Acute myocardial infarction (MI)
Hibernating or stunned myocardium
Mechanical complications of MI
Papillary muscle rupture
Interventricular septum rupture
Left ventricular free wall rupture
Acute valvular regurgitation
Acute myocarditis
Septic cardiomyopathy
Myocardial contusion
Cardiac tamponade
Decompensated cardiomyopathies
As this constitutes an emergency with a very high mortality rate ranging from 50 to 80 %, early diagnosis and institution of appropriate treatment are pivotal to improving the prognosis. In the majority of cases, myocardial revascularization by percutaneous angioplasty or coronary bypass grafting will be required and hence transfer to a tertiary referral center may be necessary.
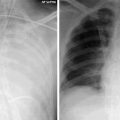
An important role of the CXR is to exclude alternative causes of shock such as a tension pneumothorax. It can also be used to assess severity of left ventricular failure which is characterized by features including cardiomegaly, redistribution of pulmonary blood flow to the upper lobes or signs of interstitial and alveolar edema, and bilateral pleural effusions (Fig. 25.1). Pulmonary interstitial edema is characterized by peribronchial cuffing, with thickening of interlobar fissures and development of interlobular septal lines or Kerley B lines which are short, 1–2 cm peripheral horizontal lines in the mid and lower zones. Opposed to this, pulmonary alveolar edema is characterized by bilateral alveolar opacification usually with a perihilar distribution. The CXR also permits checking the position and complications relating to placement of indwelling lines. It can be used to confirm the position of the intra-aortic balloon pump used for initial stabilization of patients with cardiogenic shock. The proximal balloon tip should ideally be in the descending thoracic aorta, about 1–2 cm distal to the origin of the left subclavian artery (Fig. 25.1).
Fig. 25.1
CXR from two different patients with cardiogenic shock. The left panel shows the CXR of a 60-year old male presenting with severe hypotension and respiratory distress requiring intubation. There is pulmonary edema as evidenced by widespread bilateral alveolar opacifcation and supine pleural effusions. The right panel shows that of a 75-year old patient who underwent treatment for shock post-cardiac surgery with good improvement in the radiographic appearances. Intra-aortic balloon pump catheter tip is projected immediately below the aortic knuckle (block arrow). Patient also has right jugular line, pulmonary artery flotation catheter and a nasogastric tube
Although non-invasive, EGG-gated cardiac CT is not an appropriate diagnostic tool to exclude acute coronary syndrome (ACS), particularly in the setting of cardiogenic shock. Catheter coronary angiography is the definitive tool for diagnosis of coronary disease with the possibility, where appropriate to angioplasty and stent to restore coronary blood flow. However, when alternative conditions such as pulmonary embolism or aortic dissection are being entertained as the potential cause of hypotension, CT can be used to solve the diagnostic conundrum. Once the patient’s condition has stabilized, Cardiac MRI can help to estimate the extent of myocardial scarring and viability.
Cardiac Tamponade
Cardiac tamponade is a potentially fatal clinical syndrome caused by compression of the cardiac chambers secondary to collection of fluid, blood, pus, air, or tissue within the pericardial space. The rise in intrapericardial pressure results in compromised diastolic filling and reduction in cardiac output. The rate of accumulation is more relevant than the size or content as the pericardial compliance is generally poorer with rapid collection.
The diagnosis of tamponade should be entertained in all patients with unexplained cardiogenic shock or pulseless electric activity. The common causes of tamponade are summarized in Table 25.2.
Table 25.2
Common causes of cardiac tamponade
8–10 % of patients with acute Stanford type A dissection of the thoracic aorta develop cardiac tamponade secondary to hemopericardium caused by aortic rupture |
Penetrating or blunt trauma |
Acute myocardial infarction with free wall rupture |
Dressler syndrome |
Malignancy |
Poorly controlled anticoagulation |
Uremia |
Heart failure |
Infection such as tuberculosis and HIV |
Chest wall radiation |
Iatrogenic injury secondary to procedural complications following pacemaker insertion, coronary intervention or cardiac surgery |
Cardiopulmonary resuscitation |
Echocardiography is the imaging modality of choice for diagnosis and assessment of the severity of hemodynamic compromise. CT plays a secondary role to echocardiography and should be considered only if the latter is equivocal or in cases of suspected hemorrhagic effusion, pericardial thickening or calcification.
Rapidly increasing cardiac size on serial CXRs is usually due to pericardial effusion (Fig. 25.2a). However, when the tamponade is due to pneumopericardium, there may be a marked reduction in the size of the cardiac silhouette with sharp outlining of the pericardium by radiolucent air on either side (Fig. 25.2b).
Fig. 25.2
(a, b) CXR from two different patients with pericardial tamponade. (a) A 67-year old male patient who had increasing cardio-mediastinal silhouette on post surgical serial chest radiographs. (b) Another post cardiac surgery patient with pneumopericardium (block arrows)
CT features are relatively non-specific: Table 25.3 shows the spectrum of findings that should raise the suspicion of tamponade.
Table 25.3
CT features in keeping with cardiac tamponade
Pericardial effusion causing compression and straightening of the right heart chambers
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|