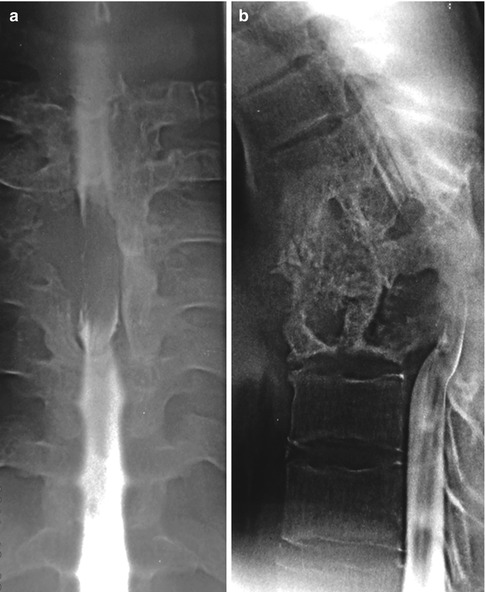
Fig. 18.1
A 73-year-old man presented with increasing low back and leg pain. Plain lumbar spinal radiography showed a compression fracture within the L2 vertebra as well as the “absent pedicle sign” at both L1 and L2. (a) Anteroposterior view. (b) Lateral view. In this patient, a hydatid cyst of the liver caused by Echinococcus multilocularis was surgically resected 30 years before the time of presentation
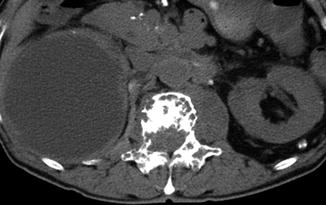
Fig. 18.2
CT shows the presence of multiloculated osteolytic lesions in the vertebral body and posterior elements. Periosteal reactions were observed

Fig. 18.3
Sagittal MRI views show multiseptated and multicystic lesions. Epidural extension of soft tissue with cord compression is also seen. T1-weighted (a) and T2-weighted (b) image
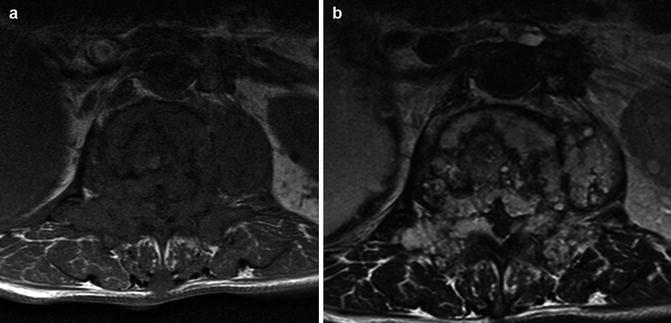
Fig. 18.4
Axial T1 (a) and T2 (b) MRI demonstrate involvement of neural structures, paraspinal muscles, and the liver

Fig. 18.5
Coronal T2-weighted MRI shows the presence of a complex T2 hyperintense mass in the paravertebral region with multiple septa
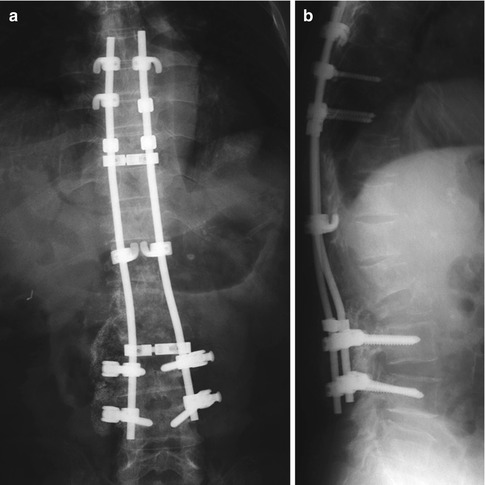
Fig. 18.6
Palliative surgery was performed with posterior decompression and instrumentation for persistent leg pain. Leg pain was significantly reduced. Spinal stability was maintained until the patient died (2 years after the surgery) (Courtesy of S. Satoh, MD) (a) Anteroposterior view. (b)Lateral view
Surgical Procedures
Laminectomy with complete resection of the cysts is the most frequently performed procedure. A posterior approach should be used to resect the involved posterior element and add posterior fixation. Care should be taken to avoid implant protrusion into the dorsal skin, decubitus ulcer formation, and vertebral fractures in the adjacent segments after posterior spinal reconstruction. An anterior approach to perform total corpectomy and bone grafting with a cage may be used when most of the disease is located in the vertebral body (Charles et al. 1988; Herrera et al. 2005). The anterior approach is useful for curative resection of infected vertebrae; however, care must be taken to avoid spread of the disease to the chest and abdominal cavities (Bhojraj and Shetty 1999). Surgical procedures used in spinal hydatidosis are discussed in detail in Chap. 14.
Surgery-Related Complications
Surgical Site Infection
In hydatid of the spine, there is not one cyst around which dissection can be carried out. The bone is infiltrated with a great number of minute cysts. In cases where leaked fluid containing parasites is left behind at the surgical site, concerns are raised about delay of skin closure, leading to deep pyogenic infection. It is particularly a cause of concern when surgical intervention is complicated by cerebrospinal fluid leakage. In this case, lumbar drainage may be required. Intensive muscle closure is also required during surgery to avoid fluid leakage. A plastic surgical procedure, such as musculocutaneous flap transfer, is often required for chronic infection. Although there have been few reports about larger series of spinal hydatidosis, Herrera et al. (2005) reported that 50 % of recurrence cases also have chronic wound infection with chronic productive sinuses that required several surgical debridements. Because surgery for spinal hydatidosis is extensive and the reappearance of postoperative surgical wound infection is frequent, perioperative antibiotic therapy is important.
Rupture of Cysts and Allergic Reactions
Another surgery-related complication is allergic reaction caused by rupture of the cyst. This reaction ranges from mild hypersensitivity to fatal anaphylaxis (Kök et al. 1993; Wellhoener et al. 2000; Laifer et al. 2002). Because spinal hydatidosis is usually advanced, rupture of the cyst into the surrounding tissue will already have occurred and the possibility of serious allergy manifesting during surgery is regarded as extremely low. However, this possibility makes close monitoring mandatory during surgery, with facilities available for treating potential complications, particularly anaphylactic shock and laryngeal edema (Khuroo et al. 1997).
Complications After Surgery
Recurrence
Recurrence remains a major problem in spinal hydatidosis (Figs. 18.7, 18.8, 18.9, and 18.10); the literature cites a rate of 30–100 % (Schnepper and Johnson 2004). The thin wall may easily rupture, either spontaneously or due to surgery, resulting in recurrence of multiple cysts (Schnepper and Johnson 2004). It is extremely difficult to resect the extradural lesions involving the spine without rupturing the hydatid cyst because the cysts are contained in narrow spaces within bone boundaries (Schnepper and Johnson 2004; Tabak et al. 2007). Therefore, the management of echinococcal cysts usually involves a combination of surgical resection and antihelminthic therapy.


Fig. 18.7
Recurrence of spinal hydatidosis. A 52-year-old man presented with intractable leg pain and motor paralysis. Two years before the time of presentation, anterior mass resection and autologous fibular grafting had been performed, followed by posterior decompression and fusion using an iliac bone graft at T6–T9. MRI shows cysts extending into the canal and compressing the spinal cord. T1-weighted (a) and T2-weighted (b) image