Cognitive impairment from a major stroke as a consequence of carotid disease is an acknowledged clinical outcome; however, cognitive impairment without major stroke is open to discussion. The three recognized mechanisms for cognitive dysfunction from internal carotid artery are microembolization, white-matter disease, and hypoperfusion. The last has been most difficult to characterize physiologically. In this article, the authors review evidence supporting the existence of chronic ischemia in the brain and its direct impact on cognitive functions. By incorporating the pathophysiology of chronic ischemia into the algorithm of the management of carotid artery disease, we may be able to extend the goals of carotid artery revascularization beyond merely preventing stroke to include preventing or reversing cognitive decline.
Chronic ischemia is a progressive condition caused by cerebral hypoperfusion that ultimately leads to neuronal death. The impact of hypoperfusion on cerebral function has been described in various clinical settings. Acutely systemic hypoperfusion can cause dizziness, visual disturbance, impaired cognition, and loss of consciousness, but, in that setting, cerebral hypoperfusion is easily reversible by laying the patient horizontally and restoring an adequate level of blood pressure. In subacute and chronic settings, cognitive brain functions are affected when the brain is subject to a sustained reduction of blood flow, as may occur in carotid artery disease. The degree, volume, and the duration of hypoperfusion are all variables that influence the brain’s response to chronic ischemia. Additional factors, such as pre-existing white-matter disease, cardiac status, thromboembolism, and medical comorbidities, all may contribute to determining whether carotid artery disease produces cognitive impairment. In this article, the authors review the clinical evidence for cognitive dysfunction in carotid artery disease and consider the evidence for chronic ischemia as an underlying pathophysiologic mechanism for cognitive impairment.
Evidence of impaired cognition due to carotid artery disease
Cognitive impairment has been reported in a wide spectrum of clinical studies in patients who have carotid disease, most frequently in global terms rather than as a specific, neurocognitive profile. Fischer was the first to postulate an association between cerebral hypoperfusion and dementia, based on a necropsy study of a demented patient who had bilateral carotid occlusion. A few years later, Carey and colleagues reported dementia in four patients who had bilateral carotid occlusion and two patients who had unilateral carotid artery occlusion. Cognitive dysfunction that results from large cortical infarction in territories supplied by carotid arteries is easy to understand; the causative relationship between carotid disease and cognitive functions is less clear when major stroke does not occur.
Bakker and colleagues performed an extensive review of literature evaluating cognitive dysfunction in patients with occlusive carotid disease. The lack of recovery from injury due to infarction was not the only means of producing cognitive dysfunction with carotid disease ; cognitive impairment was documented among patients who had transient ischemic attack and patients with no focal neurologic deficits . Bakker and colleagues conducted their own study of 39 patients with carotid occlusion who had ipsilateral cerebral or retinal transient ischemic attacks but no stroke on MR imaging. The investigators illustrated significant cognitive impairment in these patients, even in those who had only retinal symptoms and negative MR imaging. Among studies that documented cognitive dysfunction without stroke, two noted a generalized impairment , three demonstrated focal deficits (memory , learning , psychomotor , and problem solving ), and two did not specify the nature of cognitive deficits . Several studies have also demonstrated no relationship between carotid stenosis and cognitive dysfunction .
Although associations between carotid stenosis and cognitive impairment have been reported widely, the question of cause and effect has been controversial. Mathiesen and colleagues assessed neuropsychologic performance in 189 asymptomatic carotid stenosis patients and found that scores were significantly lower in tests of attention, memory, and psychomotor and motor functioning, compared with 202 patients who had no carotid disease. Cortical infarcts were distributed equally between patients and controls, however, from which they concluded that cognitive dysfunction was unlikely to be caused by emboli from the carotid arteries. Furthermore, because the study patients had relatively low-grade stenosis, hemodynamic insufficiency was also deemed an unlikely causative mechanism. Because lacunar infarcts were more prevalent in the stenosis group, the investigators concluded that carotid stenosis was no more than a marker for underlying generalized atherosclerosis, which was the direct culprit for cognitive dysfunction.
The notion that carotid atherosclerosis is simply a marker for underlying vascular disease was supported also by correlations between neuropsychologic decline and common carotid artery intima-media thickness because intima-media thickness reflects the burden of atherosclerosis without requiring stenosis of the internal carotid artery. Hofman and colleagues , for example, reported that the presence of carotid plaque and intima-media thickness was associated positively with Alzheimer’s disease and vascular dementia. On the other side of the argument, Johnston and colleagues reasoned that if carotid stenosis was simply a marker of vascular disease, then a similar pattern of cognitive dysfunction should be observed with either left-sided or right-sided carotid disease when using a test such as the Modified Mini-Mental Status Exam, which assesses mainly left hemisphere function. They prospectively followed for 5 years, 4006 patients from the Cardiovascular Health Study, in which high-grade stenosis was present in the left internal carotid artery in 28 participants and the right internal carotid artery in 20 participants. They found that, after adjusting for other vascular risk factors, left-sided stenosis (>75%) was disproportionately associated with cognitive impairment on the Modified Mini-Mental Status Exam, suggesting that carotid stenosis was, in fact, a causative variable. In this study, intima-media thickness was not found to be associated independently with cognitive impairment after adjustment of other risk factors.
Mechanisms
Hypoperfusion
The refinement of new imaging techniques that measure cerebral hemodynamics directly has advanced our understanding of the relationship between hypoperfusion in carotid diseases and cognitive impairment. Tatemichi and colleagues documented the case of a 55-year-old man with bilateral internal carotid and unilateral vertebral artery occlusions presenting with a subacute onset of severe behavioral and cognitive changes. Quantitative cerebral blood flow (CBF) and positron emission tomography (PET) studies showed a 40% to 50% reduction in blood flow and metabolism. Following extracranial/intracranial (EC/IC) bypass, the patient demonstrated an appreciable neuropsychologic improvement that was accompanied by significant increases in CBF and metabolism. Another study integrating data about cognitive performance, CBF, and metabolism showed that 25 patients who had unilateral carotid occlusion and poor neuropsychologic performance had significantly reduced regional CBF (rCBF), regional cerebrovascular reactivity, and regional cerebral metabolic rate for oxygen (rCMRO 2 ) . Another PET study showed that 12 patients who had significant cognitive dysfunction had a wide spread of metabolic derangement . Finally, using single photon emission computed tomography (SPECT), Tsuda and colleagues documented the case of a patient diagnosed with total occlusion left internal carotid artery siphon presenting with a generalized, cognitive impairment in the ipsilateral hemisphere. His cognitive status was coupled to an extensive hypoperfusion area in the left anterior parietal and parietotemporal cortex.
Additional evidence for the effects of chronic cerebral hypoperfusion on cognitive function comes from the cardiac literature. End-stage heart failure may produce a state of global ischemia of the brain resembling the state resulting from hypoperfusion due to carotid disease. Recent studies have found that as many as 35% to 50% of patients who have heart failure have a cognitive dysfunction . The pathophysiology of cognitive impairment in end-stage heart failure has been attributed to hypoperfusion and microembolism . The most widely accepted view is that decreased cardiac pumping efficiency directly influences cerebral perfusion . In human subjects, global CBF reductions have been reported in heart failure patients using functional imaging studies with SPECT .
In a pioneering study, Gruhn and colleagues demonstrated that CBF was reduced by approximately 31% in 12 patients (36 ± 1 mL/min per 100 g), when compared with 12 healthy subjects (52 ± 5 mL/min per 100 g) ( P < .05). Among the studied subjects, five patients underwent heart transplantation that resulted in a significant increase in CBF, from 35 ± 3 to 50 ± 3 mL/min per 100 g within the first month postoperation ( P < .05). Another study showed that cardiac recipients had an increase in cardiac output that resulted in a concomitant increase in middle cerebral artery (MCA)-mean flow velocity . Although neither study included neuropsychologic testing of patients, the significant 31% increase in CBF may offer a physiologic explanation for clinical reports of neuropsychologic improvement following cardiac transplantation .
Data from studies prospectively evaluating the cognitive status of patients undergoing cardiac transplants contain some evidence for cognitive change. One report failed to demonstrate significant cognitive improvement in 54 patients who were assessed preoperatively, 20 of whom completed postoperative testing . On the other hand, three prospective reports evaluating cognition among cardiac recipients showed improvement in cognitive performance of various functions . The enhanced cortical perfusion following transplant is felt to be the cause of improvement in attention span and reduction in depression and anxiety .
Pacemaker implantation is another approach by which cognition can be improved potentially in patients who have heart dysfunction . Pacemakers improve heart rate, resulting in increased CBF levels . Illustratively, Koide and colleagues reported an improvement in CBF and verbal intelligence following pacemaker implantation in 14 bradycardiac patients.
Carotid artery stenting/carotid endarterectomy
In a manner analogous to the cognitive improvement following CBF increases with treatment of heart dysfunction, studies that demonstrate cognitive improvement following revascularization support the hypoperfusion hypothesis.
Many studies have evaluated the effect of carotid endarterectomy (CE) on cognitive functioning. Results have been variable, ranging from benefit, to decrease, to no change. In reviews by Irvine and colleagues and Lunn and colleagues in the late 1990s, 16 of 28 studies (57%) reported cognitive improvement following CE, whereas deterioration was reported in 1 report (4%) and no change in 11 reports (39%).
Subsequent studies of CE have shown some support for the hypoperfusion hypothesis. Among those demonstrating cognitive benefit , the positive impact on cognition was attributed to a significant increase in CBF or to a reduced preoperative cerebral perfusion reserve . However, other studies have found no restorative effect on cognition . A recent study showed that after 44 months of postoperative follow-up, cognitive dysfunction occurred in almost one half of patients who underwent CE, and the decline was more prominent in symptomatic patients who had left internal carotid artery disease than in asymptomatic patients who had left internal carotid artery disease or in patients who had right internal carotid artery disease, either symptomatic or asymptomatic .
Some studies investigated side-specific cognitive effects, based on the premise that restoration of hemodynamic physiologic conditions would be more beneficial to the cognitive functions of the cerebral hemisphere ipsilateral to the operated side. This hypothesis stems from pre- and postoperative MR imaging studies, in which ipsilateral white-matter changes were reported to be reversible to a certain extent by endarterectomy . However, no solid conclusion was reached in these studies regarding side-related benefits of CE on cognition .
Controversy prevails and, consequently, final conclusions regarding the impact of CE on cognition cannot be reached. The wide spectrum in results, ranging from a decline, to no effect, to a benefit, has been explained by periprocedural complications and differences in methodologic factors, such as battery of neuropsychologic testing, sample size and use of control population, severity of carotid stenosis, associated comorbidities, and time to postoperative follow-up . Because of the neurologic variability, no consistent cognitive profile exists for patients who have carotid disease.
Carotid artery stenting came into routine clinical practice only in the last decade; for this reason, knowledge about the effect of carotid artery stenting on cognition is limited, but it is presumed to follow the same principle as CE. Lehrner and colleagues studied the cognitive outcome of 20 patients, 9 symptomatic with transient ischemic attack and 11 asymptomatic, 6 months after unilateral carotid stenting. Most patients had no significant change in cognitive functioning. On the other hand, 10 patients assessed 48 hours post-op showed an improvement of cognitive status following carotid artery stenting . Another study compared cognitive outcome in 20 patients undergoing carotid angioplasty without stenting with 26 patients undergoing CE. At 6 weeks follow-up, five patients in each group had a comparable decline in cognition . As with CE studies, it was shown that improvement in perfusion parameters following stent deployment, carotid or vertebrobasilar, was a significant predictor of cognitive improvement .
Extracranial/intracranial bypass
EC/IC bypass surgery was used commonly during the 1970s and early 1980s to treat patients who had total occlusion of carotid arteries and were not candidates for carotid endarterectomy. The fact that intellectual decline has been linked to chronic ischemia set the ground for investigators to address the efficacy of EC/IC bypass in restoring cognitive functions. The concept of blood flow restitution is the pillar on which EC/IC bypass surgery is based. However, the effectiveness of EC/IC bypass was reported initially only in case studies. For instance, Nielsen and colleagues found that among 33 patients undergoing EC/IC bypass, 23 had preoperative impairment of cognition that improved 3 months after surgery. A case series of 38 patients being referred for EC/IC bypass showed an improvement in scores of neuropsychologic tests of processing speed and memory . Binder and colleagues compared the cognition of 12 patients undergoing EC/IC bypass with 7 patients who had internal carotid artery occlusion treated medically. Limited to only 2 months of follow-up, no significant difference was detected. Of note, the previous studies had no control subjects, nor any hemodynamic data.
Reports from that era that assessed CBF changes following EC/IC bypass are also conflicting. Younkin and colleagues conducted a study without controls and evaluated CBF with a 133 Xe inhalation technique in a series of 44 patients undergoing EC/IC bypass. Neuropsychologic performance increased at 3 months and further improvement was detected at 9 months; however, the clinical improvement was not associated with similar changes in CBF values. A maximum increase in CBF at 3 months was noted, followed by a decrease to preoperative baseline levels by 9 months. Yonekura and colleagues found no changes in CBF measures at 6 months and decreased measures at 2 years, but Halsey and colleagues reported a significant increase in CBF at 6 months.
The initial evidence regarding the impact of EC/IC bypass on hemodynamics and cognitive functions is contentious. However, several studies did correlate cognitive postoperative changes with cerebral hemodynamics. Using SPECT, Tsuda and colleagues documented a case where the recovery in blood flow and metabolic rate following EC/IC bypass was translated into improvement in both neurologic and cognitive functions. During a period of 3 to 9 months postoperatively, rCBF was normalized, whereas cognitive improvement was witnessed in the first 2 postoperative months and maintained over a 3-year follow-up. In a more recent investigation, Sasoh and colleagues studied 25 patients who had chronic cerebral ischemia due to internal carotid occlusion, who underwent pre- and postoperative measurement of CBF and metabolism using PET. They demonstrated that elevated regional oxygen extraction rate and reduced cerebral metabolic rate for oxygen (CMRO 2 ) were associated strongly with cognitive impairment. Postoperatively, the hemodynamic factors increased significantly, accompanied by significant improvement in verbal IQ, performance, and full-scale IQ scores. Their hemodynamic findings were consistent with previous studies that demonstrated restitution of rCBF, oxygen extraction rate and CMRO 2 following EC/IC bypass . This effect of EC/IC bypass on cognition in patients who had stage II hemodynamic failure was the basis for initiating the currently active Randomized Evaluation of Carotid Occlusion and Neurocognition, in which patients’ cognitive function over 2 years will be compared in an National Institutes of Health–sponsored, prospective, randomized clinical trial. Patients will receive either EC/IC bypass or best medical therapy alone as part of the Carotid Occlusion Surgery Study.
Embolization
In addition to hypoperfusion, brain damage secondary to carotid disease may be produced by episodic embolization of platelet, thrombotic, or cholesterol material with microinfarction of cerebral tissue . Using random transcranial Doppler monitoring, spontaneous microemboli can be detected in 21% to 60% of patients who have documented carotid disease .
Emboli reaching one hemisphere or retina commonly stem from the ipsilateral carotid, and, in particular, from the distal or proximal stump, or from atherosclerotic plaques in the common carotid artery . Transhemispheric emboli (ie, microemboli) causing ischemic events in the contralateral hemisphere also may occur . Ischemic events due to microemboli occurring in the brain hemisphere ipsilateral to the occluded internal carotid artery are reduced after clipping of the proximal stump , following endarterectomy in contralateral internal carotid artery stenosis , or after use of antithrombotic agents .
Whether microembolism from carotid disease is clinically significant remains an open question. Droste and colleagues detected up to 142 embolic signals per hour in patients who had carotid stenosis and a recent transient ischemic attack; however, symptoms developing as a result of these embolic showers occur at a surprisingly low rate , perhaps because of collateral washout. Older age, hypertension, diabetes, or small-vessel disease appear to increase the susceptibility of the brain to injury from microemboli . Acute ischemic events also have a size threshold , larger emboli being more likely to cause symptoms . Furthermore, transient symptoms might go unnoticed in patients experiencing microembolization during sleep .
Even if microembolism does not induce immediate consequences, delayed sequelae are possible. Embolic fragments may trigger an inflammatory process that, in time, leads to cellular infiltration and fibrosis . This phenomenon could account for late deterioration in cognitive functions, as it does in patients following coronary artery bypass .
Lacunar disease
A growing literature suggests that white-matter lesions are involved in the pathogenesis of cognitive impairment , more so in the periventricular than subcortical regions , periventricular lesions showing a strong relationship with memory, psychomotor, and global cognitive dysfunctions . Severe carotid disease of 70% stenosis is associated with deep white-matter lesions and lacunar infarction .
One study showed that carotid artery narrowing of more than 50% is an independent predictor of lacunar infarction , which, in turn, is associated significantly with attention deficits and frontal lobe dysfunction. The clinical significance of asymptomatic cerebral microinfarction was recognized in the Rotterdam Scan Study, which showed that the incidence of silent infarcts detected by MR imaging among healthy elderly patients doubles the risk of developing cognitive decline on follow-up . Suffering additional silent infarcts appears to promote further cognitive deterioration . These findings were reproduced in two large studies, the Atherosclerosis Risk in Communities Study and the Cardiovascular Health Study . Silent infarcts of both white matter and cortical gray matter also have been correlated with poor cognition .
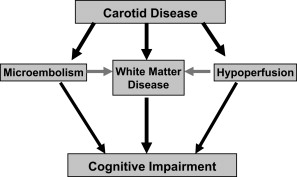
From the clinical data presented, it appears that cognitive impairment in carotid disease may result from small-vessel disease, microembolism, or chronic hypoperfusion ( Fig. 1 ). It is the last that has been most difficult to characterize physiologically. What follows is a review of the experimental literature that supports the existence of chronic ischemia in the brain.
Mechanisms
Hypoperfusion
The refinement of new imaging techniques that measure cerebral hemodynamics directly has advanced our understanding of the relationship between hypoperfusion in carotid diseases and cognitive impairment. Tatemichi and colleagues documented the case of a 55-year-old man with bilateral internal carotid and unilateral vertebral artery occlusions presenting with a subacute onset of severe behavioral and cognitive changes. Quantitative cerebral blood flow (CBF) and positron emission tomography (PET) studies showed a 40% to 50% reduction in blood flow and metabolism. Following extracranial/intracranial (EC/IC) bypass, the patient demonstrated an appreciable neuropsychologic improvement that was accompanied by significant increases in CBF and metabolism. Another study integrating data about cognitive performance, CBF, and metabolism showed that 25 patients who had unilateral carotid occlusion and poor neuropsychologic performance had significantly reduced regional CBF (rCBF), regional cerebrovascular reactivity, and regional cerebral metabolic rate for oxygen (rCMRO 2 ) . Another PET study showed that 12 patients who had significant cognitive dysfunction had a wide spread of metabolic derangement . Finally, using single photon emission computed tomography (SPECT), Tsuda and colleagues documented the case of a patient diagnosed with total occlusion left internal carotid artery siphon presenting with a generalized, cognitive impairment in the ipsilateral hemisphere. His cognitive status was coupled to an extensive hypoperfusion area in the left anterior parietal and parietotemporal cortex.
Additional evidence for the effects of chronic cerebral hypoperfusion on cognitive function comes from the cardiac literature. End-stage heart failure may produce a state of global ischemia of the brain resembling the state resulting from hypoperfusion due to carotid disease. Recent studies have found that as many as 35% to 50% of patients who have heart failure have a cognitive dysfunction . The pathophysiology of cognitive impairment in end-stage heart failure has been attributed to hypoperfusion and microembolism . The most widely accepted view is that decreased cardiac pumping efficiency directly influences cerebral perfusion . In human subjects, global CBF reductions have been reported in heart failure patients using functional imaging studies with SPECT .
In a pioneering study, Gruhn and colleagues demonstrated that CBF was reduced by approximately 31% in 12 patients (36 ± 1 mL/min per 100 g), when compared with 12 healthy subjects (52 ± 5 mL/min per 100 g) ( P < .05). Among the studied subjects, five patients underwent heart transplantation that resulted in a significant increase in CBF, from 35 ± 3 to 50 ± 3 mL/min per 100 g within the first month postoperation ( P < .05). Another study showed that cardiac recipients had an increase in cardiac output that resulted in a concomitant increase in middle cerebral artery (MCA)-mean flow velocity . Although neither study included neuropsychologic testing of patients, the significant 31% increase in CBF may offer a physiologic explanation for clinical reports of neuropsychologic improvement following cardiac transplantation .
Data from studies prospectively evaluating the cognitive status of patients undergoing cardiac transplants contain some evidence for cognitive change. One report failed to demonstrate significant cognitive improvement in 54 patients who were assessed preoperatively, 20 of whom completed postoperative testing . On the other hand, three prospective reports evaluating cognition among cardiac recipients showed improvement in cognitive performance of various functions . The enhanced cortical perfusion following transplant is felt to be the cause of improvement in attention span and reduction in depression and anxiety .
Pacemaker implantation is another approach by which cognition can be improved potentially in patients who have heart dysfunction . Pacemakers improve heart rate, resulting in increased CBF levels . Illustratively, Koide and colleagues reported an improvement in CBF and verbal intelligence following pacemaker implantation in 14 bradycardiac patients.
Carotid artery stenting/carotid endarterectomy
In a manner analogous to the cognitive improvement following CBF increases with treatment of heart dysfunction, studies that demonstrate cognitive improvement following revascularization support the hypoperfusion hypothesis.
Many studies have evaluated the effect of carotid endarterectomy (CE) on cognitive functioning. Results have been variable, ranging from benefit, to decrease, to no change. In reviews by Irvine and colleagues and Lunn and colleagues in the late 1990s, 16 of 28 studies (57%) reported cognitive improvement following CE, whereas deterioration was reported in 1 report (4%) and no change in 11 reports (39%).
Subsequent studies of CE have shown some support for the hypoperfusion hypothesis. Among those demonstrating cognitive benefit , the positive impact on cognition was attributed to a significant increase in CBF or to a reduced preoperative cerebral perfusion reserve . However, other studies have found no restorative effect on cognition . A recent study showed that after 44 months of postoperative follow-up, cognitive dysfunction occurred in almost one half of patients who underwent CE, and the decline was more prominent in symptomatic patients who had left internal carotid artery disease than in asymptomatic patients who had left internal carotid artery disease or in patients who had right internal carotid artery disease, either symptomatic or asymptomatic .
Some studies investigated side-specific cognitive effects, based on the premise that restoration of hemodynamic physiologic conditions would be more beneficial to the cognitive functions of the cerebral hemisphere ipsilateral to the operated side. This hypothesis stems from pre- and postoperative MR imaging studies, in which ipsilateral white-matter changes were reported to be reversible to a certain extent by endarterectomy . However, no solid conclusion was reached in these studies regarding side-related benefits of CE on cognition .
Controversy prevails and, consequently, final conclusions regarding the impact of CE on cognition cannot be reached. The wide spectrum in results, ranging from a decline, to no effect, to a benefit, has been explained by periprocedural complications and differences in methodologic factors, such as battery of neuropsychologic testing, sample size and use of control population, severity of carotid stenosis, associated comorbidities, and time to postoperative follow-up . Because of the neurologic variability, no consistent cognitive profile exists for patients who have carotid disease.
Carotid artery stenting came into routine clinical practice only in the last decade; for this reason, knowledge about the effect of carotid artery stenting on cognition is limited, but it is presumed to follow the same principle as CE. Lehrner and colleagues studied the cognitive outcome of 20 patients, 9 symptomatic with transient ischemic attack and 11 asymptomatic, 6 months after unilateral carotid stenting. Most patients had no significant change in cognitive functioning. On the other hand, 10 patients assessed 48 hours post-op showed an improvement of cognitive status following carotid artery stenting . Another study compared cognitive outcome in 20 patients undergoing carotid angioplasty without stenting with 26 patients undergoing CE. At 6 weeks follow-up, five patients in each group had a comparable decline in cognition . As with CE studies, it was shown that improvement in perfusion parameters following stent deployment, carotid or vertebrobasilar, was a significant predictor of cognitive improvement .
Extracranial/intracranial bypass
EC/IC bypass surgery was used commonly during the 1970s and early 1980s to treat patients who had total occlusion of carotid arteries and were not candidates for carotid endarterectomy. The fact that intellectual decline has been linked to chronic ischemia set the ground for investigators to address the efficacy of EC/IC bypass in restoring cognitive functions. The concept of blood flow restitution is the pillar on which EC/IC bypass surgery is based. However, the effectiveness of EC/IC bypass was reported initially only in case studies. For instance, Nielsen and colleagues found that among 33 patients undergoing EC/IC bypass, 23 had preoperative impairment of cognition that improved 3 months after surgery. A case series of 38 patients being referred for EC/IC bypass showed an improvement in scores of neuropsychologic tests of processing speed and memory . Binder and colleagues compared the cognition of 12 patients undergoing EC/IC bypass with 7 patients who had internal carotid artery occlusion treated medically. Limited to only 2 months of follow-up, no significant difference was detected. Of note, the previous studies had no control subjects, nor any hemodynamic data.
Reports from that era that assessed CBF changes following EC/IC bypass are also conflicting. Younkin and colleagues conducted a study without controls and evaluated CBF with a 133 Xe inhalation technique in a series of 44 patients undergoing EC/IC bypass. Neuropsychologic performance increased at 3 months and further improvement was detected at 9 months; however, the clinical improvement was not associated with similar changes in CBF values. A maximum increase in CBF at 3 months was noted, followed by a decrease to preoperative baseline levels by 9 months. Yonekura and colleagues found no changes in CBF measures at 6 months and decreased measures at 2 years, but Halsey and colleagues reported a significant increase in CBF at 6 months.
The initial evidence regarding the impact of EC/IC bypass on hemodynamics and cognitive functions is contentious. However, several studies did correlate cognitive postoperative changes with cerebral hemodynamics. Using SPECT, Tsuda and colleagues documented a case where the recovery in blood flow and metabolic rate following EC/IC bypass was translated into improvement in both neurologic and cognitive functions. During a period of 3 to 9 months postoperatively, rCBF was normalized, whereas cognitive improvement was witnessed in the first 2 postoperative months and maintained over a 3-year follow-up. In a more recent investigation, Sasoh and colleagues studied 25 patients who had chronic cerebral ischemia due to internal carotid occlusion, who underwent pre- and postoperative measurement of CBF and metabolism using PET. They demonstrated that elevated regional oxygen extraction rate and reduced cerebral metabolic rate for oxygen (CMRO 2 ) were associated strongly with cognitive impairment. Postoperatively, the hemodynamic factors increased significantly, accompanied by significant improvement in verbal IQ, performance, and full-scale IQ scores. Their hemodynamic findings were consistent with previous studies that demonstrated restitution of rCBF, oxygen extraction rate and CMRO 2 following EC/IC bypass . This effect of EC/IC bypass on cognition in patients who had stage II hemodynamic failure was the basis for initiating the currently active Randomized Evaluation of Carotid Occlusion and Neurocognition, in which patients’ cognitive function over 2 years will be compared in an National Institutes of Health–sponsored, prospective, randomized clinical trial. Patients will receive either EC/IC bypass or best medical therapy alone as part of the Carotid Occlusion Surgery Study.
Embolization
In addition to hypoperfusion, brain damage secondary to carotid disease may be produced by episodic embolization of platelet, thrombotic, or cholesterol material with microinfarction of cerebral tissue . Using random transcranial Doppler monitoring, spontaneous microemboli can be detected in 21% to 60% of patients who have documented carotid disease .
Emboli reaching one hemisphere or retina commonly stem from the ipsilateral carotid, and, in particular, from the distal or proximal stump, or from atherosclerotic plaques in the common carotid artery . Transhemispheric emboli (ie, microemboli) causing ischemic events in the contralateral hemisphere also may occur . Ischemic events due to microemboli occurring in the brain hemisphere ipsilateral to the occluded internal carotid artery are reduced after clipping of the proximal stump , following endarterectomy in contralateral internal carotid artery stenosis , or after use of antithrombotic agents .
Whether microembolism from carotid disease is clinically significant remains an open question. Droste and colleagues detected up to 142 embolic signals per hour in patients who had carotid stenosis and a recent transient ischemic attack; however, symptoms developing as a result of these embolic showers occur at a surprisingly low rate , perhaps because of collateral washout. Older age, hypertension, diabetes, or small-vessel disease appear to increase the susceptibility of the brain to injury from microemboli . Acute ischemic events also have a size threshold , larger emboli being more likely to cause symptoms . Furthermore, transient symptoms might go unnoticed in patients experiencing microembolization during sleep .
Even if microembolism does not induce immediate consequences, delayed sequelae are possible. Embolic fragments may trigger an inflammatory process that, in time, leads to cellular infiltration and fibrosis . This phenomenon could account for late deterioration in cognitive functions, as it does in patients following coronary artery bypass .
Lacunar disease
A growing literature suggests that white-matter lesions are involved in the pathogenesis of cognitive impairment , more so in the periventricular than subcortical regions , periventricular lesions showing a strong relationship with memory, psychomotor, and global cognitive dysfunctions . Severe carotid disease of 70% stenosis is associated with deep white-matter lesions and lacunar infarction .
One study showed that carotid artery narrowing of more than 50% is an independent predictor of lacunar infarction , which, in turn, is associated significantly with attention deficits and frontal lobe dysfunction. The clinical significance of asymptomatic cerebral microinfarction was recognized in the Rotterdam Scan Study, which showed that the incidence of silent infarcts detected by MR imaging among healthy elderly patients doubles the risk of developing cognitive decline on follow-up . Suffering additional silent infarcts appears to promote further cognitive deterioration . These findings were reproduced in two large studies, the Atherosclerosis Risk in Communities Study and the Cardiovascular Health Study . Silent infarcts of both white matter and cortical gray matter also have been correlated with poor cognition .
From the clinical data presented, it appears that cognitive impairment in carotid disease may result from small-vessel disease, microembolism, or chronic hypoperfusion ( Fig. 1 ). It is the last that has been most difficult to characterize physiologically. What follows is a review of the experimental literature that supports the existence of chronic ischemia in the brain.







