CHRONIC NONINFECTIOUS INFLAMMATORY CONDITIONS: GRANULOMATOSES AND HISTIOCYTOSES
KEY POINTS
- The imaging findings in noninfectious inflammatory sinonasal conditions often have an imaging pattern strongly suggestive of the correct diagnosis or at least one that narrows the differential considerably.
- Noninfectious inflammatory sinonasal conditions often mimic benign inflammatory polyps when no other clues to diagnosis are available.
- Noninfectious inflammatory sinonasal conditions may mimic lymphoproliferative disorders.
Sinusitis is an inflammation of the paranasal sinus mucoperiosteal lining. Rhinosinusitis is currently the preferred term for this condition because the nasal mucosa is almost always simultaneously involved when sinusitis occurs.1 It is most commonly infectious or allergic, as discussed in Chapters 83 through 86. Fungal sinonasal infection is discussed separately in Chapter 86 because of its most often disparate clinical setting, occurring mainly in immune-compromised rather than otherwise healthy patients, and its difference in pathophysiology and spread patterns from the more common infections that cause rhinosinusitis.
This chapter considers noninfectious inflammatory diseases that are not only local but also often related to systemic disease. Local disease can be caused by toxins such as cocaine. The granulomatoses and histiocytoses are discussed in chapters on sarcoidosis (Chapter 18), Wegener granulomatosis (Chapter 17), and Langerhans cell histiocytosis (Chapter 19).
IMAGING APPROACH
Techniques and Relevant Aspects
The techniques of computed tomography (CT) and magnetic resonance (MR) used to study the sinuses in various clinical situations discussed in this chapter are presented in Appendixes A and B.
Pros and Cons
Uncomplicated sinusitis does not require imaging unless it is not responsive to therapy or a complication is suspected. When it is not fully responsive, the disease may be related to the far less common diseases discussed in the chapters on sinonasal neoplasia. In disease not responsive to therapy, imaging should follow a complete sinonasal examination usually including anterior rhinoscopy and nasal endoscopy by an experienced health care provider to avoid the expense and radiation of a CT study that may not be necessary.
Diagnosing complications of rhinosinusitis requires a high index of suspicion with the orbit and its contents being the most common critical area involved. CT with contrast of the sinuses and orbits is the study of choice for orbital complications. Magnetic resonance imaging (MRI) with contrast of the brain and orbits is the study of choice for intracranial complications, although contrast-enhanced CT is often sufficient for the initial evaluation of both suspected orbital and intracranial complications. If CT is not definitive in the face of strong clinical evidence of an intracranial complication, then MRI should be done. If meningitis is suspected, the patient should have cerebrospinal fluid analysis immediately regardless of the imaging findings.
SPECIFIC DISEASE/CONDITION
Granulomatoses and Histiocytoses
Etiology
The more common diseases that may present in and/or involve the nasal cavity and paranasal sinuses are discussed in general in chapters on sarcoidosis, Wegener granulomatosis, and Langerhans cell histiocytosis. A less common etiology would be Erdheim Chester disease. These are all potentially multisystem diseases. Cocaine-induced granulomatous disease of the nasal cavity may mimic these diseases until the drug use is established by history or drug screening.
Clinical Presentation
These diseases present essentially in the same manner as subacute and chronic rhinosinusitis, except for a necrotizing pattern on physical examination; those features in common are discussed in Chapters 84 and 85.
Pathophysiology and Patterns of Disease
The spread patterns of sarcoidosis (Chapter 18), Wegener granulomatosis (Chapter 17), and Langerhans cell histiocytosis (Chapter 19) are discussed in the chapters indicated. These and more rare disease such as Erdheim Chester disease and rhinoscleroma have in common some basic patterns of spread that are useful to keep in mind. This is also true for the more sinonasal changes associated with cocaine use. These are, in some cases, patterns held in common with lymphoproliferative diseases (Chapters 26 and 27). The patterns include the following:
- Predominantly nasal cavity disease with nasal polyposis with or without erosive features including nasal septal and hard palate destruction (Figs. 87.1–87.4)
- An obviously necrotizing nasal cavity process with obvious erosion of the nasal septum and turbinates (Figs. 87.1–87.4)
- Multifocal or more diffuse sinus mass with aggressive bone destruction mimicking malignant sinus pathology (Figs. 87.1–87.4)
- Isolated sinus disease with localized bone erosion
Manifestations and Findings
Computed Tomography and Magnetic Resonance Imaging
The general morphology of inflammatory disease as seen on CT and MRI is described in Chapter 13. The specific manifestations of sarcoidosis (Chapter 18), Wegener granulomatosis (Chapter 17), and Langerhans cell histiocytosis (Chapter 19) are discussed in the chapters indicated. These and more rare disease such as Erdheim Chester disease have, in some cases, patterns held in common with lymphoproliferative diseases and leukemia described in Chapters 26, 27, and 28 (Figs. 87.1–87.5).
Endoscopy
Nasal endoscopy may reveal numerous, very nonspecific findings. Generalized nasal mucosal edema, significant nasal crusting, and nasal obstruction are very common findings in patients with sinonasal involvement from systemic noninfectious disorders. Secondary effects of the underlying disease, such as acute sinusitis from ostiomeatal outflow obstruction, may also be apparent on endoscopy.2 Sarcoidosis may manifest as submucosal nodules along the nasal septum or inferior turbinates. Nasal mucosal biopsy may yield the characteristic histopathologic findings of sarcoidosis but can sometimes be difficult to isolate in Wegener granulomatosis.
Differential Diagnosis
From Clinical Data
A mass that appears to be necrotizing will lead to a consideration of these diseases. A history of cocaine use is obviously helpful but often not forthcoming until the pattern and extent of disease is firmly established. Due to the relative nonspecific findings characteristic of many of these diseases, patients with significant intranasal and/or findings on imaging that do not respond to typical medical therapy for acute and chronic sinusitis must be suspected of an atypical diagnosis. Wegener granulomatosis, sarcoidosis, Langerhans cell histiocytosis, and Churg-Strauss syndrome, as well as other infectious causes of sinonasal disease such as fungal sinusitis, must be entertained in this scenario.3 Intranasal neoplastic processes are also a consideration and can be ruled out by careful endoscopic-assisted biopsy. The presence of concurrent systemic disorders may guide the clinician in narrowing the differential diagnosis. In immune-compromised patients, nasal septal problems may be due to acute bacterial infection (Fig. 87.2).
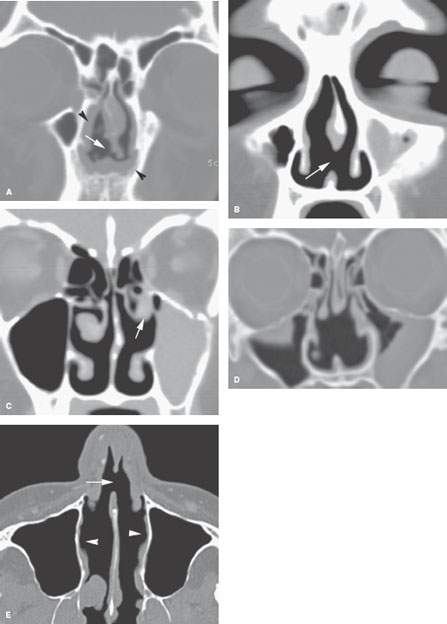
FIGURE 87.1. Four patients with documented cocaine abuse. A: Patient 1 showing generalized mucosal thickening in the anterior nasal cavity (arrowheads) with a far anterior and inferior septal perforation (arrow). B, C: Patient 2 with an anterior inferior septal perforation (arrow) in (B). In (C), the middle turbinate has become scarred due to chronic nasal granulomatous changes and adherent to the lateral wall of the nasal cavity (arrow). The maxillary sinus is completely opacified due to the adhesive changes around its ostium (not shown). D: Patient 3 showing that sometimes the nasal perforation in cocaine abuse extends more posteriorly and can be extensive; this mimics the appearance of Wegener granulomatosis more than the other three patients in this figure. E: Patient 4 with an anterior inferior nasal septal perforation (arrow) and generally atrophic changes throughout the nasal cavity (arrowheads) consistent with the necrosis and atrophic rhinitis caused by chronic cocaine abuse.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








