Chest Patterns
CS2. Chest Wall and Pleural-Based Lesions
CS3. Diaphragmatic Abnormalities
CS4. Diffuse Alveolar (Air-Space) Disease
CS5. Localized Alveolar (Air-Space) Disease
CS6. Diffuse Interstitial Disease
CS8. Focal Radiolucent Lesions
CS9. Intrathoracic Calcifications
CS9a. Cardiovascular Calcifications
CS9b. Hilar and Mediastinal Calcifications
CS13. Solitary Pulmonary Nodule and Mass
CS14. Multiple Nodules and Masses
CS1 Atelectasis
Atelectasis is defined as incomplete air filling and underexpansion of the lung. It may involve the entire lung or appear localized to a lobe, segment, or subsegment. The collapsed lung may displace the diaphragm, fissures, hila, mediastinum, or other anatomic borders. Regions of increased radiopacity and approximation of vascular markings, ribs, or other structures may occasionally be seen. Atelectasis is always secondary to underlying pathology; therefore, its presence should prompt a vigorous search for a cause. Although several mechanisms of collapse have been identified, obstruction of the airway is the most common.
| Disease | Comments |
| Adhesive (Adhesion of the Alveolar Interior Walls) | |
| Hyaline membrane disease | Decreased surfactant production in a neonate |
| Postoperative | Tissue adhesions related to cardiac or thoracic surgery |
| Cicatrizing (Scarring, Fibrosus, and Contraction of Lung Interstitium) | |
| Connective tissue disease | Widely disseminated radiopacities resulting from tissue fibrosus related to rheumatoid arthritis, scleroderma, idiopathic pulmonary fibrosis, and so on |
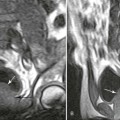
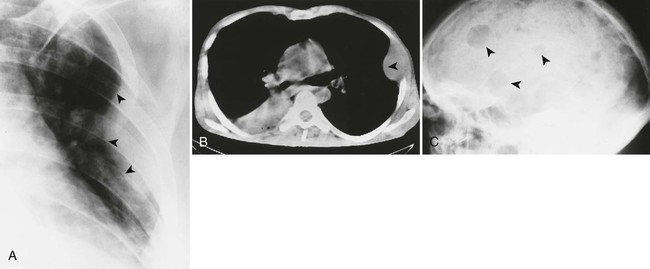
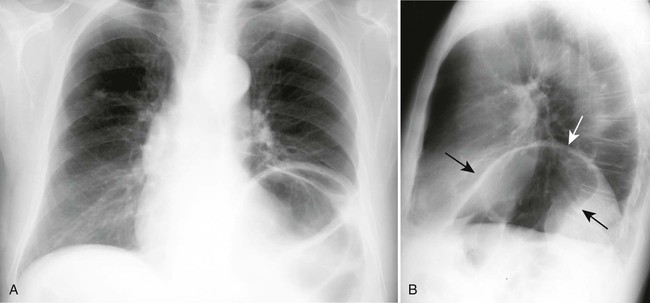
| Infections (Fig. 27-1) (p. 789) | Scattered linear and circular radiopacities in the upper lung fields correlating to a history of granulomatous infections (e.g., tuberculosis, histoplasmosis, coccidioidomycosis); lesions have a tendency to form irregular thick-walled cavities |
| Radiation | Nonanatomic regions of involvement correlating to history and site of past therapeutic radiation exposure |
| Compressive (Intrapulmonary Lesions Compressing Normal Lung Tissue) | |
| Bullous emphysema (p. 1173) | Large, thin-walled air sacs associated with emphysema and typically found in the upper lung; these sacs may compress adjacent normal lung tissue |
| Pulmonary mass | Space-occupying mass lesion within the lung (e.g., neoplasms, sarcoidosis) |
| Obstructive (Intrinsic or Extrinsic Airway Obstruction) | |
| Broncholithiasis | Occurs occasionally when a radiodense, calcified lymph node from prior granulomatous infection erodes through the bronchial wall and obstructs the lumen of the airway |
| Foreign bodies | Seen in infants, children (e.g., marble, peanut), and adults (e.g., dentures, tooth fragments after trauma, nails or screws held in mouth, meat) after aspiration of a foreign body; usually a characteristic history exists; occasionally, patients exhibit an asymptomatic period of hours to days after incident |
| Mucus plugs | Most often associated with asthma, chronic bronchitis, surgery, and neurologic suppression of cough reflex |
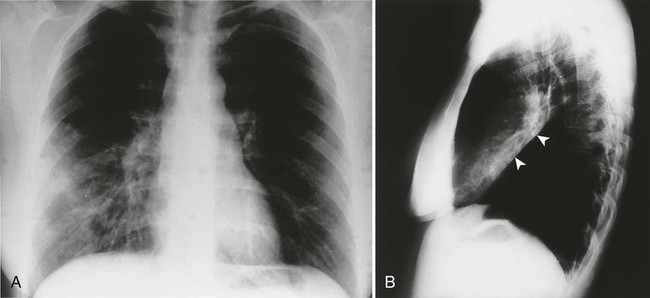
| Tumors (Fig. 27-2) (p. 1209) | Bronchogenic carcinoma is a common cause of obstruction in patients older than the age of 50 years; these patients may exhibit concurrent enlargement of the involved hilum or mediastinum. Bronchial carcinoid tumors are more common in younger patients. |
| Passive (Extrapulmonary Lesions Compressing Normal Lung Tissue) | |
| Body wall lesions | Expansile rib lesions, pleural-based disease, and intercostal soft-tissue lesions |
| Pleural space filling | Space-occupying lesions in the pleural space (e.g., edema, chyle, hemorrhage, air) |
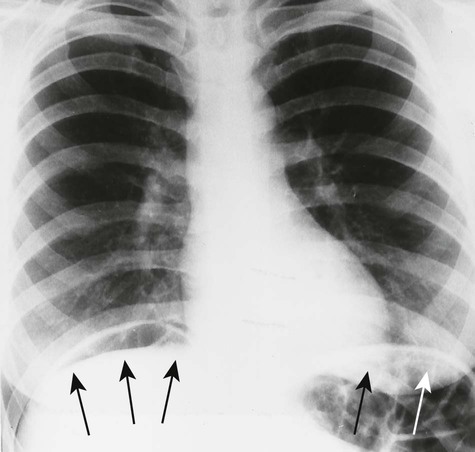
| Subsegmental, Plate-like, Discoid (Linear Radiopacity in Periphery of Lung) (Fig. 27-3) | |
| Hospitalization | Resulting from hypoventilation caused by painful breathing, anesthesia, pleural effusion, pneumonia, and so on |
| Pulmonary embolism (p. 1190) | Commonly involves collapse as a nonspecific finding of acute pulmonary embolism, often associated with pleural effusion; when the collapse occurs in late manifestations of the disease, it represents pulmonary scar formations |

CS2 Chest Wall and Pleural-Based Lesions
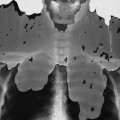
Chest wall and pleural-based lesions often are marked by a characteristic radiographic appearance of a radiopaque convexity extending inward toward the lung with sloping superior and inferior tails. The outer border of the lesion is incompletely defined, confirming an extrapulmonary location. A variety of etiologies are responsible, including infections, primary neoplasms, metastasis, and trauma.
| Disease | Comments |
| Abscess (p. 1395) | Most commonly results from Staphylococcus infection, tuberculosis, and actinomycosis; associated characteristics include rib involvement, pulmonary infiltrate, pleural effusion, and a painful red subcutaneous mass |
| Hematoma | Suggested by the presence of pleural effusion, history of trauma, evidence of trauma (e.g., rib fracture), or hemoptysis; retrosternal hematomas occasionally are seen in the lateral projection on patients experiencing automobile accidents, in which the steering wheel inflicts blunt trauma to the chest |
| Pleural fluid (p. 1185) | Free or loculated transudate, exudate, blood, chyle, and so on presenting as a well-defined density in the pleural space |
| Rib fracture | Secondary to blunt or penetrating trauma to normal ribs or less forceful trauma to ribs affected by pathology (e.g., tumor or infection). Fracture occurs as a thin, vertical radiolucent line with offset of rib cortices, best seen on an oblique projection; acute fracture warrants a careful search for associated hemothorax or pneumothorax. |
| Rib tumors (Fig. 27-4) | Most common benign tumors: osteochondromas followed by enchondromas and osteoblastomas; metastatic bone disease, chondrosarcoma, and multiple myeloma produce multiple lytic regions; nonneoplastic lesions such as fibrous dysplasia commonly involve the ribs |
| Skin lesions | Soft-tissue densities (e.g., nipples, moles, neurofibromas) typically appear with incomplete borders because of region of contact with the skin. Examination of the skin surface or repeat radiographs using a radiopaque marker confirms questionable lesions. |
| Soft-tissue benign tumor | Variety of tissue types, appearing as a smooth, protruding mass from body wall into lung field; lipomas are most common and may present as intrathoracic or extrathoracic lesions |
| Soft-tissue malignant tumor | Often visible, painful mass with associated bone destruction; the most common malignant soft-tissue neoplasms of the chest wall in adults are fibrosarcoma and liposarcoma; metastasis, mesotheliomas, and bronchogenic (Pancoast) tumors may involve the pleura; a past history of radiation therapy is a risk factor |
CS3 Diaphragmatic Abnormalities
The right hemidiaphragm typically is one intercostal space higher than the left. With proper inspiratory effort, the right hemidiaphragm should be below the level of the posterior portion of the tenth rib or the anterior portion of the seventh rib. The position of the left hemidiaphragm varies more than that of the right because of the subjacent gastric air bubble. Unilateral or bilateral changes of the diaphragm’s position suggest underlying pathology of the thorax or abdomen.
CS3a Depressed Diaphragm
| Disease | Comments |
| Increased pulmonary volume (Fig. 27-5) | Unilateral lung overinflation resulting from a large bulla, a pulmonary cyst, or in response to a contralateral small lung; chronic bilateral overinflation results from diffuse obstructive emphysema or is transient with asthma and expiratory air trapping because of bronchial obstruction |
| Large pleural effusion (p. 1185) | Difficult to detect because the fluid obliterates the diaphragm contour; the position of the gastric air bubble indicates the position of the left hemidiaphragm |
| Pneumothorax (p. 1238) | Other radiographic findings of pneumothorax: absence of interstitial and bronchovascular lung markings and the characteristic thin radiodense line represents visceral pleura; if large, the pneumothorax may invert the dome of the diaphragm |

CS3b Elevated Diaphragm
| Disease | Comments |
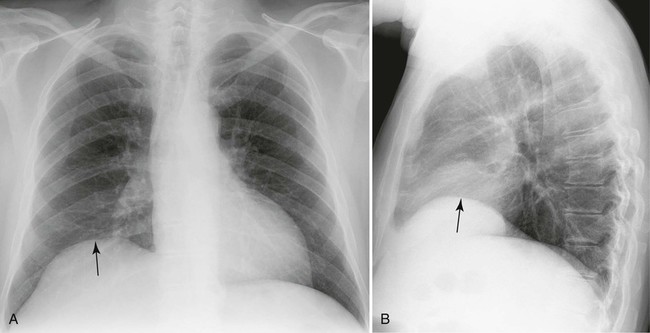
| Congenital eventration (Fig. 27-6) | Represents an elevated segment of the diaphragm, resulting from congenital absence or weakness of a portion of the diaphragmatic musculature; this condition results in poor contractility and inability to resist infradiaphragmatic visceral pressure; total hemidiaphragm eventration is more common on the left; partial hemidiaphragm eventration is more common on the right and usually involves the anteromedial segment |
| Diaphragm splinting | Lack of diaphragm excursion in response to pain, fracture, infection, and so on |
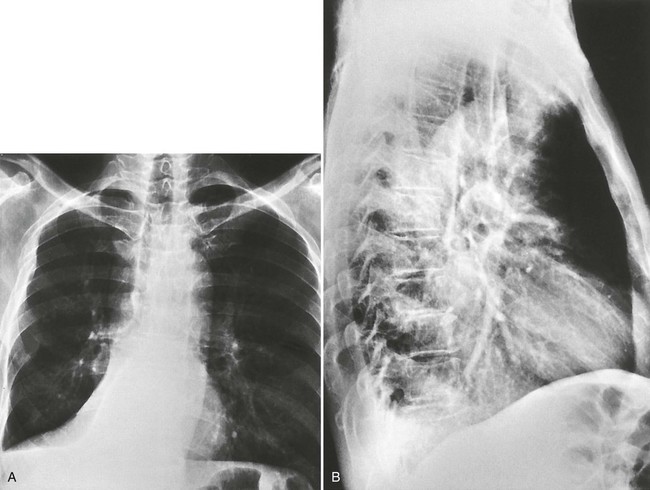
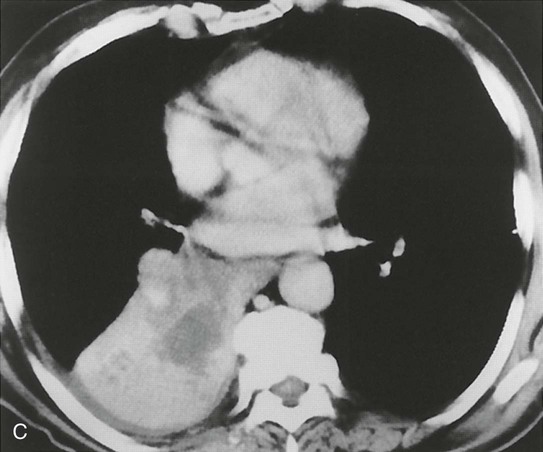
| Diaphragmatic hernia (Fig. 27-7) | Most commonly the esophageal hiatal hernia presents as a centrally located air-fluid level behind the heart shadow in the frontal projection; an esophagram is confirmatory; Bochdalek hernias typically appear as posterolateral masses above the left hemidiaphragm and represent herniations of retroperitoneal contents; Morgagni hernias typically appear as anteromedial right-sided masses in the cardiophrenic angles. |
| Intraabdominal mass (Fig. 27-8) | Unilateral elevation resulting from renal, hepatic, or splenic abscess, tumor, cyst, or gas distension of the bowel, stomach, or peritoneal cavity; bilateral elevation results from pregnancy, obesity, and ascites |
| Phrenic nerve paralysis | Reduces the contractility of hemidiaphragm by damage to the phrenic nerve (surgical transection, pressure from hilar mass, poliomyelitis, and Erb palsy); the affected diaphragm exhibits paradoxic motion under fluoroscopic observation by ascending rather than descending movement during inspiration (positive sniff test result) |
| Poor inspiratory result | Inspiratory effort is defined as the patient’s compliance with inspiratory instructions during the radiographic exposure. Inspiratory result is a general term encompassing both inspiratory effort and mechanical obstacles to full inspiration, such as obesity, pregnancy, and ascites. |
| Reduced pulmonary volume | Loss of lung volume resulting from congenital hypoplasia, pneumonectomy, atelectasis, and other diseases |
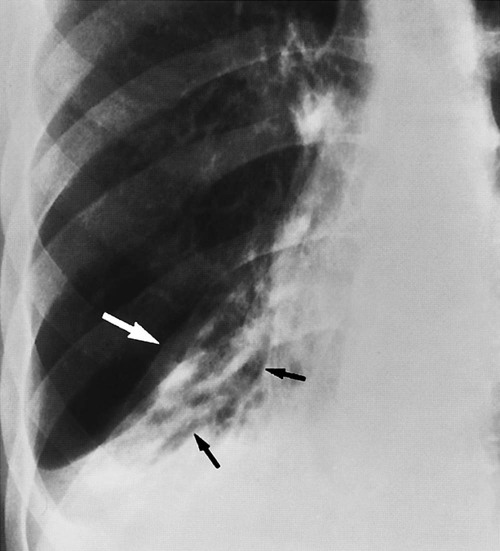
| Ruptured diaphragm (Fig. 27-9) | Significant blunt, crushing, or penetrating thoracoabdominal trauma possibly causing abdominal contents to herniate into the thoracic cavity; the rupture is nearly always left sided because the liver dissipates traumatic forces on the right; a ruptured diaphragm appears as a gas-filled bowel or stomach seen in the left lower lung field |
| Subpulmonary effusion (p. 1185) | Pleural fluid under the lung possibly simulating elevation of the diaphragm; commonly the pseudodiaphragm, or dome of the fluid, appears more lateral than its normal position; lateral decubitus projections may aid in differentiating subpulmonary effusion from an elevated diaphragm |
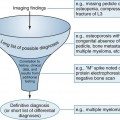
CS4 Diffuse Alveolar (Air-Space) Disease
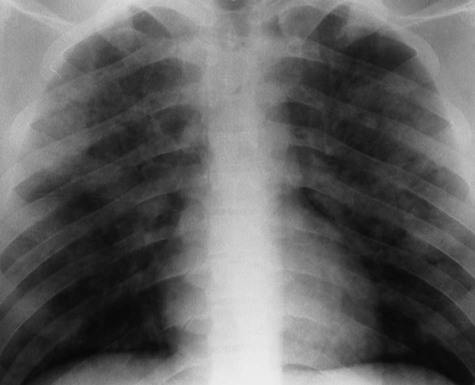
Diffuse alveolar disease comprises bilateral, widely disseminated opacifications that appear dense (homogenous consolidation) and are related to complete filling of the alveolar space. Alternatively, a patchy and fluffy appearance (heterogeneous consolidation) denotes incomplete filling of the alveolar space.
The opacifications of lung vary in size and exhibit a tendency toward coalescence. Within the regions of opacification, characteristic tubular radiolucent shadows are occasionally seen, representing air-filled bronchi transversing water-filled parenchyma (air-bronchogram sign).
The diseases are divided into acute and chronic forms based on history and serial radiography. Although an exact timeline is difficult to develop, patterns that remain largely unchanged for several weeks or months are chronic.
| Disease | Comments |
| Acute Diffuse Alveolar Disease | |
| Acute respiratory distress syndrome (p. 1235) | Increased capillary permeability resulting from a wide variety of systemic and pulmonary insults (e.g., drug abuse, fractures, smoke inhalation, shock), causing excessive fluid accumulation in the alveolar spaces |
| Near-drowning (Fig. 27-10) | May be prevented by laryngeal spasm; otherwise, fluid may enter the lung from drowning or submersion events |
| Pneumonia (p. 1193) | Related to aggressive infections of the lung; patients typically are extremely ill, exhibiting fever, productive cough, difficulty breathing, and malaise; although many organisms may be associated with this presentation, gram-negative infections are notorious for producing this appearance |
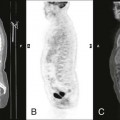
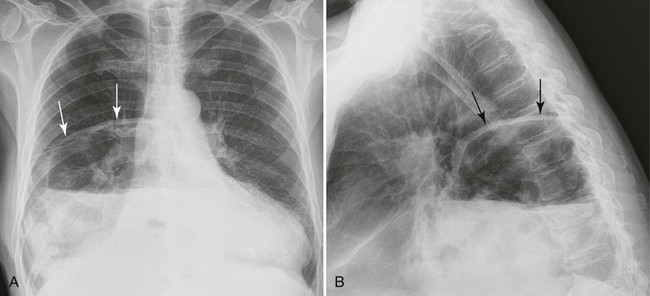
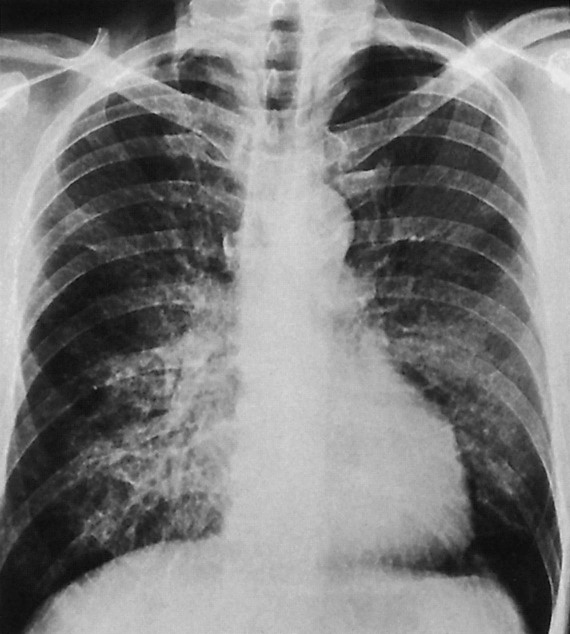
| Pulmonary edema (Fig. 27-11) (p. 1188) | Accumulates within the interstitium during the early stages; the resulting linear densities are termed Kerley lines and are subdivided by position within the lung; lymphatic drainage is overwhelmed as fluid accumulates, and edema spills over to the alveolar lumen, relating an alveolar pattern; the appearance may be “cloud-like,” diffusely involving the lung fields bilaterally; as pulmonary edema progresses, the alveolar pattern is seen centrally with interstitial extensions to the periphery |
| Pulmonary hemorrhage | Associated with anticoagulant therapy, pulmonary contusion, or less commonly Goodpasture syndrome; hemoptysis and patient history are indicative |
| Chronic Diffuse Alveolar Disease | |
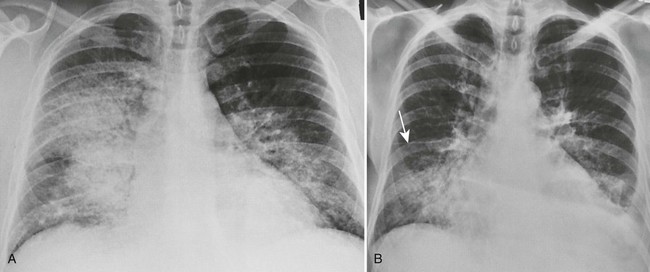
| Alveolar proteinosis (Fig. 27-12) | Bilateral confluent radiopacities, less commonly diffuse nodular pattern; appearance may be transient, and there are surprisingly few associated clinical symptoms apart from dyspnea |
| Radiation pneumonitis | Diffuse pulmonary damage with accompanying history of therapeutic radiation |
CS5 Localized Alveolar (Air-Space) Disease
Solitary or multiple localized alveolar disease is marked by extensive filling of the alveolar spaces with space-occupying lesions (e.g., blood, edema, pus, protein, cells), relating a complete (homogenous) or partial (heterogeneous) consolidation or opacification of a segment, lobe, or entire lung.
This pattern differs from the previous pattern of diffuse alveolar pattern because the involved pulmonary region is localized, unilateral, and peripherally well defined. However, similar to the previous pattern of lung disease, it may be separated into acute and chronic presentation based on patient history and available serial radiographs. Although an exact timeline is difficult to develop, patterns that remain largely unchanged for several weeks or months are chronic.
| Disease | Comments |
| Acute Localized Alveolar Disease | |
| Bronchioloalveolar (alveolar cell) carcinoma (Fig. 27-13) (p. 1209) | May appear as well-defined consolidation similar to pneumonia; however, it does not respond to appropriate management of pneumonia |
| Pulmonary contusion | Appearance corresponding to alveolar collections of edema and atelectasis of the lung in response to bronchial obstruction; the obstruction may develop slowly (e.g., bronchogenic carcinoma, bronchial carcinoid tumors) or rapidly (e.g., foreign body, mucus plug) |
| Obstructive pneumonitis | Consolidation of lung parenchyma (lung, lobe, or segment) resulting from filling of the normally air-filled alveolar sacs with exudate and inflammatory cells of similar radiopacity to water. Causative agents include bacteria, fungi, and viruses; clinical features of malaise, fever, and purulent expectorant typically accompany the radiographic findings; the consolidated area becomes patchy and fades to normal after successful treatment. |
| Pneumonia (Fig. 27-14) (p. 1193) | Transient densely radiopaque or incompletely consolidated patchy regions that extend from the body wall and represent blood and edema in the alveolar sacs; history of blunt trauma to the chest and presence of rib fractures are strongly indicative |
| Chronic Localized Alveolar Disease | |
| Atelectasis (p. 1166) | Incomplete inflation of a lung (or segment) possibly appearing as a region of increased radiopacity resulting from increased lung density; concurrent finding of incomplete inflation (hilar, diaphragm, or mediastinum displacement) and clinical absence of fever and purulent cough distinguish atelectasis from pneumonia |
| Lymphoma (p. 1226) | Appearance of radiopacities that represent pulmonary infiltrate of neoplasm or superimposed infection secondary to immunosuppression after treatment; often lymphoma presents with mediastinal widening; pulmonary involvement occurs as a result of direct lymphatic extension from the mediastinum |
| Pulmonary infarct (Fig. 27-15) (p. 1198) | Radiopaque parenchymal density (classically pleural-based triangular appearance with apex toward hilum) located most commonly in the peripheral lower lung field. Over time the lesions tend to resolve from the periphery, inward to the center, preserving the radiopacity’s triangular configuration (“melting” sign) |
| Radiation pneumonitis | Patchy, irregular areas of incomplete consolidation resulting from tissue “weeping” and edema produced from tissue irradiation; a history of radiation is suggestive; the location corresponds to the radiation port |
| Sarcoidosis (p. 1240) | Patchy, irregular, radiopaque areas representing noncaseating, granulomatous deposits in the interstitium; it appears as an alveolar pattern; parenchymal involvement only is an uncommon presentation of the disease; more commonly, findings include concurrent enlarged hilar lymph nodes or adenopathy that precedes the pulmonary disease; sarcoidosis is more common in blacks and women |
| Tuberculosis (p. 1198) | Transmitted by repeated contacts with infected individuals through inhalation; tuberculosis is not easily contracted in immunocompetent individuals; consequently, the immunocompromised and those of low socioeconomic scale (e.g., acquired immunodeficiency syndrome [AIDS] patients, alcoholics, elderly people, homeless persons) are vulnerable. The radiographic features of the primary infection include consolidation with pleural effusion; any lung segment may be involved, and the findings typically resolve without complication; reactivation infections typically involve the upper lobes, often with scarring and a tendency toward cavitation. |

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree