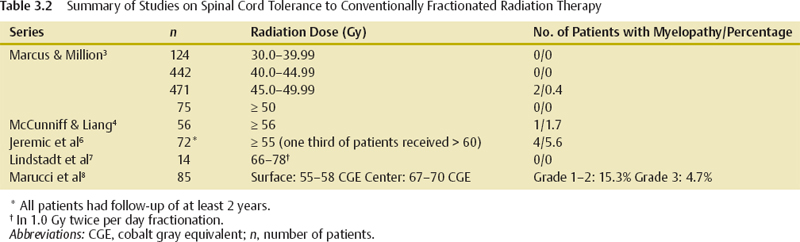
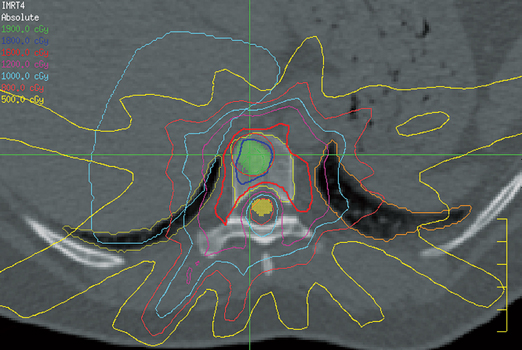
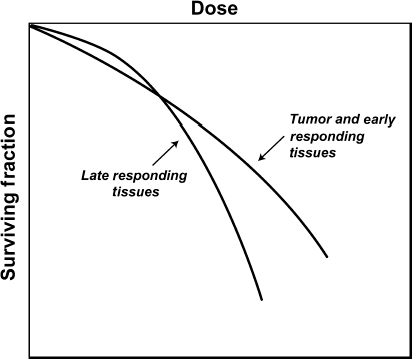
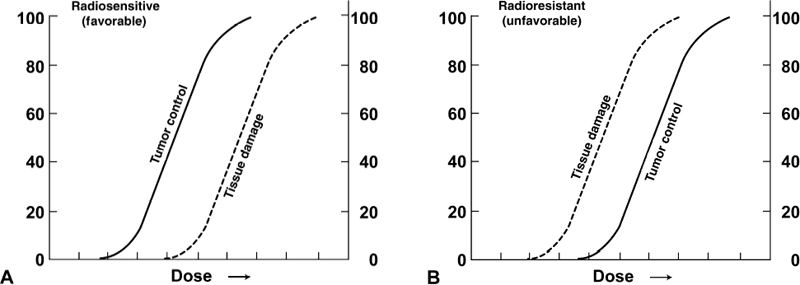
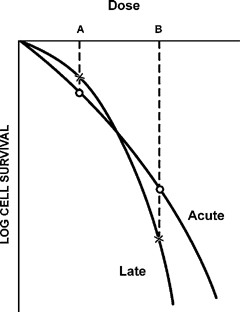
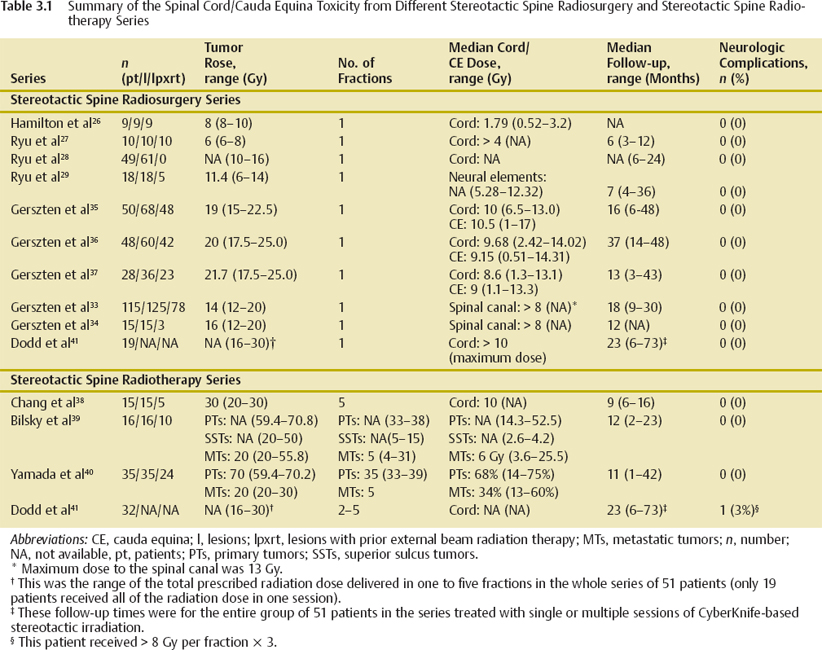
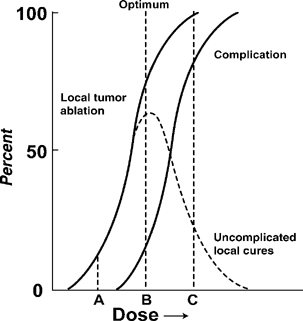
3 Stereotactic spine radiosurgery and stereotactic spine radiation therapy are advanced radiation therapy techniques that enable focused delivery of radiation treatments to spinal lesions while sparing the spinal cord. A very steep radiation dose fall-off beyond the target volume is a prerequisite for a stereotactic radiation delivery system. Because of this favorable dosimetric characteristic, it is possible to treat spinal lesions with a few fractions or only one fraction of a high dose of radiation and to more safely give a higher radiation dose than could be given by conventional radiotherapy techniques. It is also possible to re-irradiate spinal lesions that have previously been irradiated by avoiding the spinal cord as much as possible. Radiation-induced myelopathy is one of the most feared complications associated with radiation therapy. Although there has been ample experience with using conventional external beam irradiation to treat spinal tumors, as well as growing experience with stereotactic techniques, the true spinal cord tolerance to radiation has not been clearly defined due to conservative dose constraints placed on the spinal cord. Although very limited clinical data exist on the spinal cord’s tolerance to re-irradiation, practitioners of stereotactic body radiation therapy often encounter this situation. This chapter examines clinical spinal cord tolerance in the context of radiobiology, historical literature on conventional radiation therapy, and recent reports in the literature on stereotactic radiation for spinal tumors. Demyelination and necrosis of the spinal cord, both being manifestations of white matter injury, are the main morphologic features of radiation-induced myelopathy, although they are not pathognomonic of radiation injury.1 Apart from the white matter changes, vasculopathies and glial reaction can also be seen in radiation-induced myelopathy.1 Injury of the microvasculature has been implicated as a mechanism of myelopathy, but there are circumstances in which white matter necrosis occurs without accompanied vascular changes in the previously irradiated areas. Glial reaction has been observed in other demyelinating conditions not related to radiation injury, and it is believed it may have some role in radiation myelopathy. There is some suggestion that the cytokine network in the central nervous system may also have a role in radiation myelopathy.1 The use of intensity-modulated radiation therapy (IMRT) can create highly conformal dose distributions for spinal tumors with steep dose gradients that spare the spinal cord (Fig. 3.1). The use of stereotactic radiation techniques enables delivery of IMRT with millimeter precision. The combination of these techniques translates into high-dose, highly conformal irradiation that can be delivered with much greater safety than previously possible. From a radiobiological standpoint, this means that an increased therapeutic ratio is created with greater separation between the normal tissue complication curve for the spinal cord and the tumor control probability curve for the spinal tumor. The spinal cord, a late responding tissue, is highly sensitive to fraction size, as shown in Fig. 3.2, and is therefore best treated with relatively small fraction sizes when using conventional radiation therapy. Whereas hypofractionated stereotactic radiation uses larger fraction sizes, the steep dose gradients associated with IMRT previously described permit one to keep the actual fraction size seen by the spinal cord relatively small, so that late effects are minimized. It should be emphasized that conventional radiation therapy is very useful and should be considered the first line of radiation treatment for radiosensitive lesions of the spine such as breast cancer, plasmacytoma, lymphoma, and germ cell tumors, where the tumor control curve lies to the left of the normal tissue complication curve (Fig. 3.3A). However, for recurrent spinal tumors previously irradiated, as well as radioresistant tumors such as renal cell carcinoma, melanoma, and sarcomas, the tumor control curve lies to the right of the normal tissue complication curve (Fig. 3.3B). In these cases, conventional irradiation is often inadequate, as tumoricidal doses cannot be given without exceeding spinal cord tolerance. One must then resort to steretoactic spine radiation techniques to improve the therapeutic window that will allow higher doses to be given to the tumor while sparing the spinal cord. The large dose per fraction used in hypofractionated radiation therapy or single-session radiosurgery may help overcome radioresistant tumors, which are late responding tissues, by “getting over the shoulder,” going from dose point A to dose point B, resulting in greater log cell kill (Fig. 3.4). Figure 3.1 Intensity-modulated radiation therapy plan for stereotactic spine radiosurgery delivering 16 Gy to the entire T9 vertebral body and 18 Gy to the gross tumor volume; the spinal cord dose was limited to < 10 Gy. Figure 3.2 Normal tissue effect of smaller versus larger fractions of radiation therapy on early and late responding tissues. (Adapted from Hall EJ, ed. Radiobiology for the Radiologist. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2000:401, with permission.) The studies reported to date on stereotactic irradiation of spinal tumors in general show that these techniques are safe (Table 3.1). The problem for one trying to determine spinal cord tolerance is that the field has done such a good job of minimizing spinal cord complications, that the incidence of such occurrences is too low to make any determinations on what is the upper bound of a safe dose. For instance, in our review of 13 studies on stereotactic spine irradiation involving 459 patients, only Dodd et al41 reported any neurologic complication. The tumor control curve and normal tissue complication curve can be combined into an uncomplicated local cure curve (Fig. 3.5). Although it is clear that practitioners are operating along this curve with almost no complication somewhere between dose A and dose B, it is not clear what the optimum dose B is because the upper limit has not yet been defined. From our own data at M. D. Anderson Cancer Center in Houston, Texas, it appears that giving spinal tumors 27 Gy in three fractions or 30 Gy in five fractions while limiting the spinal cord to < 10 Gy is relatively safe. However, this spinal cord constraint may be overly conservative. How much to relax this constraint is currently unknown. For single-session stereotactic radiation series reported by others, it appears that limiting the surface dose of the spinal cord to 10, 12, and perhaps even 14 Gy appears safe, although patient numbers are still limited and follow-up is relatively short. Further experience with larger numbers of patients and longer follow-up will be needed. It is currently unclear and remains to be seen how much higher a surface dose the spinal cord will tolerate in a single fraction. Figure 3.3 Tumor control probability and incidence of tissue damage as a function of dose for radiosensitive (A) and radioresistant (B) tumors. (Reprinted from Rubin P. Clinical Oncology: A Multidisciplinary Approach for Physicians and Students. 7th ed. Philadelphia: Elsevier; 1993, with permission.) Figure 3.4 Compared with small fraction sizes (dose A) used in conventional radiation therapy, greater fraction sizes (dose B) used in hypofractionated radiation therapy may help overcome radioresistance in tumors with low α/β, which behave like late responding tissues. (Adapted from Fowler JR, Fractionation and therapeutic gain. In: Stell GG, Adams GE, Peckham MJ, eds. The Biological Basis for Radiotherapy. Philadelphia: Elsevier; 1983:181–194, with permission.) Traditionally, the spinal cord tolerance is generally accepted to be between 45 and 50 Gy in conventional fractionation. Emami et al estimated the TD 5/5 (the radiation dose at which there is a 5% risk of radiation myelopathy at 5 years from radiation therapy) for irradiation of 5, 10, and 20 cm of spinal cord in conventional fractionation to be 50, 50, and 47 Gy, respectively.2 However, this estimate was based on data that went back as far as the 1940s. Data in the literature suggest that the spinal cord tolerance to conventional radiation should be higher than the estimated level of 45 to 50 Gy (Table 3.2). Marcus and Million reviewed the 1112 evaluable patients treated with radiation therapy for head and neck cancer.3 These patients received > 30 Gy to > 2 cm of spinal cord and were followed for at least 1 year. The incidence of myelitis was 0.18%. The risk of radiation-induced myelitis was 0/124 at 30.0 to 39.99 Gy, 0/442 at 40.0 to 44.99 Gy, 2/471 at 45.0 to 49.99 Gy, and 0/75 at a cord dose of 50 Gy or higher.3 One can conclude from these data that the spinal cord tolerance has not been reached with these doses. McCunniff and Liang examined the rate of myelitis in 144 patients who received 56 Gy or higher to a portion of the cervical spinal cord during head and neck radiation therapy.4 Most of the patients received ≥ 60 Gy to the cervical spinal cord in 1.33 to 2.0 Gy fractions. Among the 53 patients (approximately half of them received 60 Gy or higher to the spinal cord) who had at least 2 years of follow-up, only 1 of them developed spinal cord injury 20 months after treatment.4 The investigators at Princess Margaret Hospital, Toronto, did not observe any cases of radiation-induced myelopathy in patients who received 50 Gy to the spinal cord if conventional fractionation (1.8–2.0 Gy) was used.5 Schultheiss et al estimated the TD 5/5 to be between 57 and 61 Gy and the TD 50/5 to be between 68 and 73 Gy in conventional fractionation.1 Jeremic and colleagues examined the incidence of radiation-induced myelopathy in the cervical spinal cord at doses of ≥ 55 Gy.6 Seventy-two of 176 patients had follow-up longer than 2 years. One third (26 patients) of those patients received a dose of > 60 Gy with fraction sizes of 1.57 to 1.7 Gy. Four (5.6%) patients developed permanent radiation myelitis.6 In adult patients with diffuse pontine glioma, hyperfractionated regimens delivering a total dose of > 70 Gy have been used without any incidence of myelitis.7 This suggests that smaller fraction sizes may increase spinal cord tolerance to radiation as predicted by the linear-quadratic model of radiation response, although only a small segment of cervical spinal cord received the prescribed dose. In a study of combined proton-photon radiation therapy, the dose constraints to the surface of the cervical spinal cord and the center of the cervical spinal cord were 67 to 70 and 55 to 58 cobalt gray equivalent (CGE), respectively. The spinal cord toxicity was graded using the European Organization for Research and Treatment of Cancer (EORTC) and Radiation Therapy Oncology Group (RTOG) late effects scoring system. With a median follow-up of 41.3 months, 15.3 and 4.7% of the patients developed grade 1 to 2 and grade 3 toxicity, respectively.8 Figure 3.5 Dose A results in low probability of tumor control and low complication rate. Dose B (optimum dose) achieves high probability of tumor control and low complication rate. Dose C results in a high probability of tumor control and high complication rate. The dashed curve represents the probability of uncomplicated local cures. (Adapted from Mendelsohn ML. The biology of dose-limiting tissues. In: Time and Dose Relationships in Radiation Biology as Applied to Radiotherapy. Brookhaven National Laboratory [BNL] Report 5023 [C-57]. Upton, NY: Brookhaven National Laboratory; 1969:154–173, with permission.) Hypofractionated radiation therapy is usually given in a palliative setting. Because of the different fraction sizes used, it is difficult to make comparisons between studies. Macbeth et al from the Medical Research Council estimated the risk of myelopathy in patients treated with different hypofractionated regimens for lung cancer.9 Those regimens were 8.5 Gy x 2 (n = 524), 4.5 Gy x 6 (n = 47), 5 Gy x 6 (n = 36), 3 Gy x 10 (n = 88), 3 Gy x 12 (n = 126), and 3 Gy x 13 (n = 153). The corresponding rates of myelopathy were 3/524 (0.6%), 0, 0, 0, 0, and 2/153 (1.3%), respectively.9 For the three patients who developed radiation myelopathy after 8.5 Gy x 2 fractions, the time of onset ranged from 8 to 42 months after radiation therapy compared with an onset time of 8 to 10 months for the two patients who developed radiation myelopathy after 39 Gy in 13 fractions.9 Because all the patients were treated with two-dimensional techniques in the study, the spinal cord doses stated were approximate. The authors may have underestimated the actual dose delivered to the spinal cord because it might be 5% greater than the prescribed dose as a result of tissue lateral effect and sloping chest.9 Assuming that the alpha/beta (α/β) value is 2 Gy (as suggested by the authors) and taking into account the 5% hot spot, the estimated equivalent biological total doses given as 2 Gy fractions were 48.8, 47.7, 57.1, 40.6, 48.7, and 52.7 Gy, respectively.7 No radiation-induced myelopathy was observed in patients who received 45 Gy in 15 fractions (3 Gy per fraction) in two studies.10,11 In a randomized trial comparing short-course versus split-course radiation therapy in metastatic spinal cord compression, approximately half of the patients (n = 142) received 16 Gy in two fractions for spinal cord compression.12 With a median follow-up of 33 months, none of those patients were scored to have late toxicity, although 10 of the 93 patients (10.8%) who were ambulatory before treatment lost the ability to walk after treatment.12
Clinical Spinal Cord Tolerance to Radiosurgery
 Overview of Mechanisms of Radiation-Induced Myelopathy
Overview of Mechanisms of Radiation-Induced Myelopathy
 Radiobiology of Spinal Cord Tolerance
Radiobiology of Spinal Cord Tolerance
 Spinal Cord and Cauda Equina Tolerance
Spinal Cord and Cauda Equina Tolerance
Spinal Cord Tolerance to Conventionally Fractionated Radiation Therapy
Spinal Cord Tolerance to Hypofractionated Radiation Therapy
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree