GROSS ANATOMY
Overview
- •
Begins at inferior narrowing of uterus (isthmus)
- ○
Supravaginal portion: Endocervix
- ○
Vaginal portion: Ectocervix
- ○
- •
Endocervical canal: Spindle-shaped cavity communicates with uterine body and vagina
- •
Internal os: Opening into uterine cavity
- •
External os: Opening into vagina
- •
Largely fibrous stroma with high proportion of elastic fibers interwoven with smooth muscle
- •
Endocervical canal lined by mucus-secreting columnar epithelium
- ○
Epithelium in series of small, V-shaped folds (plicae palmatae)
- ○
- •
Ectocervix lined by stratified squamous epithelium
- •
Squamocolumnar junction near external os but exact position variable
- •
Nabothian cysts commonly seen
- ○
Represent obstructed mucus-secreting glands
- ○
- •
Entire cervix is extraperitoneal
- ○
Anterior: Peritoneum reflects over dome of bladder above level of internal os
- ○
Posterior: Peritoneum extends along posterior vaginal fornix, creating rectouterine pouch of Douglas (cul-de-sac)
- ○
- •
Arteries, veins, nerves, and lymphatics
- ○
Arterial supply
- –
Descending branch of uterine artery from internal iliac artery
- –
- ○
Venous drainage
- –
To uterine vein and drains into internal iliac vein
- –
- ○
Lymphatics
- –
Drain into internal and external iliac lymph nodes
- –
- ○
Innervation
- –
Sympathetic and parasympathetic nerves from branches of inferior hypogastric plexuses
- –
- ○
- •
Variations with pregnancy
- ○
Nulliparous: Circular external os, arterial waveform shows high resistivity index (RI)
- ○
During pregnancy: Changes become apparent by ~ 6 weeks of gestation
- –
Softened and enlarged cervix due to engorgement with blood with decreased RI of uterine artery
- –
Hypertrophy of mucosa of cervical canal: Increased echogenicity of mucosal layer
- –
Increased secretion of mucous glands: Increased volume of mucus ± mucus plug in cervical canal
- –
- ○
Parous: Larger vaginal part of cervix, external os opens out transversely with anterior and posterior lips
- ○
- •
Variations with age: Cervix grows less with age than uterus
- ○
Neonatal: Adult configuration due to residual maternal hormonal stimulation
- ○
Infantile: Cervix predominant with cervix:corpus length ratio ~ 2:1
- ○
Prepubertal: Cervix:corpus length ratio ~ 1:1
- ○
Reproductive: Uterus predominant, cervix:corpus length ratio ≥ 1:2
- ○
Postmenopausal: Overall reduction in size
- ○
Anatomy Relationships
- •
Anterior
- ○
Supravaginal cervix: Superior aspect of posterior bladder wall
- ○
Vaginal cervix: Anterior fornix of vagina
- ○
- •
Posterior
- ○
Supravaginal cervix: Rectouterine pouch of Douglas
- ○
Vaginal cervix: Posterior fornix of vagina
- ○
- •
Lateral
- ○
Supravaginal cervix: Bilateral ureters
- ○
Vaginal cervix: Lateral fornices of vagina
- ○
- •
Ligamentous support: Condensations of pelvic fascia attached to cervix and vaginal vault
- ○
Transverse cervical (cardinal) ligaments
- –
Fibromuscular condensations of pelvic fascia
- –
Pass to cervix and upper vagina from lateral walls of pelvis
- –
- ○
Pubocervical ligaments
- –
2 firm bands of connective tissue
- –
Extend from posterior surface of pubis, position on either side of neck of bladder and then attach to anterior aspect of cervix
- –
- ○
Sacrocervical ligaments
- –
Fibromuscular condensations
- –
Attach posterior aspect of cervix and upper vagina from lower end of sacrum
- –
Form 2 ridges, 1 on either side of rectouterine pouch of Douglas
- –
- ○
IMAGING ANATOMY
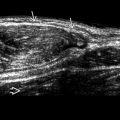
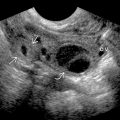
Ultrasound
- •
Transabdominal scan
- ○
Mucus within endocervical canal usually creates echogenic interface
- ○
In periovulatory phase, cervical mucus becomes hypoechoic due to high fluid content
- ○
Mucosal layer: Echogenic
- –
Thickness and echogenicity show cyclical changes similar to endometrium
- –
- ○
Submucosal layer: Hypoechoic
- ○
Cervical stroma: Intermediate to echogenic
- ○
- •
Transvaginal scan
- ○
Angle of insonation should be optimized for best visualization
- ○
Imaging may be improved with withdrawal of probe into midvagina
- ○
- •
Transperineal scan
- ○
Useful for evaluation of cervical shortening and incompetence after premature rupture of membranes or preterm labor
- ○
Useful when transvaginal scan cannot be tolerated
- ○
MR
- •
Important in local staging of cervical cancer
- •
Uniform intermediate signal on T1WI
- •
Zonal anatomy on T2WI
- ○
Endocervical canal: High signal
- ○
Cervical stroma: Predominately low signal, contiguous with junctional zone
- ○
Outer layer of smooth muscle (variably present): Intermediate signal
- ○
Parametrium: Variable signal intensity
- –
Cardinal ligament and associated venous plexuses high signal
- –
Sacrocervical ligament low signal
- –
- ○
GRAPHICS OF CERVIX ANATOMY