Introduction
CT imaging of the heart plays an important role in anatomic and sometimes functional evaluation of the heart and coronary arteries. Coronary artery cardiac CT angiography (CTA) has substantially gained popularity, specifically for imaging acute chest pain in urgent care settings, allowing for a more rapid rule-out of acute coronary syndrome (ACS) and for imaging patients before and after coronary artery bypass graft (CABG) surgery. Before the imaging specialist interprets the images from a cardiac CT examination, it is important to understand the basics of image acquisition.
Basics of Cardiac CT
Electrocardiogram Gating
Electrocardiogram (ECG) gating allows for image acquisition during certain time points in the cardiac cycle. Usually, images are acquired during the later third of the R-R interval, which corresponds to cardiac diastole when the images will be subject to less motion artifact. There are three main types of ECG synchronization: (1) prospective triggering (axial, sequential); (2) retrospective gating (spiral, helical); and (3) retrospective gating with tube modulation ( Fig. 7.1 ). A newer type is a high-pitch spiral prospectively triggered acquisition, which requires a dual-source scanner.

In prospective triggering, images are acquired in a step-and-shoot fashion. The tube current is only applied for a specific percentage of the R-R interval, usually end-diastole. The minimum amount of time that the patient can be irradiated during the cardiac cycle is determined by the gantry rotation time. On single-source scanners, this is typically between 135 and 210 ms, and on dual source scanners this may less than 70 ms, depending on exact scanner type. When the minimum time for image acquisition is used, this results in a solitary image (frame) from a single time point during the cardiac cycle. If this image is blurred by motion artifact, images from other points in the cardiac cycle cannot be reconstructed. The amount of time a patient can be irradiated during the cardiac cycle can be increased so that additional images or frames can be reconstructed, but this increases radiation dose.
Therefore, prospective gating is ideally performed in patients with low, regular heart rates, ideally less than 60 beats/min, although some sites use this mode when the heart rate is less than 65 beats/min.
When prospective triggering is performed, the patient may be imaged every other heartbeat, as opposed to retrospective gating, which images each heartbeat. Between heartbeats, the table moves within the CT gantry to the next location of image acquisition. Therefore, prospective examinations usually take longer, resulting in a slightly longer breath-hold and the need for more IV contrast.
In retrospective gating, images are acquired throughout the cardiac cycle using a helical acquisition, producing a cine clip of heart motion. Images acquired during numerous points in the cardiac cycle can be used to measure function. In addition, images from various stages in the cardiac cycle can serve to display anatomy that may be blurred by motion artifact on some cardiac phases.
A variation of retrospective gating called retrospective gating with modulation also acquires images throughout the cardiac cycle, but the tube current is varied based on the cardiac cycle. This is typically used to produce low-noise images during diastole, allowing for visualization of the coronary arteries and higher noise, and lower dose images during the remainder of the cardiac cycle. This approach minimizes radiation dose, yet allows cardiac function to be evaluated.
Image Reconstruction and Analysis
Imaging reconstruction depends on whether prospective or retrospective gating is used. For example, for examinations using a CT scanner with a minimum slice thickness of 0.625 mm, prospective triggering may be reconstructed at a 0.625-mm slice thickness, with a 0.625-mm interval. When using retrospective gating, slices may be reconstructed at a 0.625-mm thickness but with a 0.3125-mm interval. In both cases, the field of view should be confined to the anatomy of interest, but there is little benefit in a field of view less than 15 cm. Images should be reconstructed using an appropriately smooth kernel, which will have a different name based on the CT vendor.
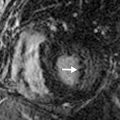
Reconstructed images can be reformatted in real time using a three-dimensional workstation. Coronary artery stenosis is best diagnosed using multiplanar reconstruction (MPR) images when the reformatted plane shows the vessel through-plane. Axial images are nearly as effective as MPR images for diagnosing coronary stenosis. Maximum intensity projection images should be used with caution when diagnosing coronary stenosis ( Fig. 7.2 ).

Common Indications for Imaging
Chest Pain
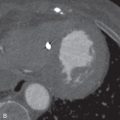
Chest pain is one of the most common indications for cardiac CT. Recently, multiple randomized trials have demonstrated that cardiac CTA has an excellent negative predictive value for excluding coronary artery disease for emergency department patients with chest pain. In low- to intermediate-risk patients, ACS can be safely excluded if there is no coronary artery stenosis greater than 50% ( Fig. 7.3 ).

Additionally, in the setting of a nondiagnostic cardiac stress test, cardiac CTA can provide information that may obviate the need for an unnecessary conventional coronary angiogram. If the cardiac CTA is normal in the setting of a nondiagnostic stress test, the patient often does not need to undergo conventional coronary angiography.
Sudden Cardiac Death
Sudden cardiac death (SCD) is defined as unexpected death occurring within a short time period from symptom onset. In patients for whom SCD has been successfully aborted, cardiac CTA can be used to diagnose structural heart disease–related causes. SCD in patients older than 35 years is usually due to coronary atherosclerosis and myocardial ischemia. In patients younger than 35 years, an anomalous coronary artery or a cardiomyopathy, such as arrhythmogenic right ventricular cardiomyopathy (ARVC), arrhythmogenic right ventricular dysplasia (ARVD), or hypertrophic cardiomyopathy, becomes more common. In the approximately 20% of SCD patients who have no structural heart disease, mostly represented by channelopathic disorders, cardiac CT does not yield a diagnosis.
Coronary Artery Disease Risk Stratification
Obtaining the coronary artery calcium score (CACS) using noncontrast cardiac CT has been shown to assist in the risk stratification of patients with atypical chest pain and asymptomatic patients with cardiovascular disease risk factors. CACS has been shown to correlate strongly with the risk of future adverse cardiac events and mortality.
The CACS inversely correlates with cardiac CTA performance for diagnosing coronary stenosis. In some cases, if a patient being evaluated for ACS has a calcium score >1000 Agatston units, cardiac CTA may be unreliable, and the patient will undergo conventional coronary angiography, regardless of the cardiac CTA findings.
Contraindications to Cardiac Catheterization
Cardiac CTA can be performed safely in patients who have a contraindication to cardiac catheterization. There are few contraindications to cardiac catheterization, but they include coagulopathy (both iatrogenic and intrinsic), uncontrolled systemic hypertension, unexplained fever, and/or untreated infection.
Coronary Artery Bypass Patency
Cardiac CTA is a noninvasive method for determining the patency of CABG surgery and for detecting complications following CABG, such as an aneurysm of the graft vessel. Using multidetector CT (MDCT), cardiac CTA has an excellent sensitivity (97%–100%) and specificity (98%) in determining if there is a stenosis in the bypass graft or the distal runoff vessel. Evaluation of the native vessels is more difficult due to the high prevalence of calcium and, often, stents.
Presurgical Planning
Cardiac CTA is often performed prior to initial cardiothoracic surgical intervention and in cases of reoperation. In cases prior to initial surgical intervention, cardiac CTA provides anatomic information that allows the surgeon to determine the best surgical approach for the desired sites of intervention. In patients undergoing reoperation, preoperative cardiac CTA provides information confirming the prior surgical interventions, as well as information used to decrease the risk of intraoperative and postoperative complications associated with the positioning of prior grafts within the thorax and their proximity to the expected access site (usually sternotomy or thoracotomy).
Problem-Solving Issues
Causes of Acute Chest Pain
Determining if Coronary Atherosclerosis Is Present
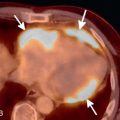
Cardiac CTA, specifically coronary CTA, can be used in the emergency department setting in patients with acute chest pain who are predetermined to have a low to intermediate risk for ACS. The risk for ACS is often calculated using the Thrombolysis In Myocardial Infarction (TIMI) score. A TIMI score of less than or equal to 4 is considered low to intermediate risk. The negative predictive value of a coronary CTA that does not demonstrate significant coronary artery stenosis, defined as less than 50% luminal stenosis, is 99%, allowing for the confident exclusion of ACS in this patient population (see Fig. 7.3 ). If a significant coronary artery stenosis greater than 50% is identified by coronary CTA, then the likelihood of ACS increases, and the patient should undergo an immediate workup for ischemic cardiac chest pain, such as cardiac catheterization ( Fig. 7.4 ). In all cases, the region of suspected stenosis should be measured by comparing it to an adjacent normal segment ( Fig. 7.5 ). Cardiac CTA can also be used to identify the sequelae of ischemia, such as true and false cardiac aneurysms ( Fig. 7.6 ).



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree