Clinical Cases: Malignant Lesions
7.1 Case 1: Ductal Carcinoma in Situ
7.1.1 Clinical Presentation
A 67-year-old woman with a history of invasive ductal carcinoma of her right breast presents for yearly routine mammography. The patient is 5 years from lumpectomy, chemotherapy, and radiation therapy. New suspicious calcifications without a mass were identified in her left breast on mammogram. The mammogram was classified as Breast Imaging–Reporting and Data System (BI-RADS) category 4C. The breast was small in size, and a stereotactic biopsy was felt to be difficult to perform. Ultrasound was recommended for further evaluation and to determine if ultrasound-guided biopsy of the calcifications could be performed.
7.1.2 Ultrasound Findings
On B-mode imaging (▶ Fig. 7.1a) an 8 mm isoechoic, ill-defined mass is associated with the microcalcifications. On color Doppler (▶ Fig. 7.1b) there is moderate blood flow associated with the mass. The lesion was classified as BI-RADS category 4B on ultrasound
On strain elastography (SE) (▶ Fig. 7.1c) the mass is stiffer than surrounding glandular tissue and has an elastogram/B-mode (E/B) ratio of 1.2 (▶ Fig. 7.1d). The lesion has a score of 5 on the 5-point color scale. The strain ratio (lesion to fat ratio) is 6.1 (▶ Fig. 7.1e). On shear wave elastography (SWE) (▶ Fig. 7.1f) the lesion has a maximum shear wave velocity (Vs) of 4.22 m/s (54 kPa). The adjacent normal breast tissue has a Vs of 2 m/s (12 kPa).
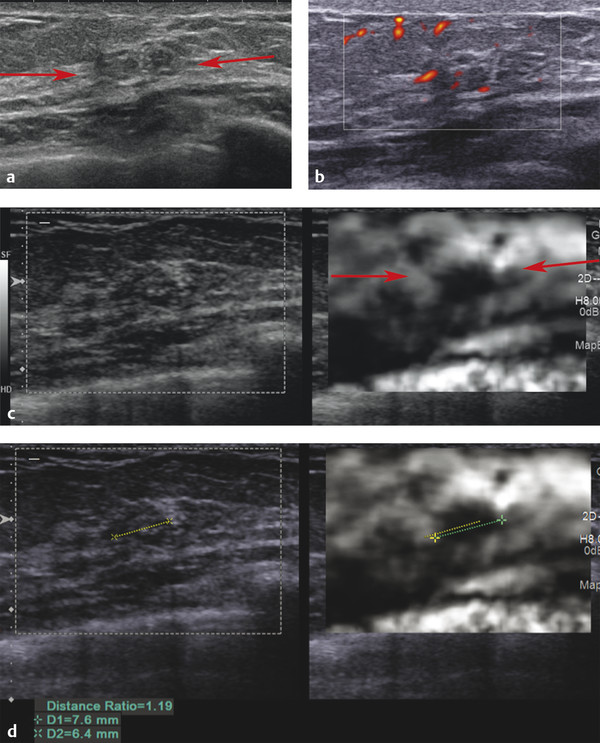
Fig. 7.1 (a) In the area of the suspicious calcifications on mammography there is an 8 mm vague hypoechoic lesion (arrows) with some associated calcifications. (b) On power Doppler imaging there is generalized increased blood flow in the area with some blood flow within the lesion. (c) On strain elastography the lesion (arrows) is stiffer than adjacent tissue with an E/B ratio of 1.2. This lesion has a score of 5 on the 5-point color scale. (d) The lesion measures 6.4mm on B-mode (yellow line) and 7.6mm on SE (green line) with an E/B ratio of 1.2. (continued)
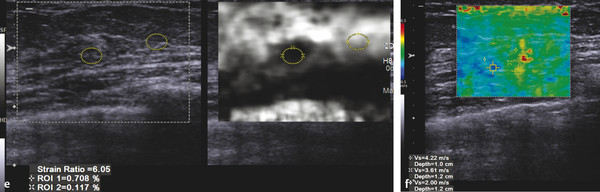
Fig. 7.1 (continued) (e) The lesion has a strain ratio (lesion to fat ratio) of 6.1 on strain imaging, suggestive of a malignant lesion. (f) On shear wave imaging the lesion has a maximum Vs of 4.2 m/s (52 kPa), which is close to the cutoff value for a malignant lesion.
7.1.3 Diagnosis
Ductal carcinoma in situ. The patient underwent an ultrasound-guided vacuum-assisted core biopsy of the mass. The pathology was ductal carcinoma in situ. The patient had a lumpectomy with a histology of ductal carcinoma in situ; intermediate grade Estrogen Receptor (ES) (+) 75% Progesterone Receptor (PR) (−). No evidence of invasive cancer was identified.
7.1.4 Discussion
Ductal carcinoma in situ (DCIS) is the most common type of noninvasive breast cancer. Ductal carcinoma refers to the development of cancer cells within the milk ducts of the breast. The cells are confined to the duct and have not extended to any surrounding tissue. DCIS is noninvasive breast cancer that encompasses a wide spectrum of diseases ranging from low-grade lesions that are not life threatening to high-grade lesions that may harbor foci of invasive breast cancer. DCIS is classified according to architectural pattern (solid, cribriform, papillary, and micropapillary), tumor grade (high, intermediate, and low grade), and the presence or absence of comedo histology.
DCIS rarely produces symptoms or a palpable mass and is mostly found on screening mammography.119 DCIS has become one of the most commonly diagnosed breast conditions, now accounting for 20% of breast cancers and precancers that are detected through screening mammography.120 DCIS is usually identified on mammography as microcalcifications.
Surgical excision removing all of the abnormal duct elements is a common treatment. Radiation after surgery further reduces the risk that the DCIS will recur. Biomarkers can identify which women diagnosed with DCIS are at high or low risk of subsequent invasive cancer.121,122 Hormonal therapy is recommended for some women with estrogen-receptor-positive DCIS to help prevent invasive breast cancer.
Unless treated, approximately 60% of low-grade DCIS lesions will become invasive at 40 years follow-up.123 High-grade DCIS lesions that have been inadequately resected and not given radiotherapy have a 50% risk of becoming invasive breast cancer in 7 years. Approximately half of low-grade DCIS detected at screening will represent overdiagnosis, but overdiagnosis of high-grade DCIS is rare.123
Although DCIS is detected through microcalcifications at mammography, those without calcifications cannot be detected by mammography, and 6 to 23% of cases of DCIS are felt to remain undetected.124–126 Izumori et al127 examined 150 cases with DCIS using ultrasound and retrospectively classified them into a cystic or solid mass, ill-defined hypoechoic mass, microlobulated mass, duct dilatation, and calcification. Among these, in 37 (79%) of 47 cases with ultrasound findings alone, a cystic or solid mass was observed. Most were ovoid in shape, and the margins were circumscribed or microlobulated, making it difficult to differentiate from benign lesions. Moreover, approximately half of these cases had heterogeneous internal echoes.
Based on the proposed elastography classification system (similar to the BI-RADS classification) presented in Chapter ▶ 5 the lesion would have a > 95% probability of malignancy. (> 95% on SE; 2–95% on SWE).
7.2 Case 2: Ductal Carcinoma in Situ—Fibroadenoma with Foci of DCIS
7.2.1 Clinical Presentation
A 43-year-old woman presents with a new mass containing suspicious calcifications on screening mammogram. The lesion was classified as BI-RADS category 0, and an ultrasound was requested for further workup.
7.2.2 Ultrasound Findings
On B-mode (▶ Fig. 7.2a) the mass noted on mammography is a lobular well circumscribed mass with several echogenic foci within the mass representing the calcifications noted on mammography. The lesion has significant blood flow on power Doppler (▶ Fig. 7.2b). The lesion was classified as BI-RADS category 3.
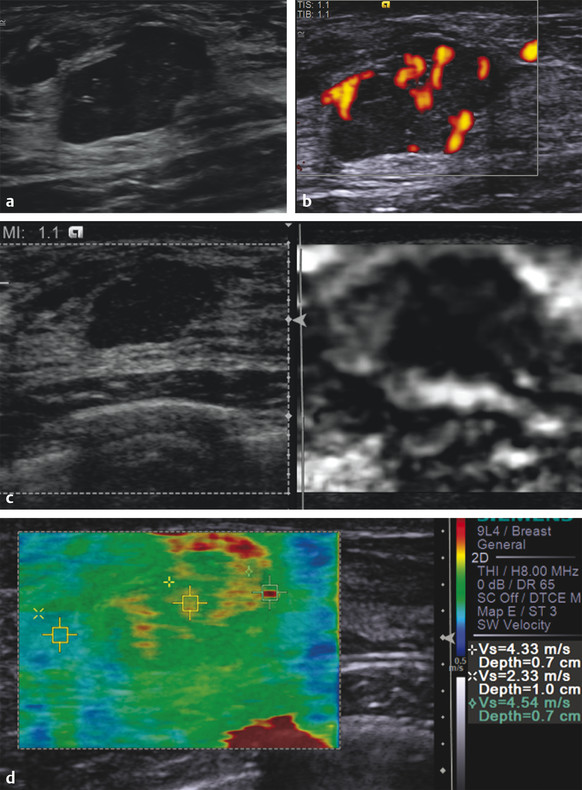
Fig. 7.2 (a) The palpable mass is a lobular 1.6 cm well defined lobular lesion with some punctate areas of hyperechogenicity suggestive of microcalcifications. (b) The lesion has marked increased blood flow on power Doppler imaging. (c) On strain imaging the lesion is stiffer than surrounding tissue and has an E/B ratio of 1.2, suggestive of a malignant lesion. This lesion has a score of 5 on the 5-point color scale. The strain ratio (lesion to fat ratio) was not calculated in this case. (d) On shear wave imaging the lesion has a Vs of 4.5 m/s, suggestive of a malignancy. The shear wave imaging color coding demonstrates the lesion has components of varying stiffness (3.5–4.5 m/s; 38–60 kPa)
On strain imaging (▶ Fig. 7.2c) the lesion is stiffer than the surrounding glandular tissue. The mass is larger on SE than on B-mode imaging with an E/B ratio of 1.2. The lesion has a score of 2 on the 5-point color scale. On shear wave imaging (▶ Fig. 7.2d) the elasticity of the lesion is heterogeneous with scattered foci of a high Vs up to 4.5 m/s (60 kPa). The background Vs of the lesion is 2.8 m/s (24 kPa). The background breast tissue has a Vs of 2.3 m/s (17 kPa).
7.2.3 Diagnosis
Fibroadenoma with foci of DCIS. The lesion was biopsied using a 12-gauge vacuum-assisted core needle under ultrasound guidance. The areas of increased Vs were targeted on the biopsy. The pathology demonstrated a fibroadenoma with foci of DCIS. The patient underwent a lumpectomy with the pathology an intermediate-grade DCIS, multifocal, cribriform, and solid patterns, arising in fibroadenoma.
7.2.4 Discussion
Fibroadenoma may be associated with fibrocystic changes, proliferative epithelial changes, and, extremely rarely, with noninvasive and invasive cancer. The incidence of carcinoma within fibroadenoma is reported between 0.1 and 0.3% in a screened population, with a peak age of occurrence between 42 and 44 years.128–131 The biological behavior of carcinoma occurring within fibroadenoma does not differ from that of breast carcinoma not related to fibroadenoma.130–132 Preoperative clinical criteria and radiological criteria are usually insufficient to suggest that malignant change has occurred in a fibroadenoma, especially in cases with DCIS.133
In this case the stiffness within the lesion is heterogeneous, ranging from 2.3 m/s (17 kPa) to 4.5 m/s (60 kPa). On pathology the lesion was a benign fibroadenoma with scattered foci of DCIS. Although direct comparison of the imaging to pathology was not performed, the areas of increased stiffness most likely represent the areas of DCIS. It is important to use the elastographic finding to guide an image-guided core biopsy. Although no studies have been performed, targeting the areas with the highest stiffness values could allow for more accurate pathological correlation of core biopsies with surgical specimens.
The maximum Vs in this case was 4.5 m/s (60 kPa), which is a borderline value for the cutoff value for benign and malignant. On SE the E/B ratio was 1.2. The maximum stiffness value and the E/B ratio have been suggested to correlate with the tumor grade. The higher the Vs or E/B ratio the greater the probability of a higher-grade tumor.28 Low-grade lesions such as DCIS or mucinous carcinoma can have an E/B ratio of 1; therefore, we always biopsy lesions with an E/B ratio of 1 or greater.
Based on the proposed elastography classification system (similar to the BI-RADS classification) presented in Chapter ▶ 5 this lesion would have a probability of > 95% of malignancy.
7.3 Case 3: Invasive Ductal Carcinoma—Borders Ill Defined, Grade 1
7.3.1 Clinical Presentation
A 47-year-old woman with a recent negative mammogram but a density 4 breast presents with a BI-RADS category 4C lesion on a screening automated whole breast ultrasound. The mammogram was classified as BI-RADS category 2, the automated whole breast ultrasound was classified as BI-RADS category 0, and a handheld ultrasound was advised for further workup.
7.3.2 Ultrasound Findings
A selected image (▶ Fig. 7.3a) from an automated whole breast ultrasound demonstrates a 1.5 cm irregular, hypoechoic mass. On handheld B-mode ultrasound (▶ Fig. 7.3b) the lesion is again noted with irregular borders, marked hypoechogenicity, and shadowing. On color Doppler imaging (▶ Fig. 7.3c) the lesion has significant blood flow. The lesion was classified as BI-RADS category 5.
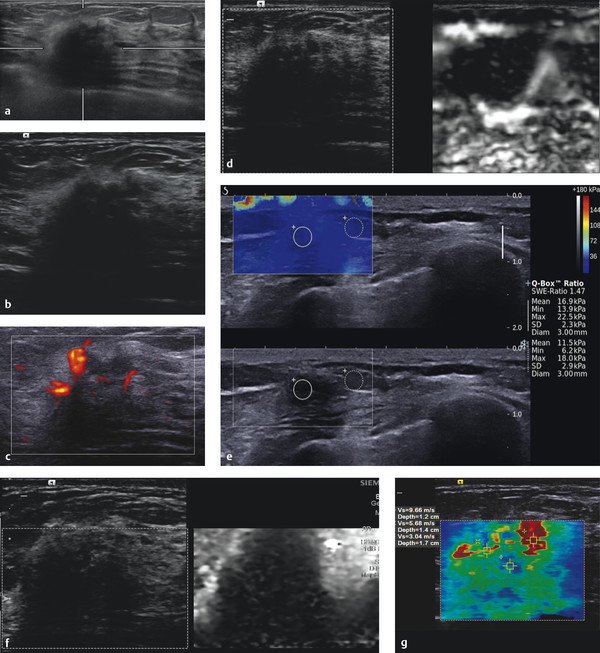
Fig. 7.3 (a) Selected image from an automated whole breast ultrasound demonstrating a 1.5 cm irregular mass with a hyperechoic rim. (b) Handheld ultrasound of the lesion in (a) confirms the presence of a 1.5 cm irregular hypoechoic mass with a hyperechoic rim and shadowing (Harmonic imaging used). (c) There is moderate blood flow adjacent to the lesion on power Doppler imaging. (d) On strain elastography the lymph node is stiffer than surrounding tissue and has an E/B ratio of 1.1 suggestive of a malignancy. (e) On shear wave imaging the lesion has a Vs of > 7.7 m/s (> 180 kPa), highly suggestive of a malignancy. (f) The quality map confirms adequate shear waves are generated for an accurate Vs measurement to use for interpretation. (g) On shear wave elastography the lesion has heterogeneous stiffness with a maximum Vs of 9.7 m/s, suggestive of a malignant lesion.
On SE (▶ Fig. 7.3d) the lesion is much stiffer than the surrounding breast tissue. It is difficult to calculate an accurate E/B ratio because the borders of the lesion are not defined on B-mode. The lesion has a lesion to fat ratio of 10.5 (▶ Fig. 7.3e). On Virtual Touch imaging (VTi, Siemens Ultrasound, Mountain View, CA) the lesion is much stiffer than the surrounding breast tissue. The lesion appears of similar size to the B-mode image. On shear wave imaging (▶ Fig. 7.3f) the lesion has a max Vs of 9.7 m/s (> 180 kPa).
7.3.3 Diagnosis
Invasive ductal carcinoma, grade 1. The lesion was biopsied under ultrasound guidance using a 12-gauge vacuum-assisted core needle. The pathology was an invasive ductal carcinoma, well differentiated, grade 1. The patient had a lumpectomy where the maximum size of the tumor on surgical resection was 2.5 cm. The patient was node negative.
7.3.4 Discussion
The morphology of breast cancer is heterogeneous because breast cancer is not one disease. The histopathological features of a breast cancer are needed for appropriate management. Breast cancer can be classified into types including lobular, tubular, medullary, mucinous, and no special type (NST).123 Tumor staging is the most useful means for predicting survival. The TNM staging system is the mainstay for prognostication of breast cancer. Histologic grading is usually performed using the Scarff, Bloom, and Richardson (SBR) system. This system is a composite of degrees of glandular formation, nuclear pleomorphism, and mitotic activity. Each of these parameters is assigned a numerical score from 1 to 3 based on specific criteria. Scores from each category are then summed; a score of 3 to 5 is equivalent to grade 1, a score of 6 or 7 is equivalent to grade 2, and a score of 8 or 9 is equivalent to grade 3.
This patient had a screening mammogram interpreted as BI-RADS category 2 with breast density 4. The patient had an automated whole breast screening ultrasound that detected a 1.5 cm irregular spiculated hypoechoic mass (▶ Fig. 7.3a). The examination was classified as a BI-RADS 0, and a whole breast ultrasound was requested. At this time a standard of interpretation of automated whole breast scanning has not been implemented. At our institution, automated whole breast scans are interpreted similar to screening mammography where an abnormality is read as a BI-RADS 0, and a handheld ultrasound is requested for further workup. At the handheld examination the lesion can be better evaluated with transducer position changes, color or power Doppler, and elastography. A BI-RADS category score of 2 to 5 can then be issued and appropriate follow-up then advised.
In this case the handheld ultrasound confirmed the presence of a 1.5 cm irregular, hypoechoic mass (▶ Fig. 7.3b) with significant blood flow (▶ Fig. 7.3c). The SE images confirm that the lesion is much stiffer than adjacent breast tissue (▶ Fig. 7.3d) with a strain ratio of 10.5 (▶ Fig. 7.3e). An accurate E/B ratio cannot be determined because the lesion borders are difficult to assess on B-mode. Note that the posterior margin of the mass is well defined in the elastogram compared with the B-mode image where there is significant shadowing. On VTi (strain imaging with acoustic radiation force impulse [ARFI]) the lesion is stiffer than surrounding tissue and appears to have an E/B ratio of approximately 1. Note that the surrounding glandular tissue is white (▶ Fig. 7.3f, arrows). Therefore the dynamic range of stiffness values set by the machine is quite large with the malignancy being very stiff, setting the upper portion of the scale. Therefore the glandular tissue is relatively “whiter” than if a malignancy were not present. Because of this scaling process SE images with a cancer often appear black and white with very few gray coding areas.
The lesion has a very high Vs of 9.7 m/s on shear wave imaging (▶ Fig. 7.3g). In this case the blue portion of the tumor had poor-quality shear waves in this area on the quality map. However, the area with high Vs had good-quality shear waves. Because of the poor shear wave generation in many breast malignancies the central portion of the tumor is either not color coded or has a poor-quality map in this region. However ,the peripheral portions of the tumor will have a high Vs, thus often giving the appearance of a “ring” of high Vs surrounding the lesion.
Based on the proposed elastography classification system (similar to the BI-RADS classification) presented in Chapter ▶ 5 we would consider this lesion to have a > 95% probability of malignancy.
7.4 Case 4: Invasive Ductal Carcinoma—Grade 2
7.4.1 Clinical Presentation
An 82-year-old woman with bilateral palpable breast masses presented for a diagnostic mammogram. A 1 cm new mass was identified in the retroaureolar region of the left breast. The lesion was classified as BI-RADS category 0 and ultrasound recommended for further evaluation.
7.4.2 Ultrasound Findings
On B-mode ultrasound (▶ Fig. 7.4a) a 1.5 cm irregular, hypoechoic, heterogeneous mass is identified. On color Doppler imaging (▶ Fig. 7.4b) there is some peripheral blood flow. The lesion was classified as BI-RADS category 4C.
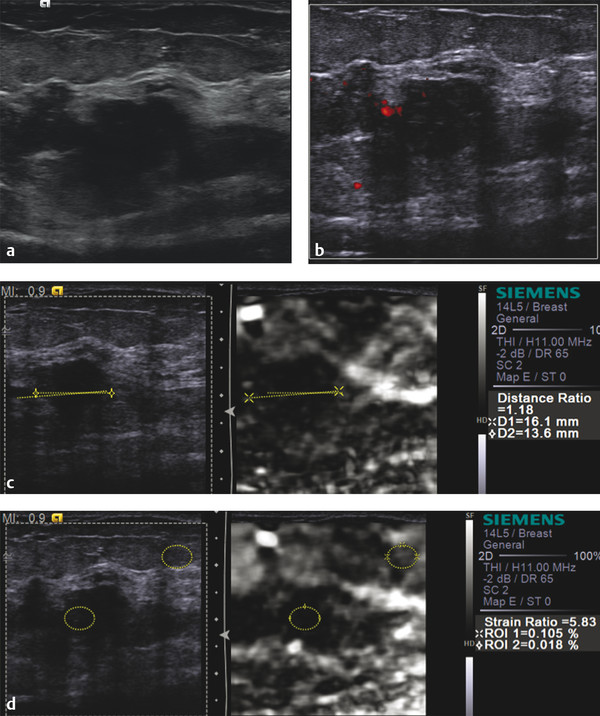
Fig. 7.4 (a) B-mode image demonstrates an irregular hypoechoic mass with a question of some internal punctate calcifications. (b) There is a small amount of blood flow adjacent to the lesion on power Doppler imaging. (c) On strain elastography (SE) imaging the lesion is stiffer than adjacent tissue. The lesion measures 13.6mm (yellow line) and 16.1mm (green line) with an E/B ratio of 1.2 and a score of 5 on the 5-point color scale, both suggestive of a malignant lesion. (d) The strain ratio (lesion to fat ratio) on SE is 5.8, also suggestive of a malignant lesion. (continued)
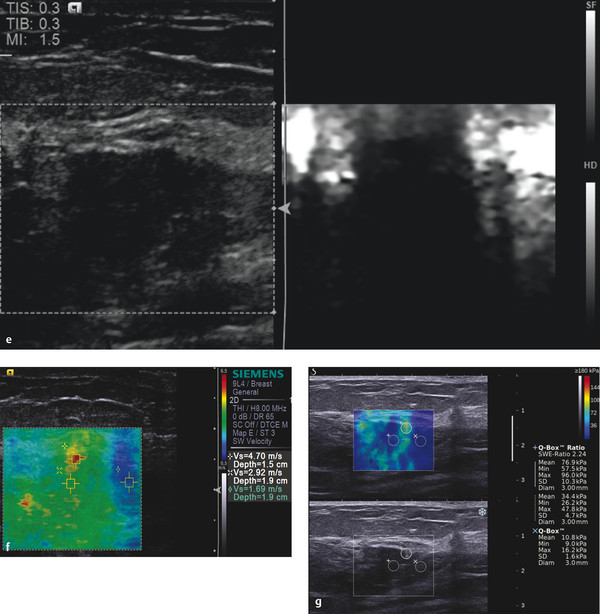
Fig. 7.4 (continued) (e) On Virtual Touch imaging (VTi, Siemens) (strain imaging using acoustic radiation force impulse [ARFI]) the lesion is very stiff with a similar appearance to SE using the manual displacement technique (c). (f) On shear wave elastography (SWE) the stiffness of the lesion is heterogeneous with the maximum Vs of 4.7 m/s (68 kPa), suggestive of a malignancy. (g) SWE obtained on a different system demonstrates the central portion of the lesion to have a lower Vs, but there is a ring of high Vs in the periphery of the lesion, also suggestive of a malignancy.
On strain imaging (▶ Fig. 7.4c) the lesion is stiffer than surrounding breast tissue and has an E/B ratio of 1.2. The lesion has a lesion to fat ratio of 5.8 (▶ Fig. 7.4d). On the 5-point color scale this lesion would be given a score of 5. Similar finding are identified on VTi (▶ Fig. 7.4e). On shear wave imaging (▶ Fig. 7.4f) the lesion has a max Vs of 4.7 m/s (68 kPa). On shear wave imaging on a different system (▶ Fig. 7.4g) the lesion has a max Vs of 5.7 m/s (96 kPa).
7.4.3 Diagnosis
Invasive ductal carcinoma, grade 2. The lesion was biopsied using a 12-gauge vacuum-assisted core needle under ultrasound guidance. The pathology was an Invasive Moderately Differentiated Ductal Cancer, grade 2 with mucinous features with associated low grade Ductal Carcinoma-in-situ.
7.4.4 Discussion
This case has concordant findings on SE and SWE. The lesion is stiffer than surrounding breast tissue on SE with an E/I ratio of 1.2, a strain ratio (lesion to fat ratio) of 5.8, a score of 5 on the 5-point color scale. Similar finding are found with VTi (strain imaging with ARFI). Both shear wave systems demonstrate a Vs of >4.5 m/s (>60 kPa) suggestive of a malignancy. As is a common feature of shear wave elastography the central portion of the malignancy is color-coded softer than the periphery. On the quality map this area has poor quality shear wave. However the ring of higher Vs surrounding the lesion is the major finding to suggest this is a malignancy. The ring may be due to neoplastic tissue that allows for good shear wave generation or may be due to reflections from the soft to hard interface between the malignancy and adjacent sort tissue (RG Barr, personal communication 1 October 2013). Further studies are needed to clarify the exact cause of the ring.
This case was classified as a BI-RADS 4C on conventional ultrasound and merits biopsy based on those findings. The addition of elastography is helpful to determine the stiffest portion of the mass to guide biopsy. Although not yet proven it is expected that better correlation with pathology finds will occur when elastography is used to guide biopsies.
Based on the proposed elastography classification system (similar to the BI-RADS classification) presented in Chapter ▶ 5 this lesion would have a > 95% probability of malignancy.
7.5 Case 5: Invasive Ductal Carcinoma—Grade 1
7.5.1 Clinical Presentation
A 50-year-old woman with bilateral breast implants was found to have a new mass in her left breast on screening mammography. The lesion was classified as BI-RADS category 0, and an ultrasound was recommended for further evaluation.
7.5.2 Ultrasound Findings
On B-mode imaging (▶ Fig. 7.5a) a 1.7 cm lobular, wider than taller, hypoechoic mass is identified. On color Doppler imaging (▶ Fig. 7.5b) there is marked blood flow within the lesion. The lesion was classified as BI-RADS category 4A.
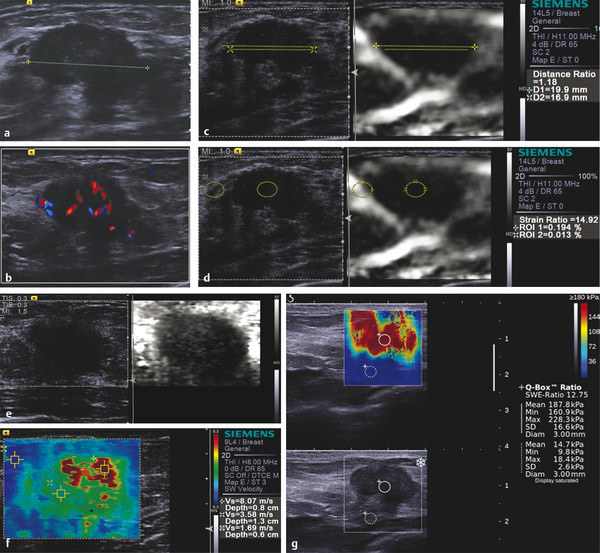
Fig. 7.5 (a) On B-mode imaging the lesion has a lobular border with the posterior portion of the lesion not well defined. (b) On color Doppler imaging the lesion (green line) has a moderate amount of internal blood flow. (c) On strain elastography the lesion is stiffer than adjacent tissue. The lesion measures 16.9mm (yellow line) on B-mode image and 19.9mm (green line) on SE with an E/B ratio of 1.2. The lesion has a score of 5 on the 5-point color scale, both suggestive of a malignant lesion. (d) The strain ratio (lesion to fat ratio) is 14.9, suggestive of a malignant lesion. (e) On Virtual Touch imaging (VTi, Siemens) the lesion is stiffer than the adjacent breast tissue and has an E/B ratio of 1.2, suggestive of a malignant lesion. (f) On shear wave elastography (SWE) the lesion has a Vs of 8.1 m/s (> 180 kPa), highly suggestive of a malignant lesion. (g) SWE on a different shear wave system has similar findings, with a Vs of 7.8 m/s (188 kPa).
On SE (▶ Fig. 7.5c) the lesion is stiffer than the surrounding breast tissue and has an E/B ratio of 1.2. The lesion to fat ratio was 14.9 (▶ Fig. 7.5d). Similar findings are identified on VTi (▶ Fig. 7.5e). On shear wave imaging (▶ Fig. 7.5f) the max Vs is 8.1 m/s (> 180 kPa). On a different shear wave system (▶ Fig. 7.5g) the lesion has a uniformly high Vs with a max Vs of > 9 m/s (228 kPa).
7.5.3 Diagnosis
Invasive ductal carcinoma, grade 1. The lesion was biopsied with a 12-gauge vacuum-assisted core needle under ultrasound guidance. The pathology was an invasive ductal carcinoma, grade 1.
7.5.4 Discussion
There is an emerging molecular classification of breast cancer. Breast cancer is now considered as consisting of at least five different molecular subtypes, which are each characterized by distinct gene expression profiles.135–137 The patients with varying subtypes have different clinical outcomes, and each responds differently to treatment. Breast cancer subtypes defined by gene profile are listed in ▶ Table 7.1.135,138–142 Another emerging molecular subtype is Luminal C, which corresponds to the histopathological subtype of infiltrating lobular carcinoma. The molecular subtypes based on gene expression profiling dictate prognosis.
| Subtype | % of cancers | Distant disease-free survival | Overall survival | Gene profile |
| Luminal A | 51–61 | 75 | 90 | ER+, PR+, HER2- |
| Luminal B | 14–16 | 47 | 40 | ER+, and/or PR+, HER2+ |
| HER2 | 7–9 | 34 | 31 | ER-, PR-, HER2+ |
| Basal | 11–20 | 18 | 0 | ER-, PR-, HER2- Cytokeratin 5/6 and EGRF+ |
| Unclassified | 2–6 | NA | NA | – for all markers |
This case of an invasive ductal carcinoma has all of the positive features of elastography. On SE the lesion is stiffer than adjacent tissue and has an E/B ratio of 1.2, a strain ratio (lesion to fat ratio) of 14.9, a score of 5 on the 5-point color scale. The VTi (strain imaging with ARFI) are similar. The lesion has high Vs through the lesion with a good-quality map throughout the lesion. The Vs is 8 m/s (> 180 kPa). All findings are concordant and highly suspicious for a malignancy. Note is made that the E/B ratio is slightly above 1, but the stiffness based on the strain ratio (lesion to fat ratio) (SE) and the Vs (SWE) suggests a markedly stiff lesion. The correlation between the E/B ratio and the strain ratio has not been evaluated.
The lesion was a BI-RADS category 4A lesion on conventional ultrasound. The elastographic findings are significantly more suspicious.
Based on the proposed elastography classification system (similar to the BI-RADS classification) presented in Chapter ▶ 5 this lesion would have a > 95% probability of malignancy.
7.6 Case 6: Invasive Ductal Carcinoma—Grade 2
7.6.1 Clinical Presentation
An 82-year-old woman presents with a palpable mass. Mammography was not performed.
7.6.2 Ultrasound Findings
On B-mode ultrasound (▶ Fig. 7.6a) an irregular 3.5 cm hypoechoic mass is identified. On color Doppler imaging (▶ Fig. 7.6b) there is some peripheral blood flow. The lesion was classified as BI-RADS category 4C.
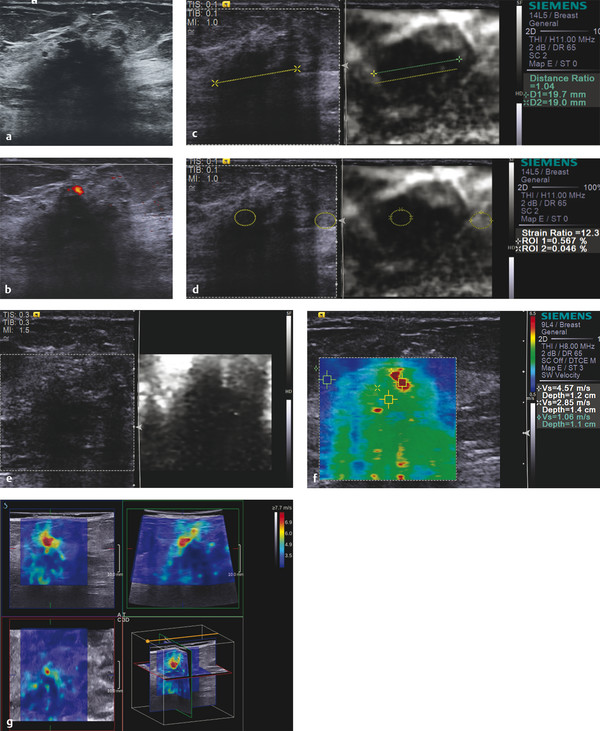
Fig. 7.6 (a) On B-mode imaging the lesion is an irregular hypoechoic lesion with some shadowing. (b) On color Doppler imaging there is a small amount of peripheral blood flow. (c) On strain elastography (SE) the lesion is stiffer than the adjacent breast tissue. The lesion measures 19.0mm (yellow line) on B-mode and 19.7mm (green line) on SE with an E/B ratio of 1 and a score of 4 on the 5-point color scale, both suggestive of a malignancy. (d) The strain ratio (lesion to fat ratio) is 12.3, highly suggestive of a malignant lesion. (e) On Virtual Touch imaging (VTi, Siemens) (strain imaging with acoustic radiation force impulse [ARFI]) the lesion is stiffer than the adjacent breast tissue and has an E/B ratio of 1.4. (f) On shear wave elastography (SWE) the lesion has heterogeneous increased stiffness with a maximum Vs of 4.6 m/s (65 kPa). (g) On three-dimensional (3D) SWE the lesion has an increased Vs surrounding the lesion, suggestive of a malignant lesion. The use of 3D SWE allows for complete evaluation of a lesion with one data acquisition (larger lesions may require more than one acquisition).
On strain imaging (▶ Fig. 7.6c) the lesion is stiffer than the surrounding breast tissue and has an E/B ratio of 1.04. The lesion to fat ratio is 12.3 (▶ Fig. 7.6d). Similar findings are found with VTi (▶ Fig. 7.6e). On shear wave imaging (▶ Fig. 7.6f) the max Vs is 4.6 m/s (65 kPa). On three-dimensional (3D) shear wave imaging (▶ Fig. 7.6g) there is increased Vs in the proximal portion of the lesion with a Vs of 7.7 m/s (180 kPa).
7.6.3 Diagnosis
Invasive ductal carcinoma, grade 3 with extensive tumor necrosis.
7.6.4 Discussion
On B-mode imaging the lesion borders are ill defined but are better identified on SE. Shadowing also interferes with the determination of the posterior border of the lesion. The posterior border of the lesion is well defined on SE. The strain elastographic findings of an E/B ratio of 1.04, strain ratio of 12.3, score of 5 on the 5-point color scale, and similar VTi (strain with ARFI) findings are all suggestive of a malignant lesion. The shear wave images are also suggestive of a malignancy with a Vs of > 4.5 m/s. The use of 3D elastography is helpful to evaluate the entire lesion to determine the site of the highest Vs. This case is one where the center of the cancer color codes blue, which is most likely an artifact of the algorithm. With improved algorithms this “blue” area will not be color coded, confirming that the shear waves in this region were of poor quality and should not be used in interpretation.
Based on the proposed elastography classification system (similar to the BI-RADS classification) presented in Chapter ▶ 5 this lesion would have a > 95% probability of malignancy.
7.7 Case 7: Invasive Ductal Carcinoma—SE and SWE Not Concordant, Grade 3
7.7.1 Clinical Presentation
A 59-year-old woman presents with a palpable mass near right axilla.
7.7.2 Ultrasound Findings
On B-mode imaging (▶ Fig. 7.7a) there is a 1 cm oval, hypoechoic lesion with ill-defined borders. On color Doppler imaging (▶ Fig. 7.7b) there is a small amount of blood flow in the lesion. The lesion was classified as BI-RADS category 4A.
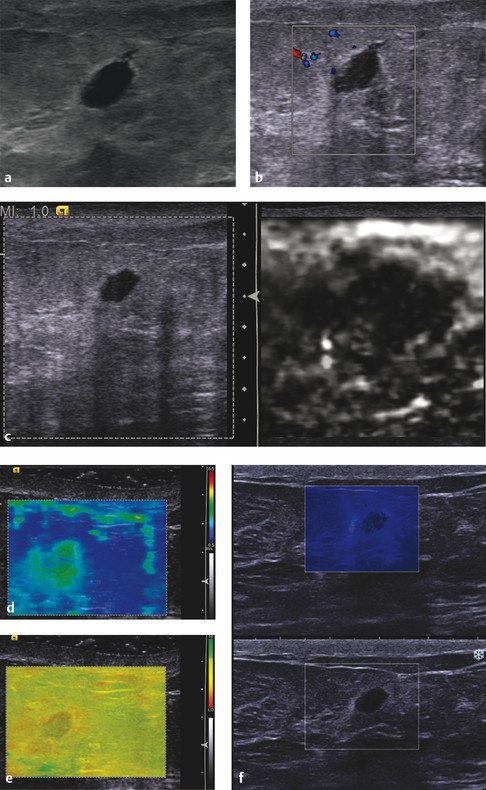
Fig. 7.7 (a) B-mode imaging demonstrates a 10 mm hypoechoic lesion with an indistinct border and the question of a small echogenic halo. (b) On color Doppler imaging the lesion has a small amount of internal blood flow. (c) On strain elastography the lesion is stiffer than the surrounding breast tissue, with an E/B ratio of 3.5 and a score of 5 on the 5-point color scale. (d) On shear wave elastography (SWE) the lesion has a Vs within the benign range. (e) The corresponding quality map of image (d) demonstrates that all of the shear waves are of poor quality and should not be used in interpretation. (f) SWE with another system also has a Vs within the benign range. With newer improved algorithms the lesion would not color code incorporating the quality map into one image.
On SE (▶ Fig. 7.7c) the lesion is stiffer than the surrounding fatty breast tissue and has an E/B ratio of 3.5. On shear wave imaging (▶ Fig. 7.7d) the lesion has a Vs of 2.5 m/s (19 kPa). On the quality map (▶ Fig. 7.7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree