▪ Imaging Modalities in Congenital Heart Disease
Multiple imaging modalities are used to define the morphology, vascular connections, and function of the heart in children with congenital heart disease. Such modalities include radiography, echocardiography, nuclear scintigraphy, computed tomography (CT), magnetic resonance imaging (MRI), and catheter angiography.
Multiple insults can occur in utero that can lead to congenital heart disease. In many cases a specific insult results in a single type of anatomic lesion, such as ventricular septal defect (VSD) or coarctation of the aorta. However, insults can result in a variety of anatomic abnormalities or “complex” congenital heart disease. Historically, chest radiography and clinical symptoms played a large role in narrowing the differential diagnosis of the types of congenital heart disease that may be present in a particular patient. With technologic advances and increased use of other imaging modalities, the dependency on chest radiography findings to diagnose the specific type of congenital heart disease has decreased, though it remains important in the identification of the possible presence of congenital heart disease.
Diagnosing a specific type of congenital heart disease by radiography is difficult. The role of radiography in making the diagnosis of congenital heart disease has probably been overemphasized in education. This is particularly true nowadays because most of the classically described radiographic findings of specific congenital heart disease do not manifest until after the neonatal period, and most patients in developed nations are diagnosed with congenital heart disease and are treated surgically during the neonatal period. However, in some cases the radiologist may be the first person to recognize that the radiographic findings in a newborn suggest that congenital heart disease rather than a pulmonary disorder is the cause of respiratory distress. Therefore it is important to understand the radiographic findings and role of radiography in relation to the other imaging modalities in the management of congenital heart disease.
Echocardiography
Echocardiography is the mainstay of congenital heart disease identification and diagnosis. This is particularly true during the fetal and neonatal periods. Most of the highly detailed anatomic and functional information needed for the medical and surgical management of patients with congenital heart disease can be obtained by ultrasound. Color Doppler can be used to identify areas of stenosis or regurgitation. However, there are populations of patients in whom echocardiography is less easily obtained and more prone to inaccuracy. These populations include older children, adults, and postsurgical patients. In these patients the acoustic window is decreased and echocardiography is more difficult. It is in these circumstances that echocardiography may not provide the necessary information needed for care, so CT and MRI play a role. It is important to keep in perspective the current relatively small (albeit growing) role of CT and MRI in cardiac imaging as compared with that of ultrasound.
Computed Tomography Angiography
The role of CT in the evaluation of congenital heart disease has rapidly increased as a result of the advent of multidetector CT technology, improved temporal resolution, and decreased ionizing radiation doses. The rapid speed of acquisition, ability to acquire volumetric data, and ability to obtain thin collimation have made CT very useful in patients with congenital heart disease. CT is beneficial in depicting those anatomic structures that are not easily seen on echocardiography, such as the pulmonary arteries, aorta, pulmonary veins, right-sided chambers, and vascular conduits. CT also enables a more global assessment of the airway and pulmonary parenchyma, which may also be abnormal in patients with congenital heart disease. CT is often used to depict complex congenital heart disease preoperatively and to evaluate the postoperative patient ( Fig. 4-1 ) for potential complications, such as stenoses, occlusions, and pseudoaneurysms. It is useful in evaluating the pulmonary veins, such as in suspected anomalous pulmonary venous return. CT is also useful in patients in whom pacemakers may preclude the use of MRI. Evaluation of metal stents is often less hampered by artifact in CT than in MRI, especially with new metal reduction algorithms on modern CT scanners. Although ionizing radiation exposure remains of paramount concern in medical imaging of children, the advent of newer technologies, such as iterative reconstruction, volume acquisition, and dual source scanners, has resulted in dramatic decreases in radiation exposure, improvement in temporal resolution associated with cardiac CT, and a resultant renewal of interest in its role in congenital heart disease evaluation.

Magnetic Resonance Imaging
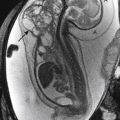
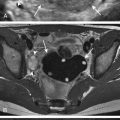
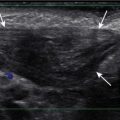
MRI has become a mainstay in the evaluation of certain types of congenital heart disease. MRI studies offer both anatomic and functional information. Cardiac gated spin echo imaging and double inversion recovery imaging, also known as “black-blood” imaging ( Fig. 4-2 ), are the main sequences used to demonstrate anatomic detail and spatial relationships between adjacent structures. These sequences allow for precise measurement of anatomic structures.

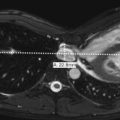
Cardiac gated cine MRI, or “bright-blood” imaging, can be obtained with a number of sequences. Predominantly a balanced steady-state free precession (bSSFP) sequence is used (e.g., FIESTA, TRUFISP, bFFE; Fig. 4-3 ), but a T2∗ GRE sequence (e.g., FLASH, SPGR) can also be used for “bright-blood” imaging. Data from these sequences can be processed to provide functional information, such as ventricular ejection fractions, and can also be used to demonstrate dynamic findings, such as turbulent blood flow related to stenosis or regurgitation. Phase-contrast imaging can be used to evaluate flow dynamics within vasculature structures. MR angiography using gadolinium and maximum intensity projection or shaded surface three-dimensional reconstructions is also useful in demonstrating complex anatomic relationships.

Computed Tomography versus Magnetic Resonance Imaging
With both CT and MRI becoming increasingly useful in the evaluation of patients with congenital heart disease, there is frequent debate regarding which examination is better for specific clinical indications. Although there are no clear-cut answers, there are advantages and disadvantages of both examinations. The benefits of CT include rapid acquisition time, avoiding the need for sedation in many cases, greater access for critically ill infants, less artifact resulting from metal stents and other structures, lack of pacemaker safety issues, and visualizing the airway and lungs. The major disadvantage of CT is radiation exposure. Techniques used in adults, including cardiac gating, thin collimation, overlapping imaging acquisition, and acquiring multiple sets of images, result in very high radiation doses relative to other CT examinations. Because of the radiosensitivity of children, many of these techniques are not appropriate when imaging children. Other disadvantages of CT include dependence on intravenous contrast bolus and relative lack of functional information. The primary advantages of MRI include lack of ionizing radiation, ability to show more detailed anatomy in some circumstances, and greater depiction of functional information. A disadvantage of MRI is the requirement for sedation or anesthesia in younger children who may otherwise be able to undergo a CT without the need for sedation or anesthesia.
Catheter Angiography
The use of diagnostic angiography in cases in which percutaneous intervention is not performed is dramatically decreasing because of improvements in noninvasive imaging tools, such as echocardiography, MRI, and CT. At the same time that the role of diagnostic angiography in the evaluation of congenital heart disease is decreasing, percutaneous interventional procedures, such as ductus arteriosus, atrial septal defect (ASD), and VSD closure device deployment, are increasing in number. Diagnostic angiography is commonly performed as part of these interventional procedures to define the anatomy of these abnormalities and provide procedure guidance.
Approach to the Chest Radiograph in Congenital Heart Disease
It is important to have a basic understanding of the radiographic findings of congenital heart disease because the radiologist may be the first to recognize that respiratory symptoms are secondary to cardiac rather than respiratory disease. In addition, understanding the radiographic findings provides a framework for understanding the pathophysiology behind congenital heart disease. When evaluating a chest radiograph in a patient with potential congenital heart disease, it is important to evaluate pulmonary vascularity, cardiac size, situs, and the position of the aortic arch.
Pulmonary Vascularity
An important radiographic feature for determining the appropriate differential diagnosis in congenital heart disease is the pulmonary vascularity. Unfortunately, it is probably also the most difficult radiographic finding to evaluate and one that can be altered iatrogenically by the administration of fluids or diuretics to a patient. In addition, the appearance of pulmonary vascular prominence can be increased by low lung volumes and portable radiographic technique. The pulmonary vascularity can be normal or can reflect increased pulmonary arterial flow, increased pulmonary venous flow, or decreased pulmonary flow.
In cases of increased pulmonary arterial flow, the pulmonary arteries appear too prominent both in size and in the number of visualized pulmonary arterial structures ( Fig. 4-4 ). A helpful rule is that if the right interlobar pulmonary artery is larger in diameter than the trachea, one should consider increased pulmonary arterial flow to be present. The prominent vascular structures seen in increased pulmonary arterial flow are very distinct and have well-defined borders. It can at times be difficult to differentiate increased pulmonary arterial flow from the increased peribronchial markings seen with reactive airway disease or viral pneumonia.

In cases with increased pulmonary venous flow, although the pulmonary vascular structures appear prominent in size and distribution, they are very indistinct and poorly defined ( Fig. 4-5 ). Increased pulmonary venous flow is akin to pulmonary venous congestion or mild pulmonary edema. In many cases, such as in left-to-right shunts, there is both increased pulmonary arterial flow resulting from left-to-right shunting and increased pulmonary venous flow due to congestive heart failure. If any of the pulmonary arteries in a particular case appear very well defined, it is important to consider at least a component of increased pulmonary arterial flow to be present.

In decreased pulmonary arterial flow, there is a paucity of visualized arterial structures throughout the lung ( Fig. 4-6 ).

Cardiac Size
Cardiac size may be normal or enlarged. In older children and adults there may be findings that suggest specific chamber enlargement. However, specific chamber enlargement may be difficult to ascertain in infants because they usually undergo an anteroposterior radiographic technique and have large thymus glands. It is for this same reason that measuring the transverse diameter of the cardiac silhouette and comparing it with the transverse diameter of half the thoracic base may overestimate cardiac size. In these infants the lateral view commonly offers greater insight into whether cardiomegaly is truly present than does the frontal view ( Figs. 4-7, A and B , and 4-8, A and B ). On the lateral view, if the posterior aspect of the cardiac silhouette extends over the vertebral bodies, cardiomegaly should be considered present.


Cardiac axis is the term given to the configuration of the apex of the heart; it indicates whether the apex points superiorly or inferiorly. If the cardiac apex is oriented superiorly, right-sided cardiac enlargement is suggested, and if the cardiac axis or apex is oriented inferiorly, left-sided cardiac enlargement is suggested.
Situs
Situs is defined as the relationship of asymmetric organs to the midline. Identifying disturbances in normal situs (the presence of heterotaxy syndromes) is important because they are associated with the presence of congenital heart disease. Situs should not be confused with the actual location of the heart within the thoracic cavity. Levoposition describes a heart mainly located in the left chest, whereas dextroposition describes a heart located primarily within the right chest. The term mesoposition is used to describe a heart located in the midline. The term dextrocardia strictly refers to a heart located in the right hemithorax with the base-apex relationship tilted rightward.
The important structures when evaluating situs on chest radiography are the cardiac apex, stomach bubble, and position of the liver. When the cardiac apex and gastric bubble appear on the same side, left or right, there is a much lower incidence of congenital heart disease than in cases in which the cardiac apex is on the opposite side of gastric bubble. When there is discordance between the side of the cardiac apex and gastric bubble, there is a near 100% incidence of congenital heart disease. Situs solitus is the name given to the normal configuration; it is associated with a 0.6% incidence of congenital heart disease. Situs inversus is the mirror image of normal and is associated with a 3% to 5% incidence of congenital heart disease. With situs ambiguous, there is no clear, straightforward left- or right-sidedness. The major types of situs ambiguous include asplenia (bilateral right-sidedness) and polysplenia (bilateral left-sidedness). Definitive determination of situs requires identifying the relationship between the atrial chambers and adjacent organs, which is not possible radiographically.
Asplenia ( Fig. 4-9, A and B ) is associated with complex, cyanotic congenital heart disease. Patients are susceptible to infections by encapsulated bacteria because of the lack of a spleen. Other abnormalities that may be present include malrotation, microgastria, and midline gallbladder. Radiographic findings include a midline liver, bilateral right-sided-appearing bronchi, decreased pulmonary arterial flow, azygous continuation of the inferior vena cava (IVC), and other findings reflecting the specific type of cyanotic heart disease

Polysplenia ( Fig. 4-10, A and B ) is typically associated with less complex acyanotic heart disease, usually left-to-right shunts. Other associations include azygous continuation of the IVC, bilateral superior vena cava (SVC), malrotation, and absent gallbladder. Radiographic findings include absence of the IVC shadow, prominent azygous vein, midline liver, and increased pulmonary arterial flow.

Position of Aortic Arch
The identification of a right-sided aortic arch should increase suspicion for the presence of congenital heart disease. The most common congenital heart lesions that have an associated right-sided aortic arch are tetralogy of Fallot, truncus arteriosus, tricuspid atresia, and transposition of the great arteries. When the aortic knob can be identified, as in most cases in adults and older children, it is obvious which side the aortic arch is on. However, in infants the aortic knob is often not easily identified. In such cases, secondary findings for the presence of the aortic arch must be used. Such findings include the position of the descending aorta (though this does not universally correspond with the side of the arch), tracheal displacement, and tracheal indentation. In a normal left-sided aortic arch, the trachea is displaced slightly toward the right as it moves inferiorly. Also in such cases there is an indentation on the left aortic border of the trachea as visualized on the frontal view of the chest. If the trachea deviates slightly leftward as it moves inferiorly or if there is a soft tissue indentation on the right aortic border of the trachea, a right-sided aortic arch should be suspected. A double aortic arch may manifest on a chest radiograph simply as a midline trachea with no indentation.
▪ Categorization of Congenital Heart Disease
In the traditional classification of congenital heart disease, two of the major features that place the disease into a particular diagnostic category include (1) whether the patient is cyanotic (blue) and (2) whether the pulmonary arterial flow is decreased, normal, or increased ( Table 4-1 ). Once these two major features have been identified, other radiographic findings will help to limit the differential diagnosis.
Another important factor to consider is the frequency of occurrence of the various types of congenital heart disease ( Table 4-2 ). Approximately 50% of cases of congenital heart disease are left-to-right shunts. Many of the types of congenital heart disease discussed here are highlighted because of striking anatomic findings but are actually quite rare. It is also important to remember that there are other systems for classifying congenital heart disease that are used by cardiac imagers, most commonly the segmental approach described by Van Praagh (see Suggested Readings ). The following discussion serves as a basic introduction to the classification of congenital heart teaching from a traditional radiography approach.
Blue, Decreased Pulmonary Arterial Flow, Mild Cardiomegaly
The differential diagnosis of patients who are cyanotic and demonstrate decreased pulmonary arterial flow on chest radiograph can be narrowed according to whether the patient has mild or massive cardiomegaly. In the cases in which the heart size is normal or there is only mild cardiomegaly, the differential diagnosis includes tetralogy of Fallot and pulmonary atresia with an associated VSD. These two entities are essentially different spectrums of the same disease.
Tetralogy of Fallot
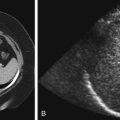
Tetralogy of Fallot is the most common type of cyanotic congenital heart disease in children. It is usually diagnosed by 3 months of age. There are four classic anatomic components of tetralogy of Fallot: (1) right ventricular outflow tract obstruction, (2) VSD, (3) overriding aorta, and (4) right ventricular hypertrophy. Radiographic features include a normal-sized to slightly enlarged cardiac silhouette with uplifting of the ventricular apex (a superiorly oriented cardiac axis) secondary to right ventricular hypertrophy The main pulmonary artery segment is concave because of the small associated pulmonary arteries. The combination of the deficient main pulmonary artery and the upturned cardiac apex makes the configuration of the cardiac silhouette appear to be boot shaped. The pulmonary vascularity is generally decreased. In tetralogy of Fallot the central pulmonary arteries may be confluent or nonconfluent. This is often difficult to evaluate with echocardiography, so MRI can be used to evaluate the status of the pulmonary arteries in patients with tetralogy of Fallot ( Fig. 4-11, A and B ). A right aortic arch is present in approximately 25% of tetralogy of Fallot patients (see Fig. 4-11, B and C ). Pulmonary atresia with a VSD is considered to be the most severe form of tetralogy of Fallot. It is synonymous with pseudotruncus or truncus arteriosus type 4 because of the larger bronchial arteries, or collaterals, arising from the aorta and supplying the lungs.