Abstract
Purpose
To assess the performance of routine abdomen/pelvis CT in detecting colorectal cancer.
Methods
A retrospective dataset consisting of 204 routine abdomen/pelvis CTs was compiled based on review of our institution’s pathology/imaging archives. 64 cases had pathologically confirmed colorectal cancer, while 140 cases had no colonic neoplasms on colonoscopy. Two radiologists blinded to the patient history and imaging indication reviewed the cases independently. They scored each case for any colonic abnormality which could represent colorectal cancer. The imaging abnormality location, morphology, presence of regional lymphadenopathy, and degree of diagnostic confidence were recorded.
Results
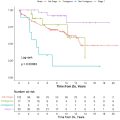
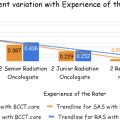
Reviewers demonstrated a sensitivity of 64–77% and specificity of 83–86% for detection of colorectal cancer. Detected tumors were significantly larger than missed cancers, with mean maximum diameter of 5.2–5.7 cm for detected cancer (n = 81) and 2.8–2.9 cm for missed cancer (n = 25) (reviewer 1 p < 0.001; reviewer 2 p = 0.01). Positive predictive value (PPV) strongly correlated with diagnostic confidence, with 100% of pooled cases (39/39) reported as 5 (Almost Certainly Neoplastic) positive for cancer compared to 53% of cases (17/32) reported as 3 (Could be Benign or Neoplastic). The presence of regional lymphadenopathy was a strong predictive feature, with 94% of pooled cases with identified lymphadenopathy (48/51) positive for cancer compared to 51% (42/82) without lymphadenopathy (p < 0.001).
Conclusion
While colorectal cancers larger than 3 cm were detected with relatively high specificity, abdomen/pelvis CT performed poorly with smaller tumors. Radiologist-reported diagnostic confidence was strongly associated with diagnostic accuracy. Regional lymphadenopathy is a highly specific finding, although insensitive.
Highlights
- •
Abdomen/pelvis CT has high sensitivity for detection of T3 or T4 colorectal cancers.
- •
Radiologist-reported diagnostic confidence was strongly associated with accuracy.
- •
Regional lymphadenopathy is a highly specific finding for colorectal cancer.
1
Introduction
Colorectal cancer is the third most common cancer and second most common cause of cancer-related death in the United States [ ]. Initial tumor stage is strongly associated with mortality, resulting in a 5 year relative survival rate of 92% for stage I colon cancer compared to 65% for stage IIB and 12% for stage IV disease [ ]. Screening colonoscopy is estimated to reduce mortality by approximately 60–70%, supporting the importance of early detection [ ]. Yet despite this benefit, only 59% of adults in the United States were up to date with age-appropriate screening as of 2021 [ ].
Computed tomography (CT) is a commonly used imaging modality, with a reported utilization rate of 428 exams per 1000 person-years amongst older adults in 2016 [ ]. Given the large number of CT exams being performed, detection of unsuspected colorectal cancer on even a small proportion of abdomen/pelvis CTs could have a significant impact on early diagnosis rates and potentially mortality.
Reported sensitivity rates for colorectal cancer on routine abdomen/pelvis CT exams range from 72.4 to 100% [ ]. The study by Colvin et al. [ ] reported a 100% detection rate, although their dataset included only 2 cases with colorectal cancer out of 96 total patients. The largest study by Johnson et al. [ ] reported an overall detection rate of 82.3% using a dataset of 209 patients with colorectal cancer; the radiologists in that study reviewed the CT images with knowledge of each tumor’s location and size. However, the task of identifying unsuspected colorectal cancer on a routine abdomen/pelvis CT is different from that of a radiologist reviewing a CT dataset composed entirely of patients with known cancer. While high sensitivity is paramount, false positive cases result in unnecessary follow-up colonoscopies with associated procedural risk, patient anxiety, and utilization of limited resources.
The purpose of this study is to report the detection rate of colorectal cancer in a mixed dataset containing CT exams from both patients with and without cancer. The predictive value of morphologic imaging features, presence of lymphadenopathy, and diagnostic confidence were also evaluated. Incorrectly identified cases, both false positives and negatives, were reviewed to identify common characteristics that may guide improvements in detection performance.
2
Methods
2.1
Patients
This retrospective study was approved by the local institutional review board with a waiver for consent due to minimal risk. A search of our institutional electronic health record identified 64 patients with pathologically proven colorectal adenocarcinoma and a pre-treatment routine abdomen/pelvis CT performed within 3 months either before or after diagnosis. For all cases, initial pathologic diagnosis was established from colonoscopic biopsy, with biopsy dates spanning August 21, 2017 through December 21, 2021. If available, subsequent surgical resection pathology reports were reviewed to determine tumor size as well as T and N staging. Primary tumors of the cecum or ileocecal valve that involved the terminal ileum were included, while tumors arising entirely from the terminal ileum were not. Patients were excluded if CT was obtained after polypectomy with follow-up biopsy or resection showing no residual carcinoma. For the negative control cases, 140 patients were identified with a routine abdomen/pelvis CT performed within 1 year after or any time before a colonoscopy without evidence of malignancy.
All CTs were reviewed using 2.5 or 5 mm axial slices with coronal and sagittal reformats. Due to the large number of different CT scanners and protocols used throughout this cohort, as well as the inclusion of exams performed at outside institutions for which this information was not available, these technical parameters were not reported.
2.2
Image analysis
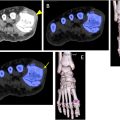
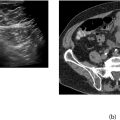
Two board-certified, fellowship-trained abdominal radiologists (OH and SB), with 5 and 18 years of experience respectively, reviewed each of the CT exams while blinded to patient history and exam indication. For each exam they reported whether an abnormality suspicious for colorectal cancer was present; if so they also noted the location of the abnormality (rectum, sigmoid, descending colon, transverse colon, ascending colon, cecum, or terminal ileum), morphologic descriptor, presence of regional lymphadenopathy (Yes/No), and degree of diagnostic confidence. Morphologic descriptors, as initially reported by Johnson et al. [ ], consisted of (1) concentric bowel wall thickening, (2) asymmetric bowel wall thickening, (3) polypoid intraluminal mass, and (4) exophytic mass ( Fig. 1 ). Diagnostic confidence was reported on a 1–5 Likert scale, with 1 indicating ‘Almost Certainly Benign’, 2 – ‘Probably Benign’, 3 – ‘Could be Benign or Neoplastic’, 4 – ‘Probably Neoplastic’, and 5 – ‘Almost Certainly Neoplastic’.

Although on surgical resection pathology some tumors were noted to involve multiple contiguous segments of colon (i.e. cecum and ascending colon), for each imaging abnormality the reviewers reported only the single segment of bowel that was most involved. If a reviewer correctly identified a case with colorectal cancer but the reported site of imaging abnormality was discordant with pathologic findings, this was classified as a false negative. Reviewers could report multiple abnormalities if they perceived two or more discrete, discontinuous sites of possible cancer; these cases were classified as true positive if any of the reported abnormalities were concordant with pathologic findings.
2.3
Statistical analysis
Reviewer performance metrics including sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). Inter-rater agreement was calculated with Cohen’s kappa. Continuous variables were summarized as mean ± standard deviation and normality was assessed with the Shapiro-Wilk test. Age was compared with unpaired two-tailed t-tests and tumor size was compared with the Mann-Whitney U test. Categorical variables were evaluated with Fisher exact tests. Linear regression was used to evaluate the association between cancer detection and diagnostic confidence. Statistical analysis was performed with R v4.0.5 (The R Foundation).
3
Results
3.1
Patient demographics
Patient demographic data is summarized in Table 1 . Of the patients without colorectal cancer, 48% (67/140) were female compared to 47% (30/64) for those with cancer (p > 0.99). The average age of patients without cancer was 57 ± 11 years (range 31–79) compared to 60 ± 16 years (range 25–90) for patients with cancer (p = 0.10). Of the patients with cancer, 33% (21/64) underwent an abdomen/pelvis CT before colonoscopic biopsy while 67% (43/64) underwent a CT after biopsy. The average time between CT and diagnosis was 16 ± 14 days (range 2–48) for patients with CT first compared to 12 ± 14 days (range 0–80) for patients with biopsy first. For patients with cancer, 61% (39/64) had a CT with only intravenous contrast, 2% (1/64) with only oral contrast, 34% (22/64) with intravenous and oral contrast, and 3% (2/64) without contrast. For patients without cancer, 84% (117/140) had a CT with only intravenous contrast, 9% (13/140) with intravenous and oral contrast, and 7% (10/140) without contrast.
| Cancer Absent (n = 140) | Cancer Present (n = 64) | p | ||
|---|---|---|---|---|
| Age (Years) | Mean (SD) | 57 (11) | 60 (16) | 0.10 a |
| Range | 31–79 | 25–90 | ||
| Sex | Male | 73 (52%) | 34 (53%) | >0.99 b |
| Female | 67 (48%) | 30 (47%) | ||
| Cancer present, surgical pathology available (n = 53) | ||||
| Tumor size (max diameter, cm) | Mean (SD) | 4.8 (2.8) | ||
| Range | 0.1–16.0 | |||
| T stage | Tis | 1 (2%) | ||
| T1 | 4 (8%) | |||
| T2 | 9 (17%) | |||
| T3 | 32 (60%) | |||
| T4 | 7 (13%) | |||
| N Stage | N0 | 32 (60%) | ||
| N1 | 12 (23%) | |||
| N2 | 9 (17%) | |||
| CT before diagnosis (n = 21) | CT after diagnosis (n = 43) | |||
| Time between diagnosis and CT (Days) | Mean (SD) | 16 (14) | 12 (14) | |
| Range | 2–48 | 0–80 | ||
a p value determined with the Student’s t -test.
Surgical resection pathology data was available for 83% (53/64) of patients with cancer ( Table 1 ). For the 11 patients without surgical resection data, four received post-diagnosis care at an outside institution, three declined treatment, two were ineligible for surgery due to distant metastatic disease, one was lost to follow-up, and one died several days after diagnosis from an unrelated medical condition. Average maximum tumor diameter was 4.8 ± 2.8 cm (range 0.1–16). Most tumors were locally advanced, with 74% (39/53) classified as either T3 or T4, compared to 26% (14/53) as Tis, T1, or T2. Most patients had no nodal metastases, with 60% (32/53) classified as N0 compared to 40% (21/53) as either N1 or N2.
3.2
Detection performance
Reviewer 1 demonstrated a sensitivity of 64% and specificity of 86%, compared to 77% and 83%, respectively, for reviewer 2 ( Table 2 ). Inter-rater agreement was moderate (κ = 0.478). Reviewer data was combined using two different approaches: one in which a case was classified as positive only if both reviewers reported it as positive (Combined-Both) and one in which a case was classified as positive if either reviewer reported it as positive (Combined-Either). Combined-Both demonstrated a sensitivity of 58% and specificity of 96%, compared to 83% and 74% respectively for Combined-Either. For each reviewer and set of combined data, tumor T stage was significantly associated with detection rate. Stage Tis disease was detected at a rate of 0% (0/1) for both reviewers, compared to 56% (5/9) and 67% (6/9) for T2 disease for reviewer 1 and reviewer 2 respectively, and 71% (5/7) and 100% (7/7) for T4 disease. Detected cancer was significantly larger than missed cancer ( Fig. 2 ), with average detected tumor size of 5.7 ± 2.8 cm (n = 37) and missed tumor size of 2.8 ± 1.5 cm (n = 16) for reviewer 1 (p < 0.001) compared to 5.2 ± 2.8 cm (n = 44) and 2.9 ± 2.2 cm (n = 9) respectively for reviewer 2 (p = 0.01).