CERVICOTHORACIC JUNCTION AND BRACHIAL PLEXUS: DEVELOPMENTAL CONDITIONS
KEY POINTS
- The origin of a cervicothoracic junction condition is often not well understood from the physical examination and may be considered threatening to one or more important and sometimes vital functions until its benign and possible congenital nature is established.
- Imaging can most often provide a very likely diagnosis and help to establish the relative acuity of the situation.
- Imaging is critical to proper medical decision making beyond the diagnosis.
- Imaging-guided biopsy may be useful in more difficult diagnostic cases when something other than a development mass is likely.
The general approach to mass lesions in cervicothoracic junction (CTJ) and brachial plexus is presented in Chapter 163, and that should be reviewed at this time if necessary. This chapter reviews the developmental conditions that occur in the low neck–thoracic inlet region in both pediatric and adult patients.
The majority of developmental low CTJ masses arise from the visceral and lateral compartments of the neck; few involve the brachial plexus. Such developmental masses are frequently transcompartmental because they follow migrational or natural growth pathways of the structures of origin, making a strict compartmental or spatial approach to diagnosis imperfect from the outset. The method of first considering a space or compartment of origin in the diagnostic process is therefore meant to serve only as a starting point. This basic means of organization for diagnosis and, more importantly, for clinical problem solving and disposition can then provide a framework to analyze a CTJ mass of uncertain, but possibly congenital, etiology.
One could consider tumors that are present at birth or in early infancy as developmental in nature; however, in this resource, neoplasms—even when this early in life—are considered in the context of tumors.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS IN DIFFERENTIAL DIAGNOSIS
Embryology
Venolymphatic malformations arise in conjunction with venous and lymphatic system development. As such, they may originate from any compartment and freely spread between compartments along the pathways of vascular development. These relatively common malformations are by this mechanism the most ubiquitous of the transcompartmental benign masses encountered in the low neck and thoracic inlet (Fig. 164.1). These are discussed in more detail in Chapters 9 and 154.
Disorders of branchial apparatus development may be the source of a mass. This embryology is discussed and illustrated more completely in Chapter 153. Thymic migration follows the path of the third branchial apparatus from the level of the carotid bifurcation in the lateral compartment to the midline in the low neck and terminating in the mediastinum; thus, various iterations of thymic remnants may present in the low neck and thoracic inlet (Figs. 153.16 and 164.2). CTJ masses may also be related to other branchial cleft or pouch dysgenesis, with a prime example being the infected pyriform sinus tract or third branchial cleft cyst and related tracts that most frequently present as an infection in the low neck around the thyroid gland (Fig. 153.15).
Duplication cysts of the foregut and neuroenteric cysts may be a rare cause of a thoracic inlet mass (Fig. 150.11 and Chapter 10). More commonly, cysts and “celes” related to the pharynx, such as various diverticuli, will occur at sites of natural weaknesses at developmental boundaries between muscles or along penetrating neurovascular bundles (Fig. 164.3).
Rests of germ cell layer tissue may produce epidermoid, dermoid, and teratomatous masses (Chapter 9) in the low neck and thoracic inlet (Figs. 150.11 and 164.4). Rests of salivary gland tissue are also left within the deep spaces of the head and neck during development. These may give rise to both benign and malignant salivary epithelial tumors at virtually any neck level, but these are very rare at this level (Fig. 156.10).
Neurologic developmental abnormalities such as those arising from neural crest remnants and dysraphisms can present as a neck mass. Rests of neural crest cells may be the origin of a cervical neuroblastoma or ganglioneuroma (Fig. 163.5). The dysraphic abnormalities are beyond the detailed scope of this resource.
IMAGING APPROACH
Techniques and Relevant Aspects and Pros and Cons
These factors are discussed in detail in Chapters 149 and 163.
There is a tendency to begin with ultrasound in the pediatric age group. While this sometimes is the most wise approach, an ultrasound study is far more often than not inconclusive and cost additive (Fig. 164.2).
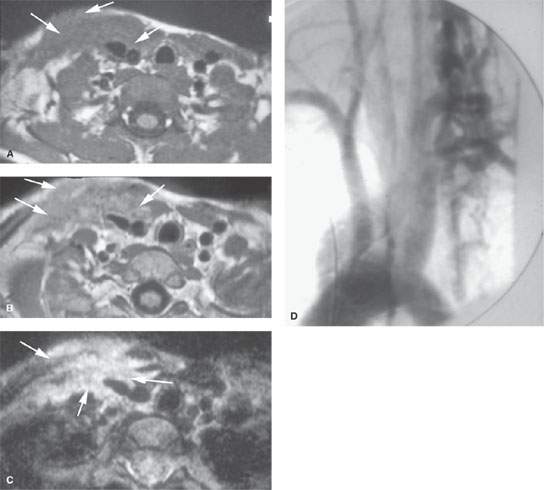
FIGURE 164.1. Two patients with cervicothoracic junction vascular malformations. A–C: Pediatric Patient 1 presenting with pain and tenderness and a compressible right supraclavicular fossa and low neck mass. In (A), the non–contrast-enhanced T1-weighted (T1W) image shows abnormal tissue (arrows) in the subcutaneous fat along the sternocleidomastoid muscle and enveloping the carotid sheath. In (B), the contrast-enhanced T1W image shows most of this tissue to enhance diffusely (arrows). In (C), the T2-weighted image shows abnormal tissue (arrows) to be very bright, suggesting a dominant fluid nature (NOTE: These findings were due to a partially inflamed and thrombosed venolymphatic malformation.) D: Patient 2 presenting with a pulsatile neck mass shown to be a high-flow vascular malformation on this arteriogram.
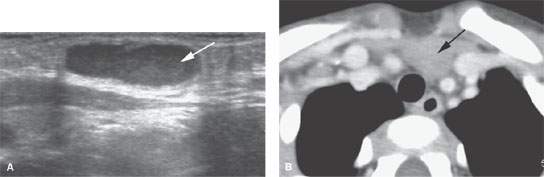
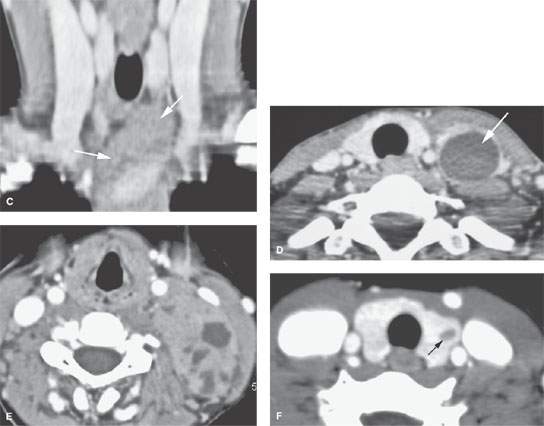
FIGURE 164.2. Several patients presenting with thymic-related abnormalities in the low neck and thoracic inlet region. A: Patient 1. Ultrasound showing a cystic lesion just off the midline (arrow) and overlying and slightly compressing the carotid artery. This was proven to be a thymic cyst. B, C: Patient 2, a child presenting with a midline and low neck mass. The contrast-enhanced computed tomography (CT) study shows normal thymic tissue projecting into the low neck, as seen on the axial image in (B) and the reformatted image in (C) showing the continuity between the mediastinal thymic tissue and that in the low neck (arrows). D: Patient 3 presenting with a low neck and thoracic inlet–region mass on the left. This was shown to be due to a thymic cyst (arrow). E, F: Patient 4 presenting with a left lower neck mass extending well superior to the cervicothoracic junction in the posterior triangle. The contrast-enhanced CT study shows this to be due to a thymoma arising in the ectopic thymic tissue. In (F), there is also aberrant thymic tissue cyst that was surgically proven in the left lobe of the thyroid gland (arrow).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








