Fig. 14.1
Cartilage degeneration in late stage of OA disease with complete loss of femoral and acetabular cartilage (white arrows)
There are different imaging protocols and approaches in detecting cartilage lesions of the hip using MRI; however, there is one common element for all protocols—high resolution. It is difficult to separate the femoral cartilage from the acetabular cartilage layer because of the thin cartilages of the femoroacetabular joint and the circumferential geometry, hence high image resolution is the key!
Current Status MR Imaging of Hip Joint Cartilage Damage
Compared with the well-established techniques for detecting osteonecrosis and for evaluating the acetabular labrum, techniques for assessing cartilage lesions in the hip have been disappointing. As in the detection of acetabular labrum lesions, both non-contrast techniques and MR arthrography are used.
Non-contrast techniques, using two- and three-dimensional sequences, analyze mainly thickness patterns to detect osteoarthritic changes [5]. The sensitivity for these measurements is reported to be 47 % for grade 1 lesions and 49 % for grade 2 lesions. The low diagnostic sensitivities suggest that these measurements are more useful in follow-up studies. Mintz et al. [6] also tried to classify cartilage based on cartilage thickness and signal intensity changes according to the Outerbridge score, but the results were unreliable. Therefore, they compared only grades 1 through 3 lesions to no lesion (grade 0) for sensitivity and accuracy. Thus, the results are comparable to thickness measurement studies with the same limitations.
With the use of MR arthrography, the detection of cartilage lesions can be improved. Schmidt et al. [1] assessed improvement in cartilage diagnosis using MR arthrography, but the classification within this study was done without staging or grading, and the sensitivity was only moderate (47 %). Additionally, the analysis was limited by low spatial resolution, restriction to two-dimensional imaging, and low signal-to-noise ratio due to field strength of only 1.0 or 1.5 T; hence, it was not possible to separate the femoral and acetabular cartilages. High interobserver variability was reported.
Beaule et al. [7] investigated cartilage delamination using MR arthrography and its correlation with intraoperative findings in four patients. They classified surgically observed cartilage delamination using the Beck classification. Beaule et al. found that MR arthrography was only able to detect a cleavage lesion (with a frayed edge). MR arthrography did not detect debonding, which is where the cartilage appears macroscopically sound but is detached from bone (carpet phenomenon). This carpet lesion is an early phase of chondral damage seen in patients with FAI. Therefore, early detection of cartilage degeneration appears limited using MR arthrography in FAI.
Pfirrmann et al. [8] showed high specificity for detecting cartilage lesion in patients with FAI by detection fluid under the cartilage delamination; however, sensitivity is low. Hypointense areas in the acetabular cartilage seen on intermediate-weighted fat-saturated or T1-weighted images appear to be helpful diagnostic criteria.
Overall, the cartilage diagnosis in the hip is limited so far and no reliable staging and grading system has been established. However, using dedicated coils and high-resolution imaging, the delamination of the cartilage as described by Beaule and Pfirrmann can be detected with high specificity (Fig. 14.2).
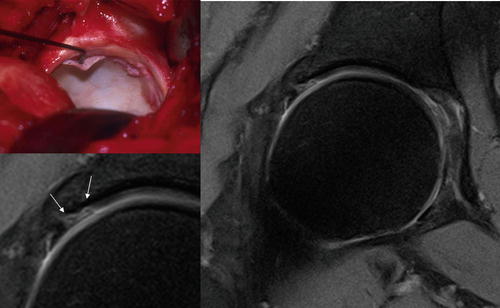
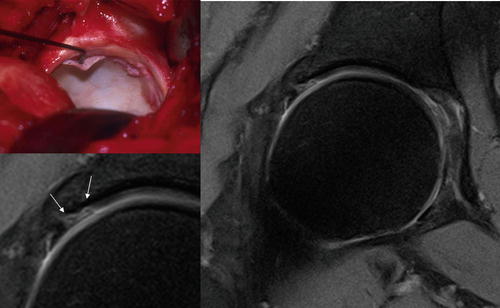
Fig. 14.2
Cartilage delemination in patient with femoroacetabular impingement. Diagnosis by high-resolution non-contrast PD TSE sequence (0.3 × 0.3 × 3 mm) at 3 T using fat saturation
Cartilage Damage Detection Using Leg Traction
One method to overcome the limitation of assessment of cartilage damage in the hip is to separate the femoral and acetabular cartilages with the use of traction as described by Llopis et al. [9]. They showed the potential advantage of applying manual traction followed by gentle leg traction during MR arthrography of the hip. Such traction produces enough space for the intra-articular contrast agent to enter the tight central compartment. This combination of contrast agent and additional space allows visualization of the cartilage surfaces as distinct entities. The limited traction is well tolerated and can be applied in a short time without specialized equipment. The arbitrarily chosen 6 kg of traction is well within the traction force used during arthroscopy, and no adverse effects such as transient neuropraxia occurred.
MR Imaging at 3 T
Recent developments in high-resolution and cartilage-specific imaging, including the introduction of novel sequences, local gradient and radio frequency coils, and high field strength, have improved the diagnostic potential of MRI to depict different structural and compositional characteristics of articular cartilage and are therefore focused on improving characterization of morphological and structural changes. Besides novel MR sequences, imaging quality can mainly improved by using higher field strengths because they provide a higher intrinsic SNR—critical for high-resolution imaging. There are preliminary studies published on the use of 3 T imaging in the hip revealing the capability of improvement in cartilage diagnosis due to high-resolution imaging and, in addition, the possibility of accurate hip imaging without the need for contrast agent.
Figures 14.3 and 14.4 show examples of high-resolution proton density (PD) weighted TSE (with and without fat saturation) imaging at 3 T without the use of contrast agents. Visualization of acetabular and femoral cartilage separation as well as assessment of the acetabular labrum and adjacent cartilage, essential for precise diagnosis of FAI, can be improved by using high-resolution techniques (Figs. 14.5 and 14.6




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree