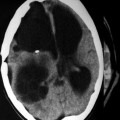
Fig. 16.1
CT scan of a 10-year-old male patient showing a hydatid cyst in the frontoparietal region (Courtesy of F. Limaiem, MD)

Fig. 16.2
CT scan of a 12-year-old male patient showing hydatid cyst in the right temporoparietal region (Courtesy of F. Limaiem, MD)
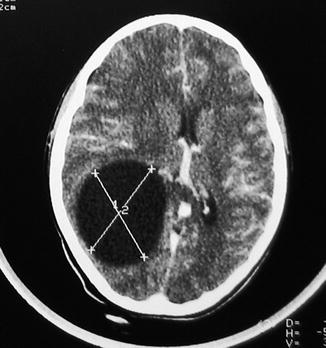
Fig. 16.3
CT scan of a 15-year-old female patient showing hydatid cyst in the right occipital region (Courtesy of F. Limaiem, MD)
The historical management of patients with CNS hydatidosis has been surgery, as it was the only modality of treatment available. Current treatment options include surgery, percutaneous evacuation, chemotherapy with benzimidazoles, and the watch and wait approach. The decision on which the treatment strategy is approached must be individualized for each patient, and combination therapy is often employed. Indications for treatment are complex and based on the characteristics of the cyst and other factors such as available medical/surgical expertise, equipment, and the ability of the patient to adhere to long-term monitoring (Brunetti et al. 2010). Spinal hydatid disease and alveolar CNS echinococcosis are treated primarily surgically and often with adjuvant chemotherapy.
Cystic Central Nervous System Hydatidosis
Cystic CNS hydatidosis is managed with surgery as the initial mode of therapy. Either surgery is combined with chemotherapy or, in some instances, chemotherapy is used singularly. Surgical therapy results in the complete resolution of lesions in the majority of cases. The response to albendazole (ABZ) is reported to be 64–100 % (Todorov et al. 1992a, b; Kalaitzoglou et al. 1998), and there have been a few case reports that have reported complete resolution of lesions following ABZ therapy. Both surgery and chemotherapy, alone or in combination, may result in complete eradication of cystic CNS hydatidosis.
Alveolar Central Nervous System Hydatidosis
Alveolar CNS hydatidosis is managed primarily with surgery where complete resection of the lesion is mandatory. This should be followed by chemotherapy for a limited period thereafter (2 years is recommended). Where surgery is not feasible, then chemotherapy, ABZ, or mebendazole (MBZ) as the only mode of therapy is acceptable, and this is usually administered long term or even lifelong. Since the introduction of chemotherapy after 1976, the 10-year survival has increased from less than 10 to 85–90 % in the chemotherapy era (Ammann and Eckert 1996).
Indications for Chemotherapy for Hydatidosis of the Central Nervous System
Surgery remains the first line of therapy for CNS hydatidosis and is the most effective form of therapy. Chemotherapy for CNS hydatidosis became a reality with the introduction of the two benzimidazoles, MBZ and ABZ, respectively, in 1976 and in 1982. Flubendazole (FBZ) was also shown to be effective for treatment of cystic echinococcosis (Ceballos et al. 2011) but is less efficacious than ABZ and is not used for the management of CNS hydatidosis. ABZ is most widely utilized, owing to its higher absorption in the gut and better gastrointestinal tolerability. Over the last 30 years, the use of chemotherapy in hydatidosis has evolved with a consensus now established on the indications, dosage, and follow-up of patients following initiation of therapy with benzimidazoles (World Health Organization [WHO] Informal Working Group on Echinococcosis 1996).
Traditional indications for chemotherapy for CNS hydatidosis include multiple or multiseptate cysts, large cysts (>10 cm), and cysts that are difficult to reach surgically or where the surgery would be clearly hazardous (El-On 2003; Ntusi and Horsfall 2008) (Table 16.1). Furthermore, patients with recurrence of CNS hydatid cysts are treated medically (Stojkovic et al. 2009), as are those for whom surgery would be contraindicated. There have been few case reports of the use of ABZ as the sole treatment of CNS hydatidosis with complete resolution of lesions on imaging (Kalaitzoglou et al. 1998; Ntusi and Horsfall 2008) in instances in which surgery was not feasible. However, there is no clinical trial evidence for the superiority of ABZ versus surgery for CNS hydatidosis.
Table 16.1
Indications for chemotherapy for central nervous system hydatidosis
1. Multiple/multiseptate cysts |
2. Large cysts (>10 cm) |
3. Cysts difficult to reach via surgery |
4. Recurrent CNS hydatid cysts |
5. Surgery is contraindicated |
6. Cases where surgery is clearly hazardous |
The adjunctive use of benzimidazoles before or after invasive procedures is now commonly practiced. The rationale for this indication is that perioperative administration may be important for cyst volume reduction and in minimizing the risk of rupture during the procedure (Morris 1987; Horton 1989).
In alveolar CNS hydatidosis, adjunctive chemotherapy with ABZ or MBZ following surgery is always indicated. In this instance, chemotherapy must be administered for a minimum of 2 years, and patients should be monitored for 10 years thereafter (Hemphill and Müller 2009). In instances where surgery is not feasible for alveolar hydatidosis, it is recommended that chemotherapy be used long term or lifelong. Currently, no evidence or guidelines are available for the perioperative use of benzimidazoles for alveolar CNS echinococcosis.
Indications for Surgical Treatment of Hydatidosis of the Central Nervous System
Surgery remains the cornerstone of management for uncomplicated cysts in CNS hydatidosis. The aim of surgical therapy is radical removal of the cyst without spillage of its content. Single lesions are more amenable to surgical removal compared to multiple lesions. All forms of spinal hydatid disease and alveolar CNS echinococcosis are treated surgically (Turgut 1997; Bresson-Hadni et al. 2000; Turgut 2001), as are lesions with bone involvement. Furthermore, patients who remain refractory to medical therapy or show progressive neurological decline despite chemotherapy should be considered for surgical treatment (Stojkovic et al. 2009).
Medical Chemotherapy for Hydatidosis
Benzimidazoles
Mechanism of Action
The action of benzimidazoles is their inhibitory effect on the uptake of glucose by the parasite, thus leading to the depletion of glycogen stores (Sheth 1975). The drug inhibits glucose uptake by the cestode, but does not affect serum glucose concentration in humans (Fierlafijn 1971). The benzimidazoles also result in degenerative alterations in the germinal layer of the cyst, leading to cellular autolysis (Schantz et al. 1982). In vitro studies have demonstrated disruption of microtubule structure and function in metacestodes treated with ABZ (Lacey 1988). Furthermore, benzimidazoles have been shown to have a higher affinity for parasite tubulin compared to that of the human host (Friedman and Platzer 1980; Gottschall et al. 1990), explaining their selective capacity for parasite immobilization and death.
Evidence of Efficacy
Benzimidazoles form the mainstay of medical chemotherapy for CNS hydatidosis. The efficacy of MBZ has been reported variably, with no consensus regarding the effective dose or optimal duration of therapy (El-On 2003). ABZ is more effective in the treatment of hydatidosis, most likely related to its superior intestinal absorption and particularly the higher penetration of its metabolite, ABZ sulfoxide, into the cyst cavity (Davis et al. 1989; Casado et al. 1996). ABZ is most efficacious in young cysts and in cysts less than 8 cm in size (Todorov et al. 1992a, b; Teggi et al. 1993).
There are limited data from randomized clinical trials, demonstrating efficacy of the benzimidazoles in the management of hydatidosis. FBZ has been shown to be inferior to ABZ and MBZ (Davis et al. 1986). Several trials have demonstrated the superiority of ABZ to MBZ, with a response rate of 75–85 % versus 50–60 %, respectively (Saimot et al. 1983; Todorov et al. 1992a, b; Teggi et al. 1993; Liu and Weller 1996; Luchi et al. 1997). The results of chemotherapy are affected by cyst characteristics such as size, age, and location, as well as by host characteristics (El-On 2003). ABZ is associated with evidence of radiological improvement in hydatid cysts in 68–82 % of patients (Falagas and Bliziotis 2007; Stojkovic et al. 2009). Prolonged courses of ABZ have been shown to be effective in the management of CNS hydatidosis (Teggi et al. 1993; Ntusi and Horsfall 2008).
Administration and Dosing
MBZ is given orally. About 2–10 % of the drug is absorbed intestinally and converted to its active metabolites, ABZ sulfoxide and ABZ sulfone, by the liver (El-On 2003). MBZ is excreted in the bile as glucuronide or a sulfate conjugate (Gottschall 1993). The usual dose in adults is 40–50 mg/kg/day, given in three equally divided doses after meals. Treatment is usually given for 3–6 months (Table 16.2).
Table 16.2
Administration and dosing of chemotherapy for central nervous system hydatidosis
Chemotherapy | Mechanism of action | Dose | Duration | Side effects |
|---|---|---|---|---|
Mebendazole | Inhibition of glucose uptake by parasite | 40–50 mg/kg/day inthree divided doses | 3–6 months | Nausea, vomiting,diarrhea, and abdominal pain |
Disruption of microtubules byinhibition of the polymerizationof tubulin into microtubules | ||||
Albendazole | Inhibition of glucose uptake by parasite | 10–15 mg/kg/dayin two divided doses | 3–6 months | Gastrointestinaldisturbances,abnormalities in liverfunction, leukopenia,and hematuria |
Disruption of microtubules byinhibition of the polymerizationof tubulin into microtubules | ||||
Praziquantel | Increases the cell permeabilityto calcium in cestodes | 25 mg/kg/day(in combinationwith albendazole) | No clear data | Dizziness, headache,malaise, abdominalpain, and nausea |
ABZ is also given orally. Its absorption in the gastrointestinal tract is better than for MBZ. It is metabolized by the liver to ABZ sulfoxide. The standard dose is 10–15 mg/kg/day, usually 800 mg/day, given in two equally divided doses. Absorption is improved by a fatty meal. Therapy is given for 3–6 months. Previously, ABZ was given for 4 week courses, followed by two drug-free intervals, due to safety concerns. Nevertheless, continuous therapy does not increase side effects (Teggi et al. 1993).