Fig. 13.1
Acute cholecystitis with a cystic duct stone. (a). A cystic duct stone (arrow) is well visualized on precontrast CT image. (b, c) Diffuse wall thickening with mild inner layer enhancement (arrows) and pericholecystic fat infiltration (arrowhead) with distended lumen are seen on contrast-enhanced CT
13.7.2 Gallbladder Wall Edema
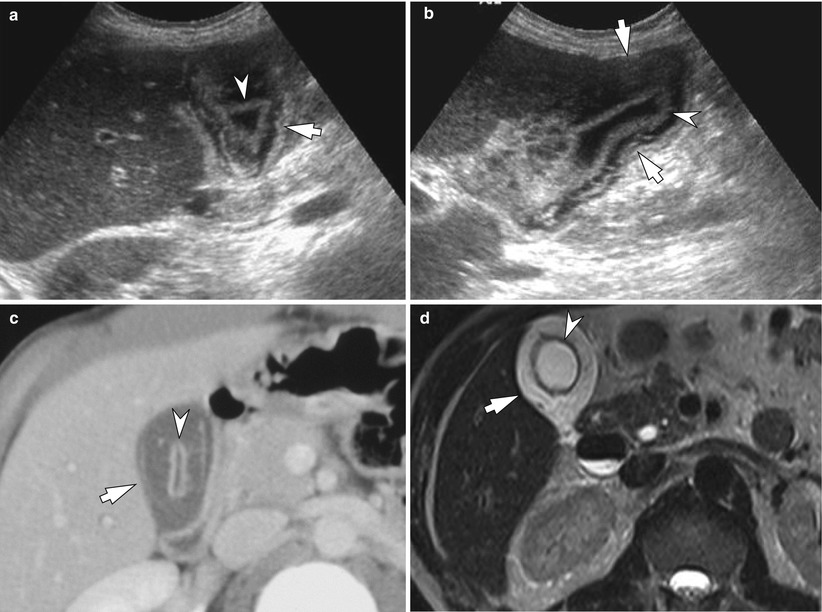
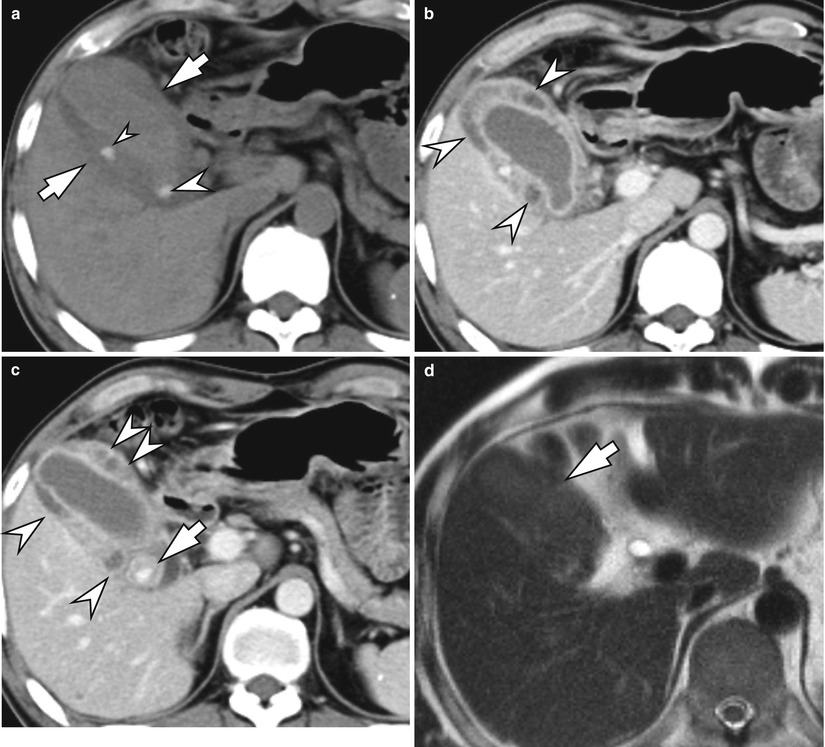
Fig. 13.2
Gallbladder wall edema. (a, b). Diffuse wall thickening of the gallbladder with loose outer layer (arrows) and intact inner layer (arrowheads) is seen on ultrasound, which represents edema of the perimuscular connective tissue and intact mucosa. The lumen is not distended. (c, d) Contrast-enhanced CT and T2-weighted MR images show diffuse wall edema (arrows) and intact inner layer (arrowheads). Gallbladder wall thickening can be caused by chronic cholecystitis, liver dysfunction, ascites, hypoproteinemia, heart failure, renal disease, multiple myeloma, and so on as well as acute cholecystitis
13.7.3 Acute Gangrenous Cholecystitis
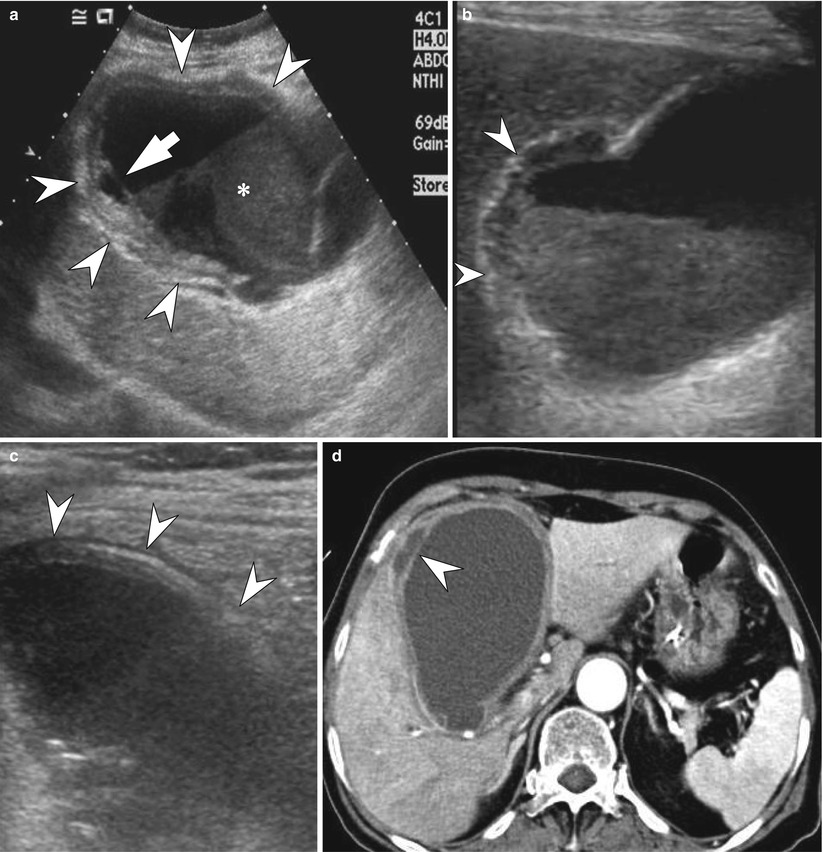
Fig. 13.3
Acute gangrenous cholecystitis. (a) Irregular gallbladder wall thickening (arrowheads) with detached mucosa (arrow) is seen on ultrasound. Echogenic sludge is seen (asterisk). (b). Deep ulceration (arrowheads) with loss of normal wall layer toward gallbladder bed is seen on ultrasound. (c) Striated wall thickening is seen (arrowheads). (d) CT reveals a markedly distended gallbladder with detached mucosa (arrowhead) in the lumen. The gallbladder wall is diffusely thickened. Heterogeneous liver enhancement seen in right lobe of the liver may indicate the coexistence of cholangiohepatitis or reactive hyperemia
13.7.4 Acute Hemorrhagic Cholecystitis
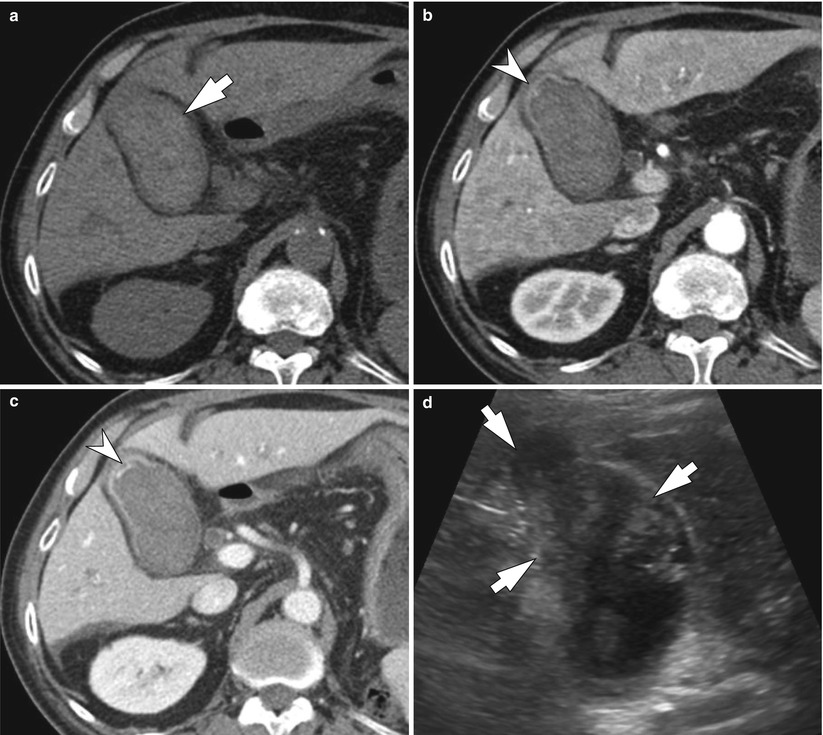
Fig. 13.4
Acute hemorrhagic cholecystitis. He was being treated by sunitinib malate for the treatment of metastatic renal cell carcinoma. Sunitinib malate can cause mild or serious bleeding as a side effect. He was presented with abdominal pain and melena. (a) Precontrast CT shows a distended gallbladder with high attenuation contents (arrow). (b) Arterial phase CT shows a focal thickening of the fundus with a faint contrast extravasation (arrowhead). (c) Portal venous phase CT shows more extravasation of contrast media in the lumen, indicating intraluminal active bleeding (arrowhead). (d) Abundant amount of echogenic material (arrows) fills the fundus and body of the gallbladder
13.7.5 Emphysematous Cholecystitis

Fig. 13.5
Emphysematous cholecystitis. (a) Air (arrows) exists in the lumen of the distended gallbladder on precontrast CT. (b) Intramural airs (arrow) are seen, strongly indicating emphysematous cholecystitis on precontrast CT
13.7.6 Emphysematous Cholecystitis
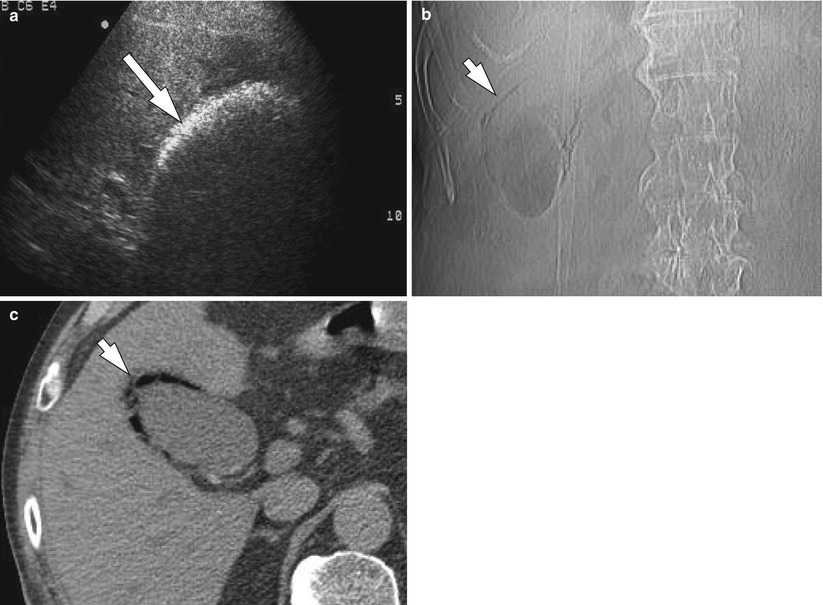
Fig. 13.6
Emphysematous cholecystitis. (a) Curvilinear band with very bright echogenicity is seen in the gallbladder fossa. It generates dirty posterior shadowing which is typically seen from the air bubbles. (b) Plain radiograph shows curvilinear gas density in the right upper quadrant (arrow), which represents gas within the gallbladder wall. (c) Precontrast CT shows air within the gallbladder wall (arrow)
13.7.7 Gallbladder Perforation
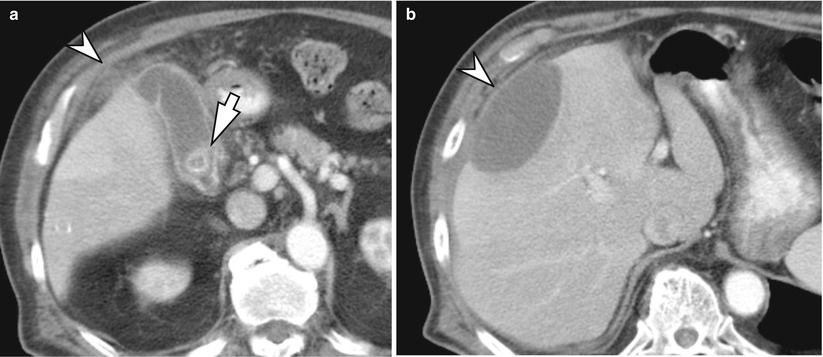
Fig. 13.7
Gallbladder perforation. (a) Distended gallbladder has a gallstone (arrow) and pericholecystic fat infiltration (arrowhead). Hyperemia appears in the adjacent liver. (b) A lentiform fluid collection anterior to the right lobe of the liver with mass effect is seen (arrowhead). The fluid collection is in contact with the fundus (not shown). It indicates subcapsular biloma by perforation of the fundus of the gallbladder
13.7.8 Gallbladder Perforation

Fig. 13.8
Gallbladder perforation. Perforation into gallbladder bed (arrowhead) is seen along with distended gallbladder
13.7.9 Chronic Calculous Cholecystitis with Cholesterolosis
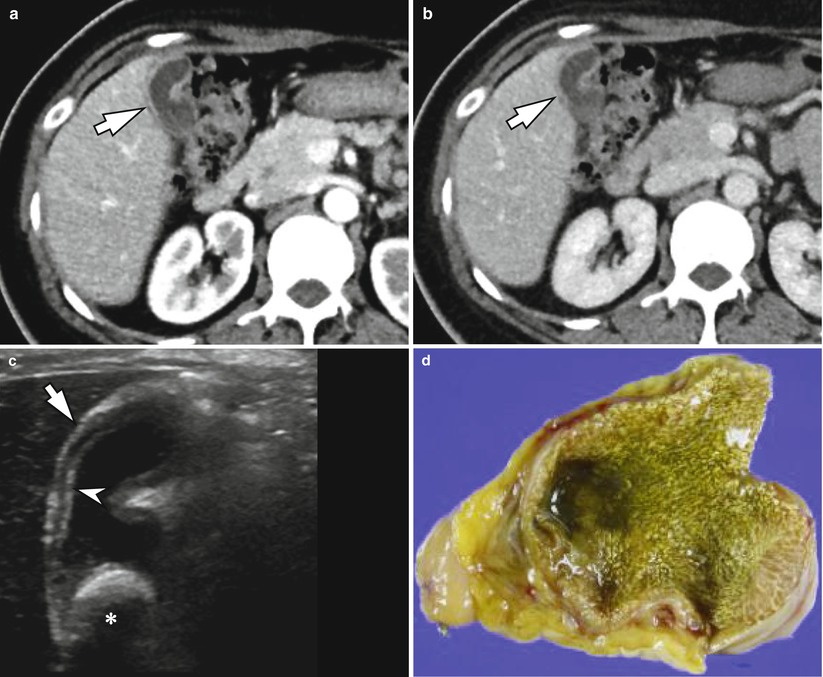
Fig. 13.9
Chronic calculous cholecystitis with cholesterolosis. (a, b) Arterial phase (a) and portal venous phase (b) images show mild thickening of whole gallbladder wall and slight contraction of the lumen (arrows). However, the presence of stone cannot be determined on these CT images. (c) Ultrasound also shows thickening of the gallbladder wall (arrow) and a large stone (asterisk). Arrowhead indicates prominently hyperechoic and thickened mucosal layer, which most likely represents cholesterol deposition in mucosal layer (cholesterolosis). (d) On gross specimen, mucosal surface shows diffuse yellowish material deposition by cholesterol. It was confirmed as chronic cholecystitis with cholesterolosis
13.7.10 Cholecystoduodenal Fistula Causing Gallstone Ileus
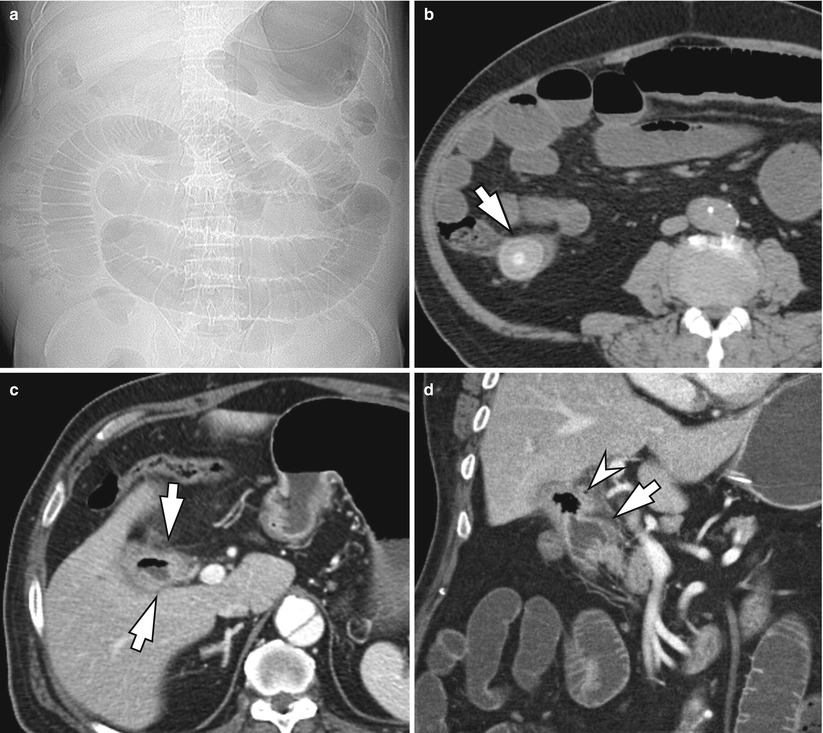
Fig. 13.10
Cholecystoduodenal fistula causing gallstone ileus. (a) On plain radiograph, markedly dilated small bowel loops are seen, indicating mechanical ileus. (b) Precontrast CT shows a large stone (arrow) within terminal ileum, obstructing small bowel loop. (c) Enhanced CT shows irregular wall thickening of gallbladder containing air (arrows). (d. On coronal CT image, the gallbladder (arrowhead) is connected with adjacent duodenum (arrow), indicating the presence of cholecystoduodenal fistula