Clinical Cases of Other Lesions
8.1 Case 1: Lymph Nodes—Benign Intramammary Lymph Node
8.1.1 Clinical Presentation
A 79-year-old woman presents with a 1 cm well circumscribed new mass in the right upper outer breast on mammography. The mammogram was classified as Breast Imaging–Reporting and Data System (BI-RADS) 0, and an ultrasound was advised for further workup.
8.1.2 Ultrasound Findings
On B-mode ultrasound (▶ Fig. 8.1a) a 10 mm oval well circumscribed hypoechoic lesion with a central area of increased echogenicity is identified. On color Doppler (▶ Fig. 8.1b) there is significant blood flow with some vessels appearing to enter the cortex and not at the hilum. The lesion was classified as BI-RADS category 4A.
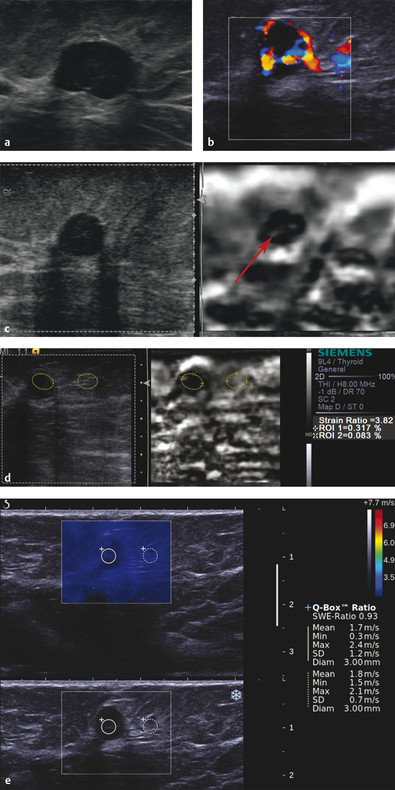
Fig. 8.1 (a) The mass identified on mammography is a well circumscribed, hypoechoic mass with a central area that is hyperechoic. (b) On color Doppler imaging there is significant blood flow in the lesion with a large feeding vessel and draining vein. (c) On strain elastography the mass has a soft central area with a thick rim that is stiffer than surrounding breast tissue. The lesion is smaller on elastography than in B-mode imaging. The lesion would be classified with a score of 2 or 3 in the 5-point color scale. (d) The strain ratio (lesion to fat ratio) is 3.8 on strain imaging, suggestive of a benign lesion. (e) On shear wave imaging the lesion has a Vs of 1.7 m/s (9 kPa), suggestive of a benign lesion.
On strain elastography (SE) (▶ Fig. 8.1c) the cortex of the lesion is stiffer than surrounding tissue and the central area is soft (white). The lesion is smaller on elastography. The strain ratio (lesion to fat ratio), using the cortex as lesion is 3.8 (▶ Fig. 8.1d). On shear wave elastography (SWE) (▶ Fig. 8.1e) the lesion has a Vs of 1.7 m/s (9 kPa).
8.1.3 Diagnosis
Benign intramammary lymph node. The lesion was biopsied with an 18-gauge core needle under ultrasound guidance. The pathology was a benign intramammary lymph node.
8.1.4 Discussion
Normal and abnormal axillary lymph nodes are commonly identified on mammography. Normal axillary lymph nodes are frequently identified and are typically small and oval with a lucent center due to hilar fat. Abnormal lymph nodes are characterized by high density, absence of hilar fat, and a round, irregular, ill-defined shape with or without intranodal calcifications on the Medial Lateral Oblique (MLO) view.169,170 The spectrum of calcifications within lymph nodes comprises microcalcifications, punctate or amorphous calcifications, and coarse calcifications.
Ultrasonography of the axillary region is an imaging method that can be used when an abnormal lymph node is detected on a negative mammogram. On ultrasound, a normal lymph node has a thin hypoechogenic cortex in the periphery and an echogenic hilum. Abnormal nodes tend to become more rounded. Eccentric enlargement with focal thickening of the cortex is a strong indicator of malignant transformation. Indentation of the hilum, and especially obliteration of the hilum, is highly suggestive of malignancy.171
Peripheral flow and transcapsular vessels seen on color Doppler favor malignancy compared with central flow in normal axillary lymph nodes. For an accurate diagnosis, needle aspiration or biopsy should be performed under ultrasound guidance. Enlargement of lymph nodes can be due to a variety of benign and malignant causes. The most common malignant cause of abnormal axillary lymph nodes is breast cancer; however, when lymph nodes enlarge because of metastatic breast cancer, the primary tumor within the breast is usually visualized mammographically. Occult breast cancer presenting as axillary metastasis is uncommon, accounting for less than 1% of all patients with primary breast cancer at diagnosis.172,173
In addition to metastatic breast cancer, another malignant cause of lymph node enlargement with a negative mammogram is metastases from other primary tumors (e.g., lymphoma, malignant melanoma, or lung or ovarian carcinomas). Benign causes of abnormal axillary lymph nodes include systemic inflammatory processes (sarcoidosis), infectious diseases (bacterial lymphadenitis, tuberculosis), collagen vascular diseases, and several miscellaneous causes (silicone implants, tattooing).
This lymph node has the elastographic features of a benign lymph node. The fatty hilum is soft, and the cortex of the lymph node is stiffer than surrounding tissue. The lymph node has an E/B ratio of < 1, and the strain ratio (lesion to fat ratio) of the cortex is usually less than 4. On SWE the lymph node usually has a Vs of < 3.2 m/s (30 kPa). The elastographic features of an abnormal lymph node include an E/B ratio of ≥ 1, a strain ratio of > 4.5, and a focal area of stiffness (stiffer than the normal lymph node cortex).
Based on the proposed elastography classification system (similar to the BI-RADS classification) presented in Chapter ▶ 5 the lesion has an ~ 0% probability of malignancy.
8.2 Case 2: Lymph Nodes—Benign Axillary Lymph Node
8.2.1 Clinical Presentation
An 84-year-old woman with a history of breast cancer with mastectomy now presents with a left axillary mass on physical exam. Mammography was not performed.
8.2.2 Ultrasound Findings
B-mode imaging (▶ Fig. 8.2a) shows a normal-appearing 1.8 cm lymph node. On color Doppler (▶ Fig. 8.2b) no blood flow is identified. The lesion was classified as BI-RADS 3.

Fig. 8.2 (a) On B-mode imaging the mass is a 1.8 cm lesion with the appearance of a lymph node. The cortex of the lymph node is relatively uniform in size, and the central echogenic fat is maintained. (b) On power Doppler no blood flow is identified in the lesion. (c) On strain imaging the cortex of the lymph node is stiffer than the adjacent breast tissues, whereas the central fatty hilum (arrow) is soft as expected. The lesion (dotted line) is similar in size on the B-mode image and elastogram. (d) On shear wave imaging the lymph node has a low Vs of 2.6 m/s (20 kPa) consistent with a benign lesion.
On strain imaging (▶ Fig. 8.2c) the cortex of the lesion is stiffer than surrounding tissue, with the hilum of the lymph node soft and of similar stiffness to the adjacent fat. The elastogram/B-mode (E/B) ratio is 0.95, and the strain ratio is 3.8. On shear wave imaging (▶ Fig. 8.2d) the lymph node has uniform stiffness with a Vs of 2.6 m/s (20 kPa).
8.2.3 Diagnosis
Mature lymphocytes consistent with lymph node origin. The lesion was biopsied with a 20-gauge needle using a fine-needle aspiration (FNA) technique. The pathology was mature lymphocytes consistent with lymph node origin.
8.2.4 Discussion
Inflammation of lymph nodes by bacterial or granulamotous infections such as tuberculosis is known as lymphadenitis. The most common causes of axillary lymphadenitis are bacterial agents that are located in the normal flora of the skin. Focal lymphadenitis is prominent in streptococcal infection, tuberculosis, nontuberculous mycobacterial infection, tularemia, plague, and cat-scratch disease. Multifocal lymphadenitis is common in infectious mononucleosis, cytomegalovirus infection, toxoplasmosis, brucellosis, secondary syphilis, and disseminated histoplasmosis.170,171 Tuberculous lymphadenitis (or tuberculous adenitis) is a chronic specific granulomatous inflammation with caseation necrosis of the lymph nodes. On physical examination, tenderness, redness, swelling, fluctuation, or abscess formation are detected as a result of bacterial lymphadenitis, whereas tuberculosis lymphadenitis may result in cold abscesses, which develop so slowly that there are no signs of inflammation unless it becomes complicated.
In this case a larger than normal (1.8 cm) axillary lymph node is identified. No other conventional sonographic abnormality is identified. On SE the hilar fat is identified as soft central tissue. The cortex is stiffer than adjacent tissue with an E/B ratio of 0.95. The strain ratio of the cortex is 3.8. On SWE the lymph node has a Vs of 2.5 m/s (19 kPa). The SE findings are benign as are the SWE findings.
Based on the proposed elastography classification system (similar to the BI-RADS classification) presented in Chapter ▶ 5 the lesion has an ~ 0% probability of malignancy.
8.3 Case 3: Lymph Nodes—Metastatic Adenocarcinoma to Axillary Lymph Node
8.3.1 Clinical Presentation
A 63-year-old woman with a history of left invasive ductal breast cancer presents with a new palpable mass in her left breast. On mammography a 1.5 cm irregular, hypoechoic mass is identified, and a lobular mass is also identified in the axilla. The mammogram was classified as BI-RADS 0, and an ultrasound was advised for further workup.
8.3.2 Ultrasound Findings
On B-mode imaging (▶ Fig. 8.3a) there is a lobular mass in the axilla. The normal lymph node appearance is not identified. The mass has marked increased blood flow on power Doppler imaging (▶ Fig. 8.3b) and color Doppler imaging (▶ Fig. 8.3c) with blood vessels noted entering the cortex of the lymph node. The breast mass is not presented here.
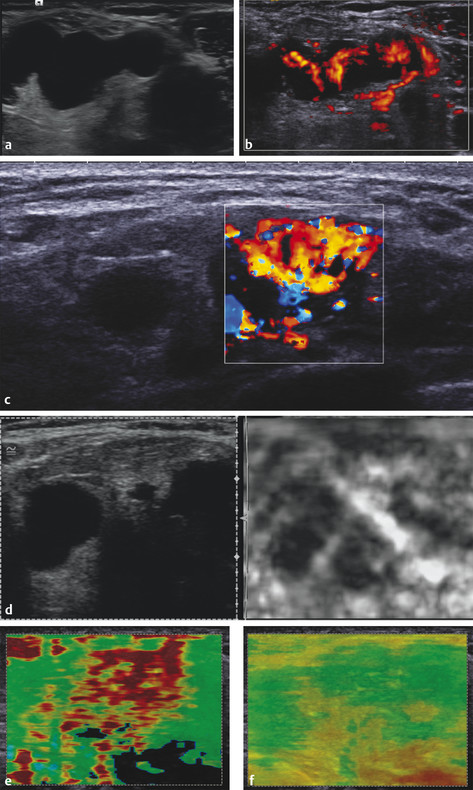
Fig. 8.3 (a) B-mode image of the axilla demonstrated several well circumscribed masses. The lesions did not have a normal lymph node appearance with absence of the central fat. (b) The power Doppler image demonstrates a large amount of internal blood flow. Some blood vessels enter through the cortex of the lymph node. (c) The color Doppler image demonstrates similar findings as (b). (d) On strain elastography the lymph node is stiffer than surrounding tissue and has an elastogram/B-mode (E/B) ratio of 1.1, suggestive of a malignancy. (e) On shear wave imaging the lesion has a Vs of > 7.7 m/s (> 180 kPa), highly suggestive of a malignancy. (f) The quality map confirms adequate shear waves are generated for accurate interpretation.
On SE (▶ Fig. 8.3d) the abnormal lymph node is stiffer than adjacent tissue with an E/B ratio of 1.1 and a strain ratio of 4.7. The lesion has a score of 5 on the 5-point color scale. On SWE (▶ Fig. 8.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree