Cardiovascular System Scintigraphy
David K. Shelton
Nuclear medicine applications in the cardiovascular system include gated or nongated myocardial perfusion imaging (MPI), myocardial viability studies, infarction imaging, gated ventricular function studies of the blood pool in the ventricles, and detection and quantitation of intracardiac shunts.
Myocardial Perfusion Scans
Technique
Each of the perfusion agents may be imaged with planar techniques, SPECT, and now with SPECT-CT, which allows anatomic coregistration and attenuation correction. Meticulous quality control of the stress and rest images is essential. The comparison of images between stress and rest requires identical repositioning so that the same areas of myocardium are visualized. Poor positioning will lead to false-positive interpretations of ischemia and infarct.
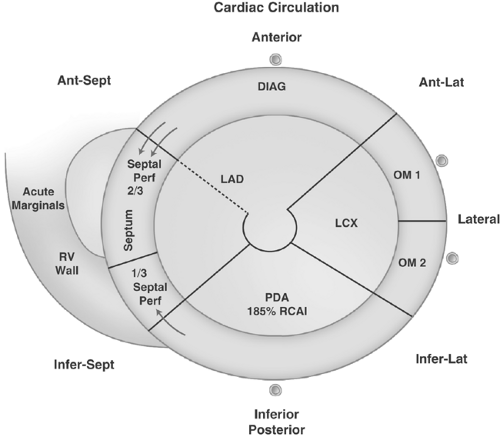
The three principle coronary artery distributions of the LV are the left anterior descending artery (LAD), the left circumflex artery (LCX), and the posterior descending artery (PDA). Each artery normally provides an equal intensity of myocardial labeling at any given level of cardiac work. Perfusion of the thinner right ventricular wall is considerably less than that of the LV, but can be imaged using the same techniques (Figs. 56.1 to 56.3).
Exercise on a treadmill, or simulation of exercise by infusion of dipyridamole or adenosine, is used in conjunction with perfusion agents to increase radionuclide delivery to the normal myocardium. Step-wise increases in physical exercise are monitored by sequential electrocardiogram (ECG), blood pressure, and pulse measurements, while the patient is queried for symptoms of angina. The radiopharmaceutical is injected under conditions of maximal exercise, which should be continued for 30 to 60 seconds after injection to obtain optimal mapping of stress perfusion. Exercise should reach at least 85% of the maximum predicted heart rate (MPHR) in order to achieve adequate stress.
One method for calculating MPHR is: MPHR = 220 – age. Exercise may also be stopped because of chest pain and ischemic changes on the ECG. Adequacy of the exercise challenge can more thoroughly be estimated simply from a calculation of the “double product” (DP) (systolic pressure × heart rate = DP). For exercise to be judged as adequate, the DP should at least double from rest to peak exercise, and should rise to above 20,000.
For those patients who cannot perform sufficient physical exercise, coronary vasodilatation can be pharmacologically induced. IV dipyridamole, adenosine, or regadenoson will vasodilate normal coronary arteries but do not effectively increase flow through vessels with 50% stenosis or greater. These stenosed coronaries, which cannot dilate normally, will appear to have decreased myocardial perfusion on stress when compared with the rest acquisition.
IV dobutamine can also be used when dipyridamole, adenosine, or regadenoson are contraindicated, such as active bronchospasm. Dobutamine has direct inotropic and chronotropic effects, which result in increased coronary flow similar to true exercise. Areas of relative hypoperfusion result from significant coronary stenoses greater than 50%.
Image Acquisition. Planar imaging has largely been replaced by SPECT imaging with reconstruction of the LV myocardium into short axis, vertical long axis, and horizontal long axis planes. A 180° acquisition is generally preferred over a 360° acquisition because of the asymmetry of the heart in the thorax and because of spine attenuation effects in the posterior projections. ECG-gated acquisitions are readily accomplished for technetium and thallium radiotracers, allowing evaluation of wall motion, brightening, and thickening from diastole to systole. Functional data acquisition has also become routine, allowing accurate calculations of end-diastolic volume, end-systolic volume, and left ventricular ejection fraction (LVEF). ECG-gated planar imaging can still be accomplished for patients who cannot be imaged on the SPECT table (often because of weight).
The tomographic images from SPECT have improved the accuracy of MPI and provide better correlation to other imaging modalities such as echocardiography, CT, and MRI. The addition of ECG-gated SPECT allows wall motion analysis and functional information which has improved interpretation and made MPI a more complete examination.
Prone imaging can be accomplished after the standard supine, post–stress acquisition, and may help reduce false-positive examinations because of breast or diaphragm attenuation, hot bowel loops, or motion artifacts. However, new hybrid
SPECT-CT cameras use the CT anatomic data to provide accurate attenuation correction, thus reducing artifacts. The SPECT camera itself can be a single-, a dual-, or a triple-headed camera.
SPECT-CT cameras use the CT anatomic data to provide accurate attenuation correction, thus reducing artifacts. The SPECT camera itself can be a single-, a dual-, or a triple-headed camera.
Radiopharmaceuticals
Three gamma-emitting radiopharmaceuticals are readily available for mapping the flow of blood or perfusion to the myocardium. Each has advantages and some disadvantages.
Thallium-201 (Tl-201), an analog of the potassium ion (K+), is delivered to capillary beds by regional blood flow and is actively pumped into viable cells by the sodium/potassium (Na+/K+) adenosine triphosphatase pump. Cyclotron production at a remote site (requiring shipping), a long physical half-life (73 hours), low energy, poorly penetrating photons (mostly 69- to 83-keV γ-rays), and a relatively high-absorbed dose (0.24 rad/mCi whole body at the usual dose of 2 to 5 mCi) combine to make Tl-201 a less than ideal agent for imaging. However, because of its active transport into cells, it is a more physiologic radionuclide than the technetium-99m (Tc-99m)-labeled agents.
A widely used technique uses Tl-201 with exercise stress or a pharmacological challenge. Images are usually acquired soon after injection as possible. However, some authors advocate waiting for 5 to 10 minutes to allow the exercised patient to stop breathing heavily so that the movement of the heart heaving up and down with the diaphragm will be minimized. This slight delay also limits an artifact caused by the “upward creep” of the heart. As the lungs decrease in volume slowly after exercise, the average level of the diaphragm is raised, shifting the heart upward. This shift in location of the heart produces an artifactual shift in radionuclide activity that may be misinterpreted as ischemia.
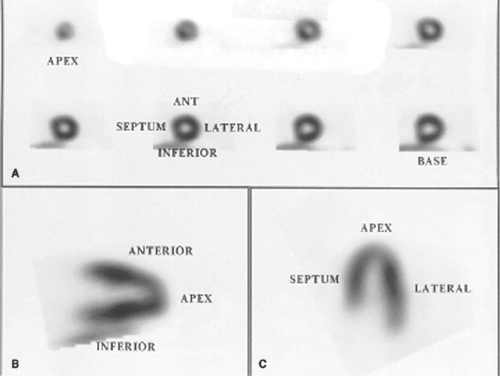 Figure 56.2. Normal SPECT Pro-jections. Short axis (A), vertical long axis (B), and horizontal long axis (C) images in standard projections show the walls of LV. In the short axis images, an apical “button” starts the series, which extends back to the base of the ventricle. The names of the walls for the short axis images are best given by the diagram in Figure 57.3. In the vertical long axis images, the anterior and inferior (or posterior) walls are seen. In the horizontal long axis images, the short septum and long lateral or “free” walls are well seen. The long axis images also show the apex very well. |
The effective half-life (T1/2), or 50% washout, of Tl-201 from the normal myocardium is about 4 hours. A complex “redistribution” of the isotope within the myocardium is governed by rates of washout from myocardial cells, renal excretion, and shifts of the isotope between muscle, visceral, and other compartments. Rest or redistribution imaging is usually
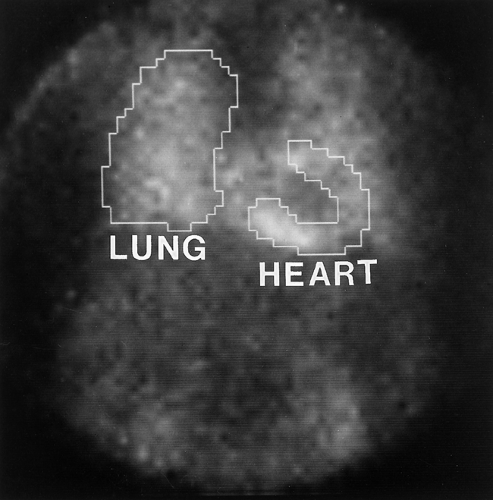
done 3 to 4 hours after the stress injection. Because Tl-201 has significant blood pool activity, it can slowly redistribute into the myocardium and thus slowly fill in ischemic-type defects. In addition to clinical data (ECG, angina, etc.), the initial Tl-201 images of the chest and heart may help assess the heart’s performance. High lung activity immediately after exercise usually indicates that left ventricular failure occurred during exercise. Poststress dilation of the heart compared with the resting images is another indicator of failure. Both phenomena have a severe prognosis for subsequent cardiac events (angina, infarction, arrhythmia, and sudden death) (Fig. 56.4). Another imaging strategy for improving the visual detection of ischemic myocardium by Tl-201 scintigraphy calls for a “reinjection” of 1 mCi of Tl-201 just before delayed, rest imaging. This technique is especially important to fill in defects caused by very high-grade stenoses, resulting in more accurate diagnosis of ischemia versus infarction.
done 3 to 4 hours after the stress injection. Because Tl-201 has significant blood pool activity, it can slowly redistribute into the myocardium and thus slowly fill in ischemic-type defects. In addition to clinical data (ECG, angina, etc.), the initial Tl-201 images of the chest and heart may help assess the heart’s performance. High lung activity immediately after exercise usually indicates that left ventricular failure occurred during exercise. Poststress dilation of the heart compared with the resting images is another indicator of failure. Both phenomena have a severe prognosis for subsequent cardiac events (angina, infarction, arrhythmia, and sudden death) (Fig. 56.4). Another imaging strategy for improving the visual detection of ischemic myocardium by Tl-201 scintigraphy calls for a “reinjection” of 1 mCi of Tl-201 just before delayed, rest imaging. This technique is especially important to fill in defects caused by very high-grade stenoses, resulting in more accurate diagnosis of ischemia versus infarction.
Tc-99m is used to label two commercially available myocardial perfusion agents.
Tc-99m sestamibi (trade name Cardiolite) is taken up by the perfused myocardium by passive diffusion and is bound in the myocyte, mostly within myocardial mitochondria. There is no significant redistribution effect with this agent. Washout is negligible. Imaging of the 15 to 20 mCi dose is delayed for 30 minutes to 1 hour after stress to allow for biliary and background clearance. Because there is neither redistribution nor significant washout of Tc-99m sestamibi, a repeat injection of 15 to 20 mCi for resting images is commonly performed on a different day. With this 2-day protocol, stress imaging is usually done first. An alternative 1-day protocol uses a small dose (8 mCi) for the initial rest scan, followed 4 hours later by the stress scan with a larger dose of 20 to 25 mCi.
Tc-99m tetrofosmin (trade name Myoview) is rapidly extracted from the blood by perfused myocardium in a fashion that resembles Tc-99m sestamibi. The two agents have proven to act clinically in a very similar manner, but availability and pricing make important considerations.
Both of the Tc-99m-labeled agents are prepared from Tc-99m pertechnetate and stocked pharmaceutical kits. Both are easy to image radiopharmaceuticals with good soft tissue penetration (140-keV gamma energy) and a high photon flux from typical doses of 8 to 25 mCi. In addition, the Tc-99m agents also provide perceptibly improved image quality and an opportunity with the same injection to better perform gated first pass or gated SPECT studies, which can be used to evaluate wall motion, and left ventricular functional parameters such as LVEF.
Dual Isotope Myocardial Scans. An innovative way to maximize the logistical patient throughput involves the use of a Tl-201 and a Tc-99m agent for sequential scans. The most widely used dual isotope scan technique uses a resting Tl-201
scan which can be immediately or subsequently followed by a Tc-99m (sestamibi or tetrofosmin) stress scan. Because the energy and photon flux of the subsequent Tc-99m scan is higher than the Tl-201 scan, there is no problem with cross talk between the rest and stress images. Excellent scan quality can be combined with this 1-day protocol. When needed, a delayed 24-hour redistribution, thallium scan can be accomplished to evaluate a “fixed defect” for hibernating myocardium versus infarct.
scan which can be immediately or subsequently followed by a Tc-99m (sestamibi or tetrofosmin) stress scan. Because the energy and photon flux of the subsequent Tc-99m scan is higher than the Tl-201 scan, there is no problem with cross talk between the rest and stress images. Excellent scan quality can be combined with this 1-day protocol. When needed, a delayed 24-hour redistribution, thallium scan can be accomplished to evaluate a “fixed defect” for hibernating myocardium versus infarct.
Interpretation
Myocardial Ischemia. Interpretation of myocardial perfusion scans is difficult but important. Subtle abnormalities can signal serious coronary artery disease (CAD). Observer knowledge and experience is essential for an accurate diagnosis. Parametric methods of perfusion image analysis have been employed in attempts to standardize diagnosis. Circumferential profiles of isotope distribution and analyses of regional rates of Tl-201 washout, compared with normal databases, make interpretation more sensitive in the detection of ischemia. Displayed as graphic data, “bull’s-eye” maps of SPECT images, and three-dimensional reconstruction of SPECT data, these aids in interpretation may be overly sensitive. If an abnormality is truly present, it should also be visible in the planar or SPECT images. Depending on the statistical assumptions used and the population studied, the sensitivity and specificity for detecting myocardial ischemia are in the percent range of the high 80s or the low 90s. It is important to remember that according to Bayes’ Theorem, the positive and negative predictive values of a test will vary according to the prevalence of disease in the population being tested. The myocardial perfusion scan also detects other causes of ischemia (including left bundle branch block, coronary vasculitis, and small vessel disease), which cannot be seen on coronary arteriography and thereby reduce its apparent specificity. In addition to detecting significant CAD, the presence and severity of ischemic myocardium correlates strongly with the prognosis for adverse cardiac events including angina and cardiac death (Fig. 56.5).
MPI demonstrates relative regional perfusion. Areas of myocardium with poor blood supply, usually because of atherosclerosis, fail to increase radiotracer uptake during the stress component. Thus, an area of decreased perfusion or uptake at stress, which reverses or is normal at rest, is typical of what is called reversible ischemia. Reversible changes detected by either exercise or pharmacological dilation of normal vessels usually correspond with coronary stenoses greater than 50% and are considered ischemic but viable myocardium. Correction of the anatomic abnormality by angioplasty, laser atherectomy, or coronary artery bypass surgery is expected to relieve the ischemia and the reversible changes. Another frequent location of ischemic tissue can be seen immediately adjacent to an area of infarct. This is called peri-infarct ischemia and does not portend the same clinical significance as an ischemic or reversible zone.
Short axis summary presentations of myocardial perfusion are often presented in a “bull’s-eye” format similar to that in Figure 56.3. In addition, many computer programs will present the perfusion data in a semi-quantitative method. One such program uses a 20-segment model, which divides the short axis bull’s-eye into 20 segments, and grades each segment on a scale of 0 to 4. In this method, 0 is normal, 1 is mildly reduced, 2 is moderately reduced, 3 is severely reduced, and 4 is absent of activity. A summed stress score (SSS) is then calculated for the stress data as a whole. In a similar fashion, a summed rest score (SRS) and then a summed difference score (SDS) are calculated. While not infallible, the SSS is a very good, objective method to quantify the severity of the ischemia and to communicate with clinicians. A SSS of less than -4 is normal, 4 to 8 is mild, 9 to 13 is moderate, and more than 13 is severe.
Some patients will have naturally recruited coronary collaterals or bypass grafts that produce apparent discrepancies between angiographic and scintigraphic studies. Abnormal anatomy in a coronary artery may not produce hemodynamically significant changes in blood flow to the myocardium and not all ischemia is produced by large vessel atherosclerosis. Capillary disease in diabetics, left bundle branch block, vasospasm, vasculitis, or cardiomyopathy (dilated or hypertrophic) may produce ischemic myocardium even with normal arteries. Ischemia may not be detected if there is inadequate exercise, inadequate pharmacological challenge, or balanced triple vessel disease. Fortunately, it is uncommon for all three coronary arteries to be hemodynamically compromised equally, and poststress dilation or decrease in LVEF will usually be present.
Hibernating Myocardium. Severe ischemia with high-grade stenosis may be so slow to “reverse” on Tl-201 imaging that it will not be detected by rest or redistribution images at 3 to 4 hours after stress. Imaging at 24 hours, or a Tl-201 second injection rest study, may be required to detect extreme ischemia secondary to very high-grade stenoses. The Tc-99m-labeled agents are routinely given as two separate injections and there is no significant washout or redistribution. Evidence has shown that rest-injected Tl-201 with delayed imaging is the best SPECT technique for detecting the severe ischemia that leads to a phenomenon known as hibernating myocardium. Hibernating myocardium is important to diagnose as it occurs with high-grade stenoses and simulates infarction by not contracting even at rest. It remains viable, however, because of collateral circulation, and will return to normal function after revascularization (Fig. 56.6). Hibernating myocardium can also be evaluated with PET FDG or contrast-enhanced MRI.
Myocardial infarction produces layers of nonperfused scar tissue which are detected as areas of thin myocardium with
decreased radiotracer uptake at both stress and rest imaging. The extent of an infarct, from subendocardial to transmural, is reflected by the size and degree of the perfusion defect (Fig. 56.7). Technical artifacts from attenuation of the perfusion agent’s radiation may be produced by breast tissue, arm positioning, and subdiaphragmatic structures. These may appear as fixed defects superimposed on planar or SPECT images. This may lead to a false-positive reading of infarction. A false-positive interpretation of ischemia should not occur as long as the artifact does not change between stress and rest imaging.
decreased radiotracer uptake at both stress and rest imaging. The extent of an infarct, from subendocardial to transmural, is reflected by the size and degree of the perfusion defect (Fig. 56.7). Technical artifacts from attenuation of the perfusion agent’s radiation may be produced by breast tissue, arm positioning, and subdiaphragmatic structures. These may appear as fixed defects superimposed on planar or SPECT images. This may lead to a false-positive reading of infarction. A false-positive interpretation of ischemia should not occur as long as the artifact does not change between stress and rest imaging.
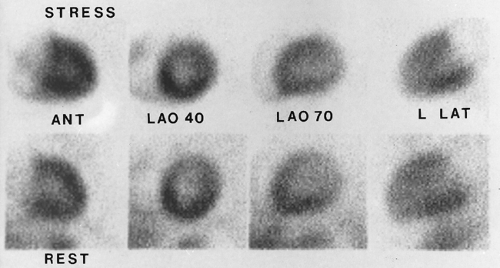
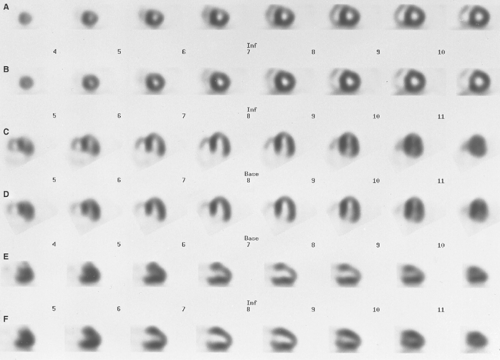 Figure 56.5. SPECT of Left Anterior Descending Artery Reversible Ischemia. The row of short axis stress images (A) has a perfusion defect in the anterior wall (arrows) which perfuses normally in the rest of short axis images (B). This is also visible in the horizontal long axis stress (C) and vertical long axis stress images (E) which have the same perfusion defect (arrows). At rest, the matched images (D, E, F) show normal perfusion.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|