CERVICAL ESOPHAGUS: BENIGN AND MALIGNANT TUMORS
KEY POINTS
- Computed tomography and magnetic resonance imaging detect cancers that may explain odynophagia, dysphagia, and vocal cord paralysis that cannot be found by any other means.
- Imaging is critical to medical decision making in these uncommon malignancies.
- As well, imaging is critical to medical decision making in the more common circumstances when malignancies of the thyroid gland, hypopharynx, larynx, and trachea secondarily invade the esophagus.
- Fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) may play an important role in selected patients with a malignant tumor.
The basic staging and medical decision-making procedures for cervical esophageal tumors including cancer include endoscopy with biopsy, contrast-enhanced computed tomography (CT) or contrast-enhanced magnetic resonance (MR) depending on the practice preference, and a chest x-ray. The imaging studies are essential in this clinical-diagnostic evaluation, providing unique and often pivotal information. Imaging provides additional information concerning the deep extent and regional spread of disease. Chest CT and FDG-PET are necessary in selected cases.
This chapter describes the important role of diagnostic imaging in clinical decision making with regard to cervical esophageal benign tumors and cancers. Squamous cell carcinoma (SCCA) will be the main focus. The much less common malignant tumors are rare in the cervical esophagus and have essentially the same growth patterns, with the exception of likelihood of spread to regional lymph nodes, so they will be discussed in conjunction with SCCA. The even more rare benign tumors will be included in the same discussion since they really cannot be distinguished from malignancies until biopsy or removal unless there is some overt sign of malignancy such as distant metastases, metastatic lymph nodes, aggressive infiltrating morphology, and/or perineural spread.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Applied Anatomy
A thorough knowledge of the following anatomy and anatomic variations of normal in each of the these areas is required for the evaluation of cervical esophageal tumors. This anatomy is presented in detail with the introductory material on the cervical esophagus, hypopharynx, larynx, and infrahyoid neck in general.
Primary Site Evaluation
- With regard to the cervical esophagus and hypopharynx, a detailed knowledge of the relationship of the cervical esophagus to the hypopharynx, larynx, and pyriform sinus apex region is required. The relationship of the postcricoid region of the hypopharynx and esophageal verge must be completely understood. The relationship of the upper cervical esophagus to the upper trachea, thyroid gland, and recurrent laryngeal nerve is important adjunctive information (Chapters 201, 209, and 221).
- With regard to the larynx, the relationship of mucosal landmarks and functional structures of the esophageal verge to the laryngeal attachments of the postcricoid hypopharynx musculature is critical knowledge for assessing tumor spread in this region. This fund of knowledge must include the detailed anatomy of the lower laryngeal skeleton and its normal variations (Chapters 149, 201, and 221).
Evaluation of Extraesophageal Spread
- Visceral compartment of the neck and related fasciae as well as the lateral compartment of the neck and carotid sheath (Chapter 149).
Evaluation of Regional Lymph Node Disease
- Detailed knowledge of normal node and perinodal morphology and the common drainage pathways of esophageal cancer, which emphasizes nodal levels 2 through 6 (Chapters 149 and 159).
Evaluation of Perivascular and Perineural Spread
- Knowledge of the entire course of the vagus and recurrent laryngeal nerves on both sides (Chapter 201).
IMAGING APPROACH
Techniques and Relevant Aspects
The cervical esophagus, as studied specifically for known cancers or masses of uncertain etiology, is imaged with MR and CT in the same manner as the larynx and hypopharynx are studied for these indications, except the study is continued to the carina to cover that segment of the esophagus and the contiguous mediastinal lymph nodes. The principles of using these studies are reviewed in Chapter 201. Specific problem-driven protocols for CT and magnetic resonance imaging (MRI) are presented in Appendixes A and B.
There is little or no use for ultrasound in studying the esophagus unless endoluminal ultrasound is considered, but the use of that technique is beyond the scope of this resource.
The approach with radionuclide studies depends on the aim of the examination. Most of the current usage is limited to known or suspected cancer evaluation with FDG-PET. Specifics of the use of this physiologic imaging in relation to anatomic imaging are discussed in Chapter 5 in general and in a manner that relates more specifically to the esophagus in Chapter 206. In summary, the use of FDG-PET should be thoughtful and selective rather than “routine.”
Pros and Cons
Indications for Study in Potential Cervical Esophageal Cancer
Evaluation of the Primary Site and Regional Disease
Almost all cervical esophageal tumors are studied with imaging, often with both MR and CT. The potential primary tumor and all cervical and upper mediastinal nodes must be studied. MR study is best used in a frequent supplemental role as directed by CT findings to localized areas of interest.
CT and MR are frequently used to mainly define the full extent of intraluminal and extraluminal disease in a known cancer that may primarily or secondarily involve the cervical esophagus. CT and MR may show muscular wall invasion extending well beyond the visible mucosal extent of the tumor as perceived at endoscopy (Figs. 223.1–223.10). MR is superior to CT for that task, assuming adequate image quality. This ability of MR and, to a lesser extent, CT reflects the known tendency for “skip metastases” in primary esophageal SCCA. The submucosal extent of tumor is best appreciated on T2-weighted or contrast-enhanced T1-weighted MR images. Complete assessment of extraluminal spread may require a combination of MR and CT scanning. MR demonstrates tracheal and thyroid gland invasion, spread to the postcricoid region, and the relationship of tumor to the brachiocephalic vessels (Fig. 223.9). CT is preferable to MR for evaluating nodes and the status of the thyroid and cricoid cartilages. A preferred approach is to use MR first, with CT used to evaluate the neck and mediastinal nodes and laryngeal skeleton when necessary. Both studies can help to differentiate primary tumor from adjacent tracheoesophageal groove nodes, but MR is usually more definitive than CT in this regard.
Detection of Recurrent Tumor
Diagnostic CT or MR may be used as the primary examination for detection of recurrence in the nodes or at the primary site or reconstructed esophagus; in selected cases, supplemental FDG-PET can be very helpful.
Evaluation of Cervical Esophageal Dysfunction and Submucosal Masses
Some patients have SCCAs growing entirely beneath intact mucosa. Rarely, these tumors may arise out of sight of the endoscopist, spreading mainly within the esophageal wall (Figs. 223.1–223.3). Submucosal masses are rarely caused by other submucosal cancers, such as those from minor salivary glands discussed in Chapter 22 (Fig. 223.3) and benign mesenchymal tumors (Fig. 223.8) discussed in Chapter 35, that cannot be distinguished from SCCAs. Benign tumors of the same cell lines often cannot be distinguished from the malignant varieties. These usually present with odynophagia and/or dysphagia or occasionally as vocal cord dysfunction because the tumor has involved the recurrent laryngeal nerve or larynx.
Controversies
FDG-PET for Initial Evaluation and Surveillance
In most cervical esophageal cancer, FDG-PET has a mainly adjunctive role to play, as this technique does not allow one to reliably assess the anatomic extent of the lesion and the possible invasion of the tumor into adjacent structures. FDG-PET may show “skip” lesions in the esophagus and otherwise occult metastatic mediastinal and cervical metastatic disease. A negative FDG-PET study does not exclude nodal disease in the neck or mediastinum, so possible nodal metastases must be accounted for in the treatment plan regardless of their FDG-PET status. The issues surrounding its value are discussed in general in Chapter 5, and in this particular area of interest, the issues are similar to those for laryngeal and hypopharyngeal SCCA and other malignancies and are discussed in that light in Chapter 206. This technique must be used with discernment rather than routinely applied for diagnosis and staging given its expense and sometimes limited potential to truly alter management or effect outcome in a positive manner.
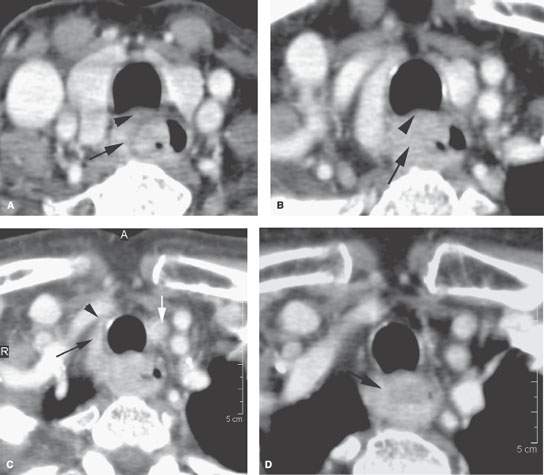
FIGURE 223.1. Contrast-enhanced computed tomography study of an entirely submucosal squamous cell carcinoma of the cervical esophagus. The patient presented with dysphagia. In (A), the tumor invades outside the muscular wall of the esophagus (arrow) and likely invades the common membranous wall between the trachea and esophagus (arrowhead). This pattern continues in (B). In (C), the mass invades along the lateral wall of the trachea (black arrow), coming very near to the brachiocephalic artery (arrowhead). There is a metastatic left level 6 lymph node (white arrow). In (D), the tumor spreads inferiorly both within and outside the muscular wall of the esophagus.
SQUAMOUS CELL CARCINOMA, OTHER MALIGNANT TUMORS, AND BENIGN TUMORS OF THE CERVICAL ESOPHAGUS
Etiology
Alcohol, tobacco, and a previous head and neck cancer are known risk factors for esophageal SCCA. The effects of alcohol and tobacco are likely synergistic as causative influences. The Plummer-Vinson syndrome is a rare but acknowledged risk factor in Scandinavian and British women.
Other cancers are sporadic and rare and have no consistent etiology. Adenocarcinoma of the lower esophagus is related to gastric reflux and chronic inflammation; this is not applicable to the cervical esophagus.
Benign tumors have no specific etiology.
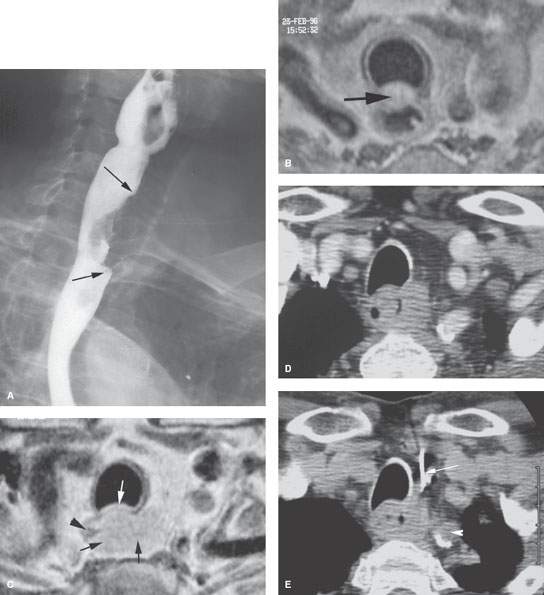
FIGURE 223.2. A patient presenting with dysphagia. In (A), barium swallow shows a submucosal mass in the cervical esophagus (arrows). Contrast-enhanced T1-weighted magnetic resonance images in (B) show that the cancer invades the common wall between the trachea and esophagus (arrow). In (C), the white arrow shows continued invasion of the membranous wall of the trachea and submucosal spread throughout the muscular wall of the esophagus (black arrows) except for a small portion remaining normal on the right (black arrowhead). Several endoscopic attempts at biopsy were unsuccessful. In (D) and (E), the tumor mass is identified on computed tomography for imaging-guided biopsy, which returned squamous cell carcinoma. In (E), the path of the biopsy needle (arrow) is shown, which safely avoids the common carotid artery (arrowhead).
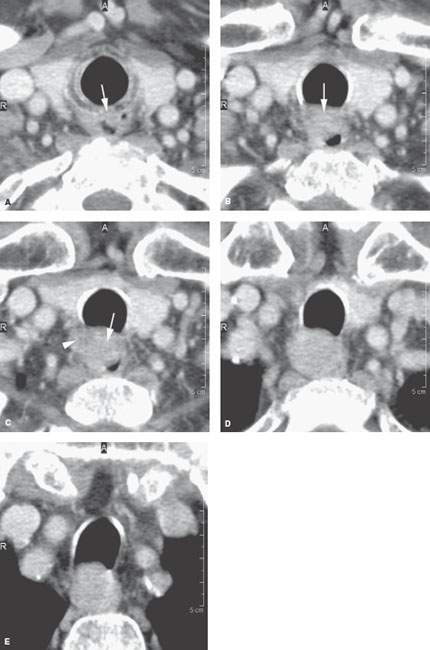
FIGURE 223.3. A patient presenting with dysphagia. Two endoscopic examinations were negative. Barium swallow was negative. Contrast-enhanced computed tomography was done and showed an infiltrating mass involving the cervical esophagus. A: The mass invades the lower margin of the cricoid cartilage (arrow). B: The mass clearly involves the anterior wall of the cervical esophagus and common wall between the esophagus and trachea (arrow). C: The primary tumor (arrow) continues the spread pattern (arrow) seen in (A) and (B), and there could be an adherent level 6 lymph node present as well (arrowhead). D, E: There is continued distal spread within the muscular wall of the esophagus and involving the membranous wall of the trachea without other evidence of level 6 adenopathy. (NOTE: Endoscopic biopsy was not successful. The lesion was biopsied with CT guidance and returned adenoid cystic carcinoma.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








