinomas. There is a strong association with Primary sclerosing cholangitis (PSC).
Intrahepatic and extrahepatic types exist with intrahepatic further classified as peripheral and perihilar, the latter also known as Klatskin tumour, being the most common type. Less frequently the tumour presents along the common hepatic duct and common bile duct.
Klatskin tumour is further classified as:
Type 1: >2 cm distance to bifurcation
Type 2: <2 cm distance, no involvement of bifurcation
Type 3: involvement of bifurcation
Type 4: involvement of intrahepatic branch ducts
Four different growth patterns have been identified:
(a)
Exophytic, where tumour grows outside the bile ducts and forms a mass, characteristic of the peripheral CCC
(b)
Infiltrative, along and engulfing the biliary tree, typical for perihilar and extrahepatic type
(c)
Polypoid, with intraluminal growth
(d)
Combined
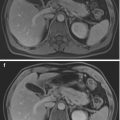
Mass–forming cholangiocarcinomas are typically homogeneously hypodense on non-contrast CT and show heterogeneous peripheral enhancement, with enhancement in the delayed phase. Capsular retraction may be present and the bile ducts distal to the mass are typically dilated.
Periductal infiltrating tumours appear as thickening of the periductal parenchyma with altered calibre of the involved duct, which can be narrowed or dilated. There is usually some distal dilatation of the biliary tree.
At MRI, CCC appears hypointense on T1-w and hyperintense on T2-w images and may present with delayed enhancement. A thickened bile duct wall >5 mm is considered suspicious.
Cholangitis
Acute cholangitis occurs due to bacterial infection of the obstructed biliary tree from the GI tract or the portal venous system. Cholangitis is a life-threatening condition if untreated which may also lead to hepatic abscess formation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree