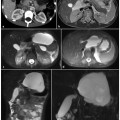
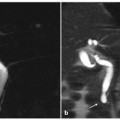
Fig. 4.1
Multiple bile duct stones causing cholangitis. a A magnetic resonance cholangiopancreatography image shows dilatation of the entire biliary tree, with multiple hypointense intraluminal defects caused by stones. T1-weighted magnetic resonance images, before (b) and after (c) contrast-medium injection, show some distorted areas near the biliary major ducts, hypointense in the basal condition and with poor contrast enhancement, consistent with inflamed biliary walls and adjacent liver parenchyma (b, c, arrows). An endoscopic retrograde cholangiopancreatography (ERCP) procedure (d) allows removal of bile duct stones from the lumen of the common biliary duct (e), but the multiple small intrahepatic biliary stones cannot be removed; therefore ERCP is repeated to remove the remaining small stones (f)
Biliary obstruction following endoluminal treatment of biliary ducts indicates a high risk of cholangitis [6]. The microorganisms most frequently cultured from patients affected by cholangitis are Escherichia coli, Enterococcus spp., Klebsiella spp. and enterobacteria [4, 7]. Regarding Pseudomonas spp., the skin and oral flora have been investigated following interventional procedures, and anaerobic bacteria found in 15% of cases, most frequently in elderly patients or following surgery on biliary ducts [1, 7, 8].
The most frequent cause of cholangitis in industrialized countries is choledoco-lithiasis (>80% of cases), secondary to cholelithiasis; other possible causes are sclerosing cholangitis, neoplasia (10–20% of cases), ERCP, advanced age (>70 years), neurological diseases, the presence of peri-ampullary diverticula, fibrosis of the papilla, pancreatitis, bile duct neoplasia, and metastasis of the hepatic hilum and peri-pancreatic lymph nodes.
Primary choledocholithiasis is rarely seen in western countries, while it is more common in Asian countries, namely Hong Kong and Southeast Asia, where oriental cholangiohepatitis is endemic [1, 9]. The tendency of oriental cholangiohepatitis to form multiple gallstones in multiple ducts and locations differs from that seen in western populations, where gallstones are more frequently found in the distal third of the main bile duct and tend to be made of cholesterol, originating from the gallbladder. The cause of oriental cholangiohepatitis is not known; however parasitic infections (Clonorchis sinensis, Ascaris lumbricoides), portal bacteremia and malnutrition have been implicated in its aetiology.
The clinical presentation of cholangitis may vary. The classic Charcot’s triad with fever, jaundice and pain in the right hypochondrium is observed in 50–70% of cases [1, 4, 10, 11]. Fever is usually seen in 90% of cases, while jaundice and pain in right hypochondrium are reported in 60% and 70% of cases, respectively [4]. A small percentage of patients present an altered state of consciousness (10–20%) and hypotension (about 30%): the so-called „Reynold’s pentad”, when associated with Charcot’s triad [1, 4, 10, 11]. Pain in the right hypochondrium is present in two-thirds of patients, but signs of peritoneal irritation are less frequently observed [12]. Severe cholangitis may be associated with hepatic microabscesses, which are typically associated with a more severe prognosis.
The diagnosis of acute cholangitis is a clinical one, but should be confirmed by laboratory data and diagnostic imaging. Moreover, acute cholangitis should be differentiated from cholecystitis, hepatic abscess and pancreatitis. Diagnostic laboratory tests typically indicate leukocytosis, hyperbilirubinemia, increased alkaline phosphatase and a modest elevation of transaminase.
Acute complications of acute cholangitis include sepsis, hepatic abscesses, portal vein thrombosis, bile peritonitis and death. The mortality rate ranges between 4% and 60% and seems to be related to increased pressure inside the biliary ducts, as this is one effect of the disease that favors the passage of bacteria and toxins into the systemic circulation, leading to septic shock.
Treatment involves the use of antibiotics and possibly the removal of the cause of biliary obstruction.
Histological examination shows: increased wall thickness of the biliary ducts, with an inflammatory infiltrate and the presence of small ulcers; enlargement, of periportal spaces resulting from edema and the presence of leukocytes; tortuosity of bile ducts (caused by an increased intraluminal pressure); and the presence of small periductal abscesses.
Ultrasonography and computed tomography (CT) are the first-line diagnostic imaging techniques in use.
Ultrasonography shows high sensitivity in diagnosing cholelithiasis [11], but lower sensitivity in diagnosing choledocholithiasis (about 50%) [13].
Choledocholithiasis may be suspected when there is association with biliary duct dilatation in the presence of cholelithiasis. An ultrasound (US)-negative test does not exclude the presence of cholangitis [1]. Many studies suggest that CT is superior to US in determining the degree of biliary duct obstruction [14–16]. Magnetic resonance imaging (MRI) and magnetic resonance cholangiopancreatography (MRCP) have >90% accuracy in diagnosing choledocholithiasis and in showing biliary anatomy.
ERCP is accurate in determining the cause of biliary obstruction and allows appropriate treatment, when necessary. However, given the risk of complications, and the accuracy of non-invasive diagnostic imaging techniques, ERCP should not be used as a diagnostic technique, but it should be used when the need for intervention is high, as in the case of many patients with clinical suspicion of cholangitis. In particular, ERCP is indicated when cholangitis is suspected in patients with cholelithiasis, and the possibility of a concurrent choledocholithiasis is high [2, 8, 9, 17].
During the acute phase of ascending cholangitis, the presence of biliary sludge can be identified in diagnostic imaging studies. Liver abscesses, which complicate bacterial cholangitis, are readily identified by US investigations as corpusculate fluid gatherings that are heterogeneously hypoechoic, with septa, debris or gas. CT can also identify the following: the presence of abscesses associated with dilatation of the bile ducts: welldefined, round, hypodense masses (0–45 HU); „target lesions” (with hypodense rim, isodense periphery and decreased attenuation in the center); the presence of central gas; and the presence of air-fluid level or fluid-debris level (Fig. 4.2).
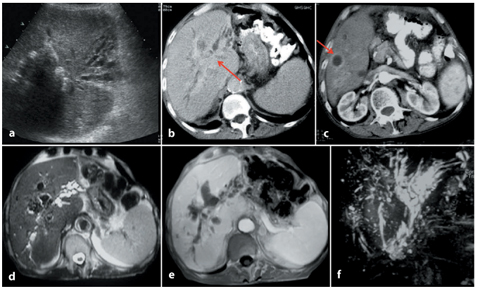
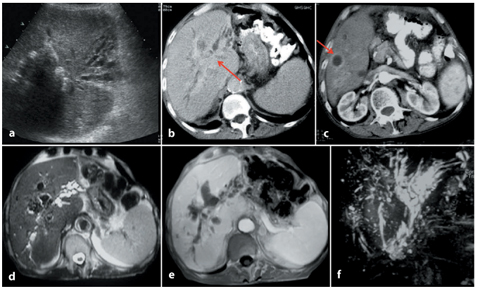
Fig. 4.2
Bacterial cholangitis. a Ultrasound image of the hepatic left lobe showing a dilated biliary tree and heterogeneously hypoechoic area at the hepatic hilus.b, c Computed tomography scan confirming the biliary tree dilatation, with inflammation of the major biliary duct at the hepatic hilus (b, arrow). A hypodense, well-shaped area with peripheral enhancement is present in segment VII, consistent with a liver abscess (c, arrow). T2-weighted magnetic resonance image (d) and T1-weighted post-contrast image (e) demonstrate a hypointense area near the hepatic hilus, with some intraluminal defects in the biliary tree (pneumobilia). Magnetic resonance cholangiopancreatography confirms the important biliary tree dilatation, especially of the intrahepatic bile ducts of the left lobe
At MRCP, a typical sign associated with choledocholithiasis is dilatation of intrahepatic biliary ducts, with the following distribution types: central portion of the liver (38%), diffuse (16%) and segmental (46%). The bile ducts show an increased wall thickness (mean 2.2 mm), with symmetrical distribution and diffuse hyperintensity in T2-weighted and post-gadolinium sequences, often associated with periportal liver parenchyma of the same appearance and focal areas of liver parenchyma affected by the inflammatory process [18]. It has been reported that this type of cholangitis can show persistent increased enhancement on 2 min post-gadolinium fat-suppressed images [18]. This is probably the result of greater capillary leakage of the contrast agent into the liver parenchyma interstitium.
Additional signs of choledocholithiasis are parenchymal atrophy, adipose involution, contrast enhancement of the biliary ducts and segmental contrast enhancement of the liver and parenchyma, hepatic abscess, biloma and pneumobilia.
4.2.2 Recurrent Bacterial Cholangitis
Recurrent bacterial cholangitis is caused by repeat episodes of bacterial cholangitis.
It usually appears after the age of 40 years, with a similar incidence in men and women, and it is more common in Southeast Asia populations.
Predisposing factors are the presence of ectasias and biliary duct stenosis, as well as intrahepatic lithiasis [19].
Clinically, it presents with pain in the right hypochondrion, recurrent fever and jaundice, which may be associated with hypotension and shivering in cases of septicemia caused by Gram-negative microorganisms. Laboratory tests show leukocytosis, and high levels of alkaline phosphatase and bilirubin.
Abscess formation is one possible acute complication (20% of cases) (Fig. 4.3).
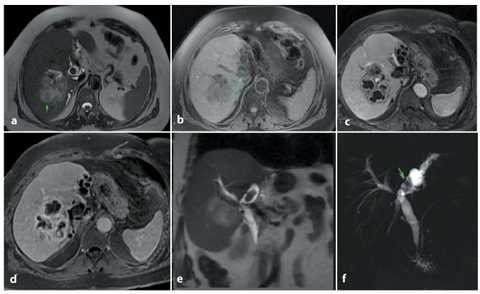
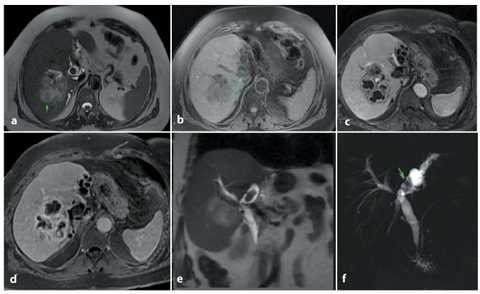
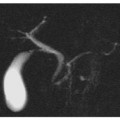
Fig. 4.3
Large stone within the common biliary duct, with hepatic abscess. T2-weighted (a) and T1-weighted (b) magnetic resonance images show a large stone (a, b, arrows) in the left bile duct that appears hypointense on the T2- weighted image and hyperintense on the T1-weighted image; it coexists with a distorted, heterogeneous hypointense area in the right hepatic lobe (a, arrow). c, d After contrast-medium injection, this area remains heterogenous, with a progressive peripheral enhancement and multiple central hypointense regions caused by colliquation. This is the typical aspect of a cholangitic abscess caused by bile stagnation. Coronal T2-weighted (e) and magnetic resonance cholangiopancreatography (f) images confirm biliary tree dilatation especially in the left lobe, and the large stone in the left major duct (f, arrow)
Among chronic complications, ductal obstruction and chronic portal thrombosis can lead to lobar or segmental atrophy (usually localized to the left lobe) (Fig. 4.3); the risk of cholangiocarcinoma is higher in these patients, with an incidence of 5–18%. [19] The last stage of the disease is represented by biliary cirrhosis (Fig. 4.4).
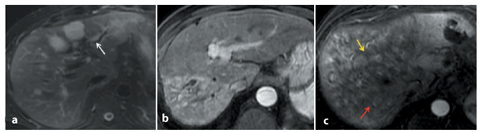
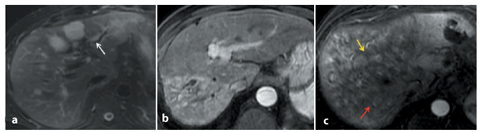
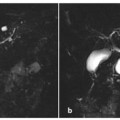
Fig. 4.4
Subacute and chronic hepatic changes in bacterial cholangitis. In three different patients, subacute cholangitis presents with areas of increased parenchymal signal intensity on a T2-weighted image (a) and contrast enhancement (b) in a patchy, peribiliary or wedge-shaped distribution. A white arrow indicates inflamed dilated intrahepatic bile ducts with pneumobilia (a). c In chronic cholangitis damage, microabscesses are present (yellow arrow), but the relevant feature of this stage is the subcompleted hepatic architecture subversion, with extended fibrotic involvement and parenchymal destruction (red arrow)
The picture of acute cholangitis is associated with ectasia of the biliary ducts and intrahepatic lithiasis (stones occur in up to 80% of cases) [20].
Stenotic biliary segments can be identified, interposed between dilated ductal segments, but they are usually less than 1 cm in size. The periportal space is thickened. Pneumobilia is a frequent finding: it can be caused by bacterial fermentation, but more often by the passage of stones through the ampulla [20, 21].
The disease, when localized, can be treated with drainage, stenosis dilatation and stone removal. When recurrent or diffuse, or when first-line intervention has failed, surgery must follow.
4.2.3 Diagnostic Imaging
T1-weighted MRI shows dilated ducts appearing hypointense, with gallstones that are hyperintense or of intermediate intensity.
On T2-weighted images, the dilated ducts appear hyperintense, with hypointense filling defects caused by biliary stones.
After administration of contrast agents, there may be contrast enhancement of the ductal walls and the adjacent liver parenchyma due to fibrosis and inflammation present during exacerbation phases; this is better appreciated during the portal vein equilibrium phase.
The MRCP pattern shows dilated intrahepatic and extrahepatic ducts, often with low signal filling defects (stones); it also shows stenosis and narrowing of peripheral ducts, with the disappearance of more peripheral branches and the sudden thinning of biliary ducts with an „arrowhead” appearance. Poor representation of the more peripheral bile ducts is associated with a disproportionate dilatation of intrahepatic and extrahepatic proximal biliary ducts [21] (Fig. 4.5).
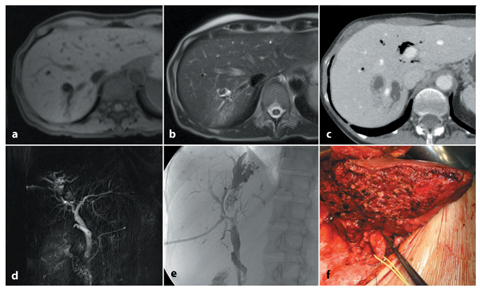
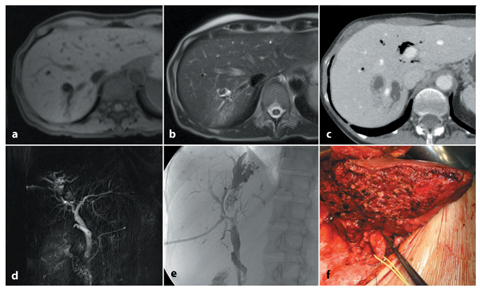
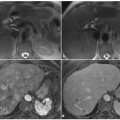
Fig. 4.5
Recurrent pyogenic cholangitis. a, b The intrahepatic biliary tree is dilated. The intrahepatic duct stone is hypointense in the T2-weighted image (b), and hypointense with a central hyperintense spot in the T1-weighted image (a). b The T2-weighted image shows an area of increased parenchymal signal intensity in a wedge-shaped distribution. c A computed tomography scan shows inflamed dilated intrahepatic bile ducts with pneumobilia. Magnetic resonance cholangiopancreatography (d) and endoscopic retrograde cholangiopancreatography (e) confirm the dilatation of the intrahepatic biliary tree, with a segmental distribution and multiple small filling defects within the dilated bile ducts representing intrahepatic duct stones. f The surgical specimen confirms the radiological diagnosis
ccount acute bacterial cholangitis, sclerosing cholangitis and cholangiocarcinoma. Sclerosing cholangitis is characterized by thickening of the common bile duct, multiple stenoses, stones forming distally to stenoses and association with chronic inflammatory bowel disease. Cholangiocarcinoma is associated with sclerosing cholangitis, choledochal cysts, recurrent pyogenic cholangitis and clonorchiasis. The infiltrative type of cholangiocarcinoma, which is involved in the differential diagnosis of benign stenoses, is more often found at the confluence of hepatic ducts. It is characterized by duct dilatation, with or without parenchymal mass. The late retention of contrast medium is typical.
4.2.4 Parasitic Cholangitis
Parasitic cholangitis is characterized by a varied clinical presentation and, when complicated by bacterial superinfection, may be indistinguishable from recurrent bacterial cholangitis. Imaging, serological tests and the presence of eosinophilia may help in the diagnosis.
4.2.4.1 Echinococcosis
Humans can be accidentally infected by Echinococcus granulosus, for which they act as intermediate hosts. Initially, infection leads to the formation of a simple cyst surrounded by a fibrous capsule produced by the host, and this is known as the pericyst. In this stage of the disease, MRI shows a simple cyst with a hypointense border, corresponding to the fibrous capsule. Subsequently, daughter cysts start to develop inside the cyst, and produce its characteristic „cartwheel” appearance: daughter cysts appear less hypointense than the mother cysts on T1-weighted images. With the death of the parasite, the endocysts break away (water-lily sign) and the cyst calcifies [20, 22].
Untreated cysts expand, causing damage from mass effect: pressure can exceed that of the biliary tree, causing rupture and fistulization in the biliary ducts, leading to cholangitis. Biliary echinococcosis is characterized by dilatation of the biliary ducts, cystobiliary fistulas, and filling defects in biliary ducts caused by daughter cysts and hydatid membranes.
Peritonitis is more rare, caused by the cyst rupturing into the peritoneal cavity (Fig. 4.6).
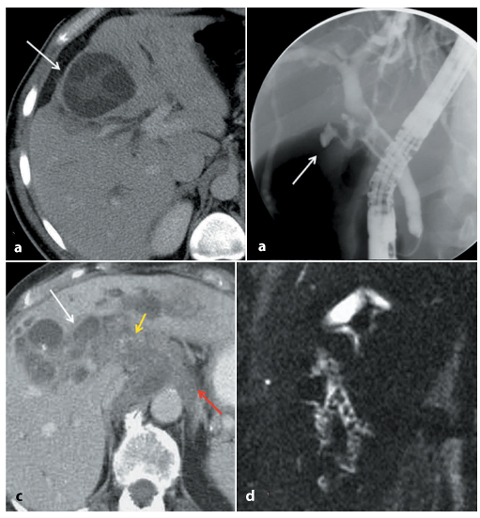
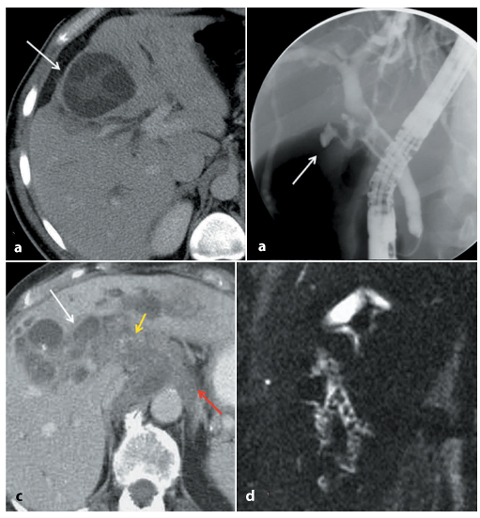
Fig. 4.6
a, b Hydatid disease (Echinococcus granulosus). Computed tomography shows the typical spoke-wheel appearance (a, arrow) of E. granulosus, with multiple daughter cysts arising from the germinal layer. Surrounding biliary ducts are dilated due to intraductal echinoccosis, which is more clearly depicted at endoscopic retrograde cholangiopancreatography (b, arrow). c, d Alveolar hydatid disease (Echinococcus multilocularis). Multiple hypodense lesions within the hepatic parenchyma represent necrotic tissue, and some cysts (c, white arrow), representing vital metaceste vesicles, are demonstrated on computed tomography (c). Note associated calcifications (c, yellow arrow). Parasitic tissue (c, red arrow) infiltrates the retroperitoneum and the hepatic hilum, partially encasing the aorta. d The magnetic resonance cholangiopancreatography image demonstrates the biliary tree dilatation, with multiple intraductal defects due to intraductal echinoccosis
4.2.4.2 Clonorchiasis
This is an infection found predominantly in the Far East Asia. The parasite, in the form of metacercaria, enters the biliary tree, nestles in the medium- and small-caliber ducts and stays there, proliferating, for decades. The only effect of the infection is chronic inflammation with periductal fibrosis, but if the parasite numbers increase significantly (gt;100) this can cause obstruction of small-diameter ducts, resulting in cholangitis. Large-caliber ducts are typically spared, in particular those that are extrahepatic.
4.2.4.3 Fascioliasis
Parasites reach the liver through the peritoneal cavity, after perforating the duodenal wall. In a first phase, called hepatic phase, they cause fever, abdominal pain and hepatomegaly: a strong indication is the „tunnel and caves sign”, an imaging sign produced by subcapsular serpiginous structures and by clusters of parenchymal nodules [20].
In the subsequent biliary phase, the symptoms become those of biliary colic or cholangitis: imaging shows dilated intrahepatic and extrahepatic ducts, with endoluminal filling defects and thickening, as well as signs of parietal inflammation.
4.2.4.4 Ascariasis
Ascaris lumbricoides can colonize both biliary and pancreatic ducts, but has a predilection for the common bile duct in patients who have undergone cholecystectomy, or surgical or endoscopic treatments. In such cases, parasitic secretions cause spasms of the sphincter of Oddi, with resulting biliary colic. MRCP shows a morphologically linear hypointense filling defect within the hyperintense bile.
When the intrahepatic ductal tree is colonized, necrosis and abscesses can follow.
4.2.4.5 Schistosomiasis
Signs of schistosomiasis can appear on MRCP before cholestasis indexes are altered, and they consist of a relatively poor representation of first-order and second-order ducts and biliary duct irregularity, with areas of focal narrowing.
4.2.5 HIV-related Cholangitis
HIV-related cholangitis resembles sclerosing cholangitis, but is associated with papillary stenosis and long extrahepatic bile duct structures. It may affect HIV-positive patients with CD4 counts of <100/μl. Cryptosporidium parvum and cytomegalovirus are the most common pathogens.
Right-upper-quadrant pain, normal bilirubin and increased alkaline phosphatase are typical findings, while jaundice is uncommon. Histologically, HIV-related cholangitis shows a marked periductal inflammatory response with interstitial edema, interstitial inflammatory cell infiltrates and necrotic biliary epithelium.
The pathological classification system for HIV-related cholangitis is as follows:
Type I: distal common bile duct stricture from ampullary stenosis (15–20% of patients).
Type II: diffuse intrahepatic biliary strictures (20% of patients).
Type III: combined types I and II (50% of patients).
Type IV: long-segment common bile duct stricture with possible ulceration (15% of patients).
Type V: acalculous cholecystitis.
Typical imaging features include intrahepatic and extrahepatic biliary dilatation, predominant left-sided biliary involvement, saccular dilatations, debris, pruning, irregular thickening of the common bile duct, papillary stenosis and acalculous cholecystitis.
MRI shows thickening and enhancement of the common bile duct walls, as well as enhancement of the intrahepatic bile duct walls [18]; these are seen easily on contrastenhanced, fat-saturated T1-weighted images. MRCP findings of primary sclerosing cholangitis are characterized by long extrahepatic bile duct strictures, described as one of the cholangiographic patterns suggestive of AIDS cholangiopathy [25, 26] (Fig. 4.7).
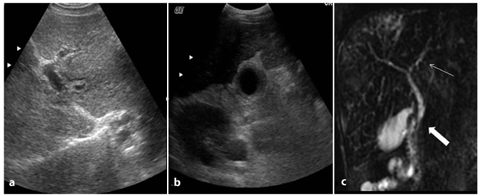
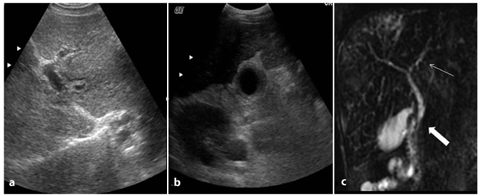
Fig. 4.7
HIV-correlated cholangitis. a, b Features of HIV-correlated cholangitis, shown in these two ultrasound images, shared with other biliary inflammatory conditions, such as primary sclerosing cholangitis, include intrahepatic duct strictures, pruning, dilatation and thickening of the walls of the bile ducts and gallbladder. c A coronal T2-weighted image showing a long extrahepatic stricture (thin arrow) and sphincter of Oddi stenosis (thick arrow); these signs are helpful in the differential diagnosis between HIV-correlated cholangitis and other forms of cholangitis
Biliary strictures in AIDS cholangiopathy are indistinguishable from those in primary sclerosing cholangitis in the absence of segmental extrahepatic biliary strictures; clinical history may help to distinguish one from the other, and diagnosis is based on duodenal/papillary biopsy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree