Over the past several years, there has been an increase in the discovery of thyroid cancers, likely because of the marked increased utilization of computed tomography (CT) and MR imaging. Despite the increase in number of thyroid cancers, the overall mortality remains unchanged because most of these cancers are the differentiated type and have a more indolent behavior. CT and MR imaging are important in the preoperative evaluation of thyroid goiters and thyroid cancer. This article discusses the imaging characteristics of benign and malignant thyroid diseases, and the important information that needs to be relayed to the surgeon.
Key points
- •
Both CT and MR imaging are important imaging modalities that incidentally detect benign and malignant thyroid disease.
- •
Cross-sectional imaging is not typically the first-line imaging technique for thyroid nodule characteristics but is extremely beneficial for surgical staging.
- •
Staging of papillary thyroid cancer depends on a combination of imaging findings, histology, and the patient’s age.
- •
Calcifications and/or cystic changes involving cervical lymph nodes are highly concerning for metastatic lymphadenopathy.
Introduction
Many benign and malignant disorders can occur in the thyroid. Some thyroid diseases can be subclinical; however, others present with structural (ie, thyroid goiter) or functional (ie, thyroiditis) abnormalities. , Thyroid cancer is the most common endocrine malignancy in the United States, affecting more than 400,000 people per year, with the incidence doubling between 2000 and 2009. This higher number of cases is likely due to increased usage of computed tomography (CT) and MR imaging. Incidental thyroid nodules are often found on neck/cervical spine imaging performed for a vast array of non–thyroid-related etiologies. Despite this overall increased incidence, patient mortality has not changed. CT and MR imaging are especially important in the presurgical evaluation of thyroid diseases for extent of disease, involvement of the adjacent structures, and presence of distant disease. ,
Normal anatomy and imaging technique
The thyroid structure consists of 2 lobes, draped over the trachea and connected by the isthmus at midline. , The thyroid is hypervascular, part of the visceral space, and encapsulated by the middle layer of the deep cervical fascia. Typically, each lobe measures approximately 2.0 × 3.0 × 5.0 cm (transverse × anteroposterior × craniocaudal) with isthmus measuring up to 0.3 cm. , The superior border of the thyroid extends to level of the mid-thyroid cartilage and extends inferiorly to the fifth or sixth tracheal ring. The thyroid wraps around the trachea and into the tracheoesophageal grooves (TEG), containing the recurrent laryngeal nerve (RLN). The common carotid arteries (CCA) and internal jugular veins (IJV) are posterolateral, and the strap muscles are anterior to the thyroid ( Fig. 1 ). The thyroid is hypervascular and supplied mainly by superior thyroid artery from the external carotid artery and the inferior thyroid artery from the thyrocervical trunk. In a small percentage of patients, a thyroid IMA arises directly from the aorta. The esophagus is posterior and separated from the thyroid by the TEG ( Fig. 2 A). The lymphatic drainage for the thyroid is variable, including the internal jugular chain, paratracheal, mediastinal, and retropharyngeal regions.
| Imaging Technique and Protocol | ||
|---|---|---|
| Computed Tomography | MR Imaging | |
| Field of view | Skull base to the carina | Skull base to the carina |
| Patient positioning | Patient’s arm at the side with neck in neutral position to slightly extended to mimic operating room positioning a, | Patient’s arm at the side with neck in neutral position to slightly extended to mimic operating room positioning a, |
| Imaging acquired |
|
|


Imaging characteristics
The imaging appearance of the thyroid varies with the modality. Many different modalities are used to evaluate the thyroid, including ultrasonography, nuclear medicine scintigraphy, CT, and MR imaging.
On nonenhanced (NE) CT, the thyroid is intrinsically hyperdense (80–100 Hounsfield units) when compared with the musculature due to elevated iodine content (see Fig. 1 A). The thyroid is able to concentrate 25 to 50 times more iodine than serum. The thyroid attenuation directly correlates with thyroid function; therefore, the more decreased the thyroid function the less hyperdense the thyroid. On contrast-enhanced (CE) CT, the thyroid avidly enhances due to hypervascularity (see Fig. 1 B). The thyroid on MR imaging has homogeneous signal intensity, slightly greater than that of the strap musculature on T1-weighted and T2-weighted imaging ( Fig. 2 A, B). After the administration of gadolinium, the thyroid homogeneously enhances ( Fig. 2 C).
Thyroid pathology
Benign
Imaging has significantly increased over recent years, resulting in an increased number of incidental findings, unrelated to the examination indication. Many incidental findings are benign thyroid nodules, identified on ultrasonography (9%–33%), cross-sectional scans (16%–18%), and PET (1%–2%). , Incidence of these nodules increase with age, and they occur more frequently in women. Not all incidental nodules need ultrasonography follow-up, given the overall indolent behavior of most thyroid cancers ( Table 1 ). In addition, these nodules only have a 1% to 2% risk of malignancy. If, however, a nodule has focal fludeoxyglucose uptake on PET, fine needle aspiration needs to be performed, as there is a 26% to 50% risk of primary thyroid malignancy. Although thyroid nodules can be detected with CT and MR imaging, ultrasonography remains the best for nodule characterization.
| Age, y | Nodule Size, cm | Recommendation |
|---|---|---|
| <35 | <1 | No additional imaging in low-risk patient |
| ≥1 | Ultrasound advised | |
| ≥35 | <1 | No additional imaging in low-risk patient |
| 1–1.4 | Additional imaging at providers discretion | |
| ≥1.5 | Ultrasound advised |
Incidental thyroid nodules
The goal of the evaluation for these incidental thyroid nodules is to determine malignancy risk, whereas most are benign. CT is often used in patients with head and neck cancer for operative planning, restaging, and follow-up; however, this is not necessarily true with thyroid cancer. Characterization of thyroid nodules on CT or MR imaging is largely nonspecific; however, these studies can help with large or retrosternal thyroid goiters (TGs), which are not adequately assessed on ultrasonography due to the trachea and sternum. CT also characterizes calcifications better than ultrasonography . Calcifications may be “egg-shell,” rimlike, or curvilinear, and 22% of these types of calcifications are associated with malignancy.
Thyroid goiter
TG occurs due to abnormal thyroid growth with or without substernal extension. A simple TG occurs in the absence of autoimmune disease, thyroiditis, thyroid dysfunction, or thyroid malignancy. Abnormal growth occurs over several years, most commonly in 50-year-old to 60-year-old women, and can be due to environmental and/or genetic factors. Functional (ie, hyperthyroidism) or structural abnormalities can cause a multitude of compressive symptoms (ie, dyspnea). Multinodular TG is heterogeneous due to nodularity, hemorrhage, calcifications, cyst formation, and scarring ( Fig. 3 ). There can be asymmetric hypertrophy of the thyroid with extension substernally or into the posterior mediastinum. CT is important for presurgical evaluation, and there are specific details the surgeon needs to know: degree of substernal extension, displacement or compressed structures, symmetry of the vocal folds suggesting paralysis, and extrathyroidal extension suggesting superimposed malignancy. Imaging findings suggestive of malignancy include invasion of adjacent structures, rather than simple displacement or compression, and also the presence of cervical lymphadenopathy ( Fig. 4 ).


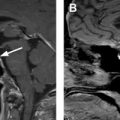
Thyroiditis
Thyroiditis is a benign inflammatory condition, often clinically apparent without need for imaging. However, Riedel’s thyroiditis (RT) has fairly characteristic imaging findings. Although the etiology remains largely unknown, it is thought to be autoimmune. RT occurs due to a rare fibrotic condition in which thyroid tissue is destroyed with infiltration of the adjacent soft tissues. This overgrowth of fibrosing connective tissue increases over time leading to a palpable, firm, painless enlarging thyroid mass with compressive symptoms (ie, dyspnea, dysphagia, hoarseness, aphonia). On clinical examination, the differential for RT includes malignancy, such as anaplastic thyroid cancer (ATC), lymphoma, and sarcoma. Definitive treatment of RT remains surgery to relieve the compressive symptoms. RT can be suggested on MR imaging due to characteristic imaging features of fibrosis. The thyroid will be hypointense on T1/T2-weighted images ( Fig. 5 ) with homogeneous enhancement. These imaging characteristics are in contradistinction to Hashimoto thyroiditis, thyroid carcinoma, and lymphoma, which are T2 hyperintense. RT also can be associated with mediastinal fibrosis, retroperitoneal fibrosis, and sclerosing cholangitis.