Author
Design
Patients (HR vs ablation)
Tumor size (cm)
Recurrence
Survival
Complication
Xu et al. [16]
Meta-analysis
1233 vs 1302
≤5
Lower for HR
Higher for HR
Higher for HR
Zhou et al. [17]
Meta-analysis
667 vs 744
≤5
Lower for HR
Higher for HR (similar when diameter ≤3 cm)
Higher for HR
Li et al. [18]
Meta-analysis
436 vs 441
≤5
Lower for HR
Higher for HR
N/A
Liu et al. [20]
Meta-analysis
534 vs 654
≤5
Lower for HR
Similar
Similar
Cho et al. [7]
Meta-analysis
550 vs 550
≤5
Lower for HR
Similar
N/A
Chen et al. [21]
Meta-analysis
339 vs 358
≤5
Lower for HR
Similar
Higher for HR
Tombesi et al. [22]
Meta-analysis
74 vs 71
≤2
Similar
Lower for HR
Higher for HR
Feng et al. [19]
RCT
84 vs 84
≤4
N/A
Similar
N/A
Huang et al. [9]
RCT
115 vs 115
≤5
Lower for HR
Higher for HR
N/A
Lü et al. [23]
RCT
54 vs 51
≤5
Similar
Similar
Similar
Wang et al. [22]
Case-control study
80 vs 114
≤5
Similar
Similar
Lower for HR
16.1.2 Prospective Cohort Study for HR and MWA/RAF
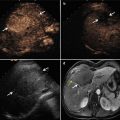
Our group is performing a prospective cohort study to compare the intermediate-term therapeutic effectiveness of HR with ultrasound-guided percutaneous cooled-tip MWA and RFA in the treatment of early-stage HCC within Milan criteria. From August 2008 to January 2013, 290 cases of biopsy-proved HCC patients with 364 nodules were treated by MWA or RFA treatment. Three hundred six patients with 339 nodules were treated by HR. The tumor size and tumor number of both groups were similar. The average age was 58.2 years old for ablation group and 53.7 years old for HR group (P < 0.001). Average operation times were significantly shorter in the ablation group (P < 0.001). The average intraoperative bleeding amounts were 20–3,100 ml (median 200 ml) for HR, while ablation with the bleeding amount less than 10 ml. Hospitalization costs were being significantly fewer in the ablation group (P < 0.001) as well.
The follow-up period was 2–54.8 months (median 21.6 months). The technique effectiveness (TE) rate was 99.2 % (361/364) in the tumors treated with ablation and 99.3 % (304/306) in those treated with HR, with no significant difference between the two groups (P = 0.85). Local tumor progression (LTP) was observed in 4.9 % (18/364) tumors at 1–38.5 months after the first ablation therapy and in 2.0 % (6/306) tumors at 1–17.5 months after the first HR (P = 0.04), respectively. There were no significant difference of LTP between the two groups in ≤3 cm tumors (P = 0.94). But for 3–5 cm tumors, ablation showed significant higher LTP compared with HR (P = 0.004). The 1-, 2-, and 3-year intrahepatic metastatic rates were 20.9, 31.9, and 45.1 % for ablation versus 14.5, 18.6, and 35.6 % for HR, respectively (P = 0.11) (Fig. 16.1). The 1-year, 2-year, and 3-year cumulative survival rates after ablation were 95.8, 89.4, and 83.9 %, and the 1-year, 2-year, and 3-year disease-free survival rates after ablation were 83.3, 71.4, and 64.4 %. The 1-year, 2-year, and 3-year cumulative survival rates after HR were 97.5, 91.2, and 84.1 %, and the 1-year, 2-year, and 3-year disease-free survival rates after HR were 81.6, 66.9, and 56.3 %. There were no significant differences of cumulative survival rates (P = 0.31) and disease-free survival rates (P = 0.71) between the two groups (Fig. 16.2) by using log-rank test analysis.



Fig. 16.1
Intrahepatic metastasis curves after thermal ablation and HR treatment of HCC. There is no significant difference between two groups (P = 0.11)

Fig. 16.2
(a) Overall survival curve comparison between thermal ablation and HR treatment of HCC. There is no significant difference between two groups (P = 0.31). (b) Disease-free survival curve comparison between thermal ablation and HR treatment of HCC. There is no significant difference between two groups (P = 0.71)
The major complication rates were 3.8 % (11/290) for ablation and 6.9 % (21/306) for HR (P = 0.10), respectively. Five needle seedings (1.4 %, 5/364) occurred at 6–42 months after ablation and one incision seeding (0.3 %, 1/306) occurred at 20 months after operation, respectively. There were four pleural effusion cases (1.4 %, 4/290) after ablation and ten cases (3.3 %, 10/306) after HR who needed drainage intervention. There was two gastrointestinal bleeding (0.7 %, 2/290) after ablation and none for HR. In addition, major complications occurred each after HR treatment, which were subphrenic abscess, abdominal cavity bacterial infection, gallbladder perforation, heart failure, bile leakage, adhesive intestinal obstruction, operative incision split, and intraoperative tumor rupture, respectively. There were no statistical differences for all the major complications between the two groups (P > 0.05).
16.1.3 Conclusion
The present prospective cohort study provides many valuable information to evaluate minimally invasive percutaneous MWA/RFA with traditional HR for <5 cm HCC therapy with relatively large series, long follow-up, and prospective data collection. The study performed the comparison in multiple parameters including liver function, operation time, hospitalization, cost, recurrence, survival, and complication. Furthermore, all the ablation procedures used cooled-tip applicators with larger ablation zone, which may increase the possibility of successfully ablation for 3–5 cm HCC.
In conclusion, for the early-stage (≤5 cm, ≤3 nodules) HCC treatment, ultrasound-guided percutaneous cooled-probe MWA/RFA and HR achieved similar intermediate-term effectiveness. Though hepatectomy showed better local tumor control for 3–5 cm tumor, ablation showed the advantages of lower expense, minimal invasion, and repeatability. Further study with long-term follow-up and more patients is expected to provide more reliable efficacy evaluation and survival analysis.
16.2 Comparative of MWA Versus RAF
16.2.1 Difference of Thermal Field Characteristics Between MWA and RFA
In RFA, a high-frequency alternating electrical current (375–500 kHz) is used to create ionic agitation, which produces frictional heat and heat conduction to achieve subsequent tissue necrosis [25, 26]. MWA uses electromagnetic energy to rapidly rotate adjacent polar water molecules in the surrounding tissue, which flip back and forth 2–5 billion times a second depending on the frequency of the microwave energy. The rapid friction produces heat, thus inducing cellular death via coagulation necrosis. Ionic polarization as another mechanism responsible for heat generation is a far less important mechanism in living tissue.
The difference between MWA and RFA characteristics are summarized as follows (Table 16.2): (1) the active tissue heating of RFA is limited to a few millimeters surrounding the active electrode, with the remainder of ablation zone relying on the conduction of electricity into the tissue [26]. Microwave uses electromagnetic energy with the much broader field of power density (up to 2 cm surrounding the antenna) to rapidly rotate adjacent polar water molecules to achieve primarily active heating, which can get a much broader zone of active heating [27]. (2) RFA is limited by the increase in impedance with tissue boiling and charring [26], because water vapor and char act as electrical insulators. MWA does not seem to be subject to this limitation. Therefore, temperature greater than 100 °C is readily achieved [28]. (3) Owing to the active heating ability, MWA can achieve higher intratumoral temperatures, larger ablation volumes, and shorter ablation time [28–31]. Because the cooling effect of blood flow is most pronounced within the zone of conductive rather than active heating, MWA is less affected by blood vessel-mediated cooling (the heat-sink effect). These benefits have the potential to allow for a more uniform tumor kill in the ablation zone, both within the targeted zone and perivascular tissue [31, 32]. (4) MWA allows for simultaneously multiple probes deployment to reduce the duration of therapy and increase the diameter of ablation zone [26–28]. (5) MWA does not require the placement of grounding pads, and the electrical energy is deployed in the target tissue only, which avoids applied energy losing and skin burns. Moreover, MWA is not contraindicated by the metallic materials like surgical clips or pacemaker.
Table 16.2
Different thermal characteristics between MWA and RFA
MWA | RAF | |
|---|---|---|
Frequency | 915, 2,450 MHz | 400–600 KHz |
Mechanism | Oscillation of polar molecule and ion | Oscillation of ion |
Temperature rise | High efficiency | Low efficiency |
Coagulation zone | Regular, narrow congestion zone | Irregular, wide congestion zone |
Ablation time | Shorter (3 cm with 10 min) | Longer (3 cm with 20–30 min) |
Ability of vessel coagulation | Strong | Weak |
Time to highest temperature | Faster (20–30 s) | Slower |
Highest temperature | Higher (15–25 °C) | Lower |
Ablated zone of in vivo | (3.9 × 2.4) cm | (3.2 × 1.6) cm |
16.2.2 Studies Status
For the comparison of two techniques in HCC, only a limited number of studies have been performed, most of which are retrospective studies and all with a relatively small samples and short-term follow-up (Table 16.3). The only reported randomized controlled trial was performed by Japanese researches in 2002 [33]. Most of the researches showed MWA and RFA achieved similar tumor necrosis effect and survival [34–37]. But Japanese researchers thought RFA had tumor control advantage in small liver lesions [38, 39]. However, randomized controlled trial with large sample and long-term follow-up is lacking and strongly recommended to provide evidence of evidence-based medicine.
Table 16.3
The clinical comparative studies for MWA and RFA
Author | Design
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
|---|