(1)
Radiology – Neuroradiology Section, S. Paolo Hospital, Bari, Italy
1.1 Introduction
The spondyloarthritis (SpA) or spondylo-enthesoarthritis represent a group of seronegative inflammatory joint diseases that share many epidemiological, pathogenetic, clinical, and radiological aspects [1]. The term spondylo-enthesoarthritis emphasizes the three main aspects of these diseases, such as the involvement of the spine, the entheses, and peripheral joints.
This group encompasses the following diseases:
Ankylosing spondylitis (AS) primitive
Psoriatic arthritis (PsA)
Reactive arthritis (ReA)
SpA associated with inflammatory bowel disease (enteropathic arthritis, EA)
Undifferentiated SpA (U-SpA)
The prevalence of SpA varies, depending on the populations studied, from 0.2 to 1.9 %. In Italy has been reported the prevalence of approximately 1 % for Spa, among which the PsA is the most frequent (0, 42%) [2].
The disease starts between 20 and 40 years; earlier or later beginnings are not uncommon. Early diagnosis and therapy are essential to achieve adequate control in the inflammatory process, preventing structural damage and disability.
1.1.1 Etiopathogenesis
The histocompatibility antigen of class I HLA-B27 is closely related to the susceptibility to SpA and, in particular, to its axial location; however, the prevalence of this marker varies in relation to the type of disease (90–95 % in AS patients, up to 40 % in patients with PsA) and to the ethnicity of the patient.
Bacterial infections have long been recognized as a possible etiological factor of many SpA as some bacteria (Chlamydiae and some other bacteria) have the ability of triggering ReA.
1.1.2 Clinical Aspects
The primary site of the inflammatory process of SpA is the entheses, the point of bony insertion of ligaments, tendons, and other fibrocartilagineous components of the musculoskeletal system [3]. Such involvement is responsible for most of the clinical manifestations of SpA, both axial and peripheral devices, such as sacroiliitis, spondylitis, enthesitis, and arthritis [4].
Extra-articular manifestations also characterize this group of diseases such as involvement of eye (anterior uveitis, conjunctivitis), of the skin (psoriasis, keratoderma pseudoblenorragicum, balanitis circinata), of cardiovascular system (aortic insufficiency, disorders of atrioventricular), and of intestine (chronic colitis).
There are no “diagnostic” laboratory tests for SpA. They are usually called “seronegative” as the tests for rheumatoid factor are negative. The acute phase reactants (APR) increase in approximately 60 % of cases. The presence or absence of the HLA-B27, singly taken, is not sufficient to confirm or rule out a diagnosis.
1.1.3 Imaging
Although the diagnosis of SpA is primarily based on clinical manifestations, imaging modalities are essential to confirm the suspected diagnosis, to define the extension of the disease, and to monitor its evolution.
Conventional radiology is usually late in detecting abnormalities. Early signs of entheseal involvement can be revealed by ultrasonography combined with power Doppler or, better, by magnetic resonance imaging (MRI).
MRI studies of the sacroiliac joints and the spine in patients with SpA have made a major contribution in the last decade to a better understanding of the course of the disease, to an early diagnosis, and have been used as an objective outcome measure for clinal trails.
1.1.4 Classification
In 1991, the European Spondyloarthropathy Study Group (ESSG) proposed the classification criteria [5]. These criteria with high specificity and sensitivity proved unable to classify oligosymptomatic patients (peripheral arthritis, dactylitis, enthesitis, isolated inflammatory back pain, or acute anterior uveitis).
The coeval Amor criteria behave better than ESSG, as they are able to classify as undifferentiated SpA even diseases without one of the two major ESSG criteria [6]. Nevertheless, even Amor criteria are unable to classify patients as monosymptomatic (no single criterion reaches the minimum score of 6).
The SpA may be clinically divided in forms with predominant involvement of peripheral or axial joints, with varying degrees of overlap between the two sub-types (ASAS criteria) [3, 4]. The advantage of this classification is in a better representation of the disease at an early stage and in improving the therapeutic strategies according to the prevalent form, axial or peripheral.
The introduction of new imaging techniques, particularly MRI, and the possibility of new and more effective treatments has renewed interest in the classification of SpA group ASAS (Assessment of Spondyloarthritis International Society) that has recently developed and validated new criteria for the axial forms (spondylitis, sacroiliitis) (Fig. 1.1) and for the peripheral forms (arthritis, enthesitis, dactylitis) [7, 8].
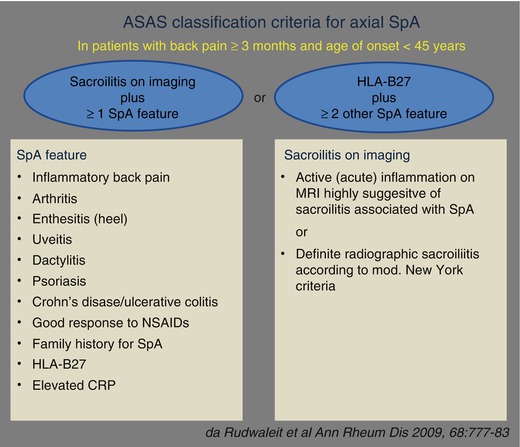
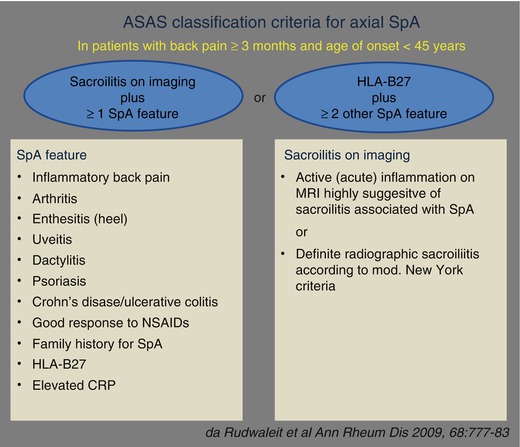
Fig. 1.1
ASAS classification criteria for the axial and peripheral forms
The ASAS criteria work better than the previous criteria in classifying the different forms of SpA although specificity and sensitivity of peripheral SpA criteria appear not completely satisfying.
1.1.5 Therapy
The treatment of SpA is based, in general, on the association of non-steroidal anti-inflammatory drugs (NSAID) with drugs called disease modifying anti-rheumatic drugs (DMARDs), such as sulfasalazine and methotrexate. In the last decade, the treatment of SpA has improved dramatically with the introduction of biologics directed against TNF-a. Tumor necrosis factor α blockers (A-TNF α), infliximab, adalimumab, etanercept, and golimumab, very effective on the symptoms and signs of SpA, have been shown to halt or delay the progression of radiological damage [9–11].
1.2 Ankylosing Spondylitis
Ankylosing spondylitis (SA), the most typical form of SpA, is a chronic inflammatory disease of unknown etiology that predominantly affects the axial skeleton (sacroiliac joints and spine) but may also involve peripheral joints and entheses [12].
The primitive (or idiopathic) spondylitis occurs independently of any other condition, and should be distinguished from secondary spondylitides that may appear during cutaneous psoriasis, reactive arthritis, or inflammatory bowel disease.
The prevalence of SA varies, depending on ethnicity and classification criteria used, between 0.2 and 1.8 %. In Italy, a recent study in the Marche region showed a prevalence of 0.37 % [2].
The disease usually begins in people between the ages of 20 and 40 years; less than 5 % of cases has an onset after the age of 45. The F:M ratio is 1:3. Usually the clinical expression of SA is more severe in males.
1.2.1 Clinical Aspects
The typical presenting symptom is inflammatory back and/or buttock pain (IBP), sometimes involving the back of thighs (so-called atypical sciatica) [13].
The involvement of the costovertebral joints, manubriosternal, condrosternal joints and the entheses at respiratory muscle insertions can cause chest pain that is accentuated by coughing or sneezing.
The involvement of the entire spine with its progressive stiffening is responsible for a significant functional limitation and typical postural abnormalities (hyperlordosis of the cervical spine, dorsal kyphosis, flattening of the lumbar lordosis). The involvement of the thorax skeleton results in a reduced ventilatory capacity compensated by the increase in diaphragmatic breathing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree