Circumscribed Astrocytic Tumors
Overview
Circumscribed astrocytic tumors of the central nervous system are characterized by well-delineated margin on pathology and imaging and usually lack infiltrative changes in the neighboring brain.
|
Pilocytic Astrocytoma
Definition: Pilocytic astrocytoma is a well-circumscribed astrocytic neoplasm composed of variable proportions of compacted bipolar cells with Rosenthal fibers and loose, textured multipolar cells with microcysts and eosinophilic granular bodies. The supratentorial pilocytic astrocytomas are genetically characterized tandem duplications of chromosome 7q34 involving the BRAF gene resulting in oncogenic BRAF fusion proteins.
Epidemiology: Pilocytic astrocytomas account for up to 6% of all gliomas, and they are the most common primary brain tumors during the first two decades of life, especially in children. They account for almost 33% of all brain tumors in the 0- to 14-year age group.
Affected age group: This tumor primarily affects children ages 0 to 14 years, with a mean age of 7 years, and young adults, with a mean age of 22 years, but can occasionally occur in older patients in the fifth to seventh decades.
Molecular and genetic profile: Molecular and genetic alterations in pilocytic astrocytomas depend on the location of tumor. The most common genetic abnormality is in duplication of 7q34, encompassing the BRAF gene. Mutation hotspots result in valine to glutamate substitution at position 600, often referred to as BRAF V600E mutation. It remains unclear if this mutation has any prognostic significance.
Pilocytic astrocytoma is strongly associated with neurofibromatosis 1 (NF1), where up to 15% of individuals develop pilocytic astrocytomas, particularly of the optic nerve pathway but also in other sites; the tumor can be multiple.
CSF markers: None.
Clinical features and standard therapy: Surgical resection is the mainstay of therapy to either resect or obtain tissue for definitive diagnosis. Currently, there is no standard chemotherapy regimen, and radiotherapy is considered to control symptoms or slow down the tumor growth.
Imaging
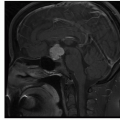
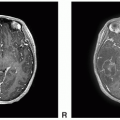
Pilocytic astrocytomas are circumscribed tumors with variable imaging features depending on the location, with more homogeneous enhancement of the hypothalamic and optic pathway tumor and an enhancing nodule and a cyst pattern in the posterior fossa tumor.
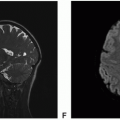
 Figure 13.1. (continued) G. diffusion-weighted imaging (DWI): Slightly increased diffusion within the solid tumor. |
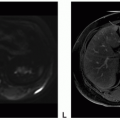
 Figure 13.2. (continued) E. Axial fluid-attenuated inversion recovery (FLAIR): Hyperintense to surrounding brain with minimal surrounding edema. F. Axial T2 FSE: Hyperintense to surrounding brain with minimal surrounding edema. G. Coronal T2 FSE: Hyperintense to surrounding brain. H. Axial DWI: Increased diffusion. I. Axial apparent diffusion coefficient (ADC): Increased diffusion. J. Axial CT unenhanced: Low-density mass without calcium.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|