Introduction
Major advances in the field of pediatric cardiology and cardiac surgery over the last several decades have led to an improvement in survival rates of the patients with congenital heart disease. During this period, improvements in surgical and medical treatments have been accompanied by developments in a spectrum of diagnostic modalities. Integration of different modalities in clinical and research environments is being used for better understanding and better managing of complex cardiac conditions.
Ideally, few noninvasive imaging modalities should be able to delineate all aspects of the anatomy and evaluate physiologic consequences of the lesion(s) in patients with congenital heart disease. Moreover, the imaging modalities used should be cost effective and portable, not cause excessive discomfort and morbidity, and not expose patients to harmful effects of ionizing radiation. To limit the number of imaging modalities used in diagnosis and therapy, research is being performed to evaluate and validate techniques that could potentially serve as noninvasive or minimally invasive imaging modalities that would replace those which are invasive and less available.
Challenges of AVSD
Appropriate diagnosis and detailed assessment of the anatomic and functional features of AVSD presents challenges. Particularly, accurate preoperative assessment of the atrioventricular valve component is crucial since long-term outcomes for surgical repairs of AVSDs depend on the successful repair of the left atrioventricular valve. Moreover, surgical destruction of the conduction system may occur in cases of inappropriate diagnosis because AVSDs have different conduction pathways compared with defects that have separate atrioventricular valves.1
Anatomy of AVSD
AVSD is anatomically characterized by abnormal development of the atrioventricular valve junction.2-6 In addition, the overall atrioventricular valve complex including valve leaflets and papillary muscles is abnormally developed. Figure 18–1 schematically depicts main differences in the normal (Fig. 18–1A) and primum AVSD heart (Fig. 18–1B) anatomy. Atrioventricular valve leaflets are different from normal mitral and tricuspidal leaflets because atrioventricular valve leaflets guard a common atrioventricular junction and are displaced. In addition, valve leaflets may be asymmetric, the mural leaflet may be abnormally small. Displacement and sometimes even dysfunction of the papillary muscles is present. Those changes are often associated with pre- and postoperative regurgitation of the valve.7-9 Left ventricular papillary muscles are positioned further from the septum compared with normal, with the posterior papillary muscle more so than the anterior papillary muscle.1 Thus, specifically, the posterior papillary muscle is a marker of distinction between AVSDs and other similar defects such as defects with mitral clefts.1
Figure 18–1.
Differences in anatomic characteristics between normal (A) and primum atrioventricular septal defect (AVSD) (B). Both the normal and primum AVSD hearts are first shown from modified left anterior oblique view at the level of the valves (a). The apical four-chamber view and short axis view of the heart at the level of papillary muscles are also presented (b). A, arteria; AV, atrioventricular; PMs, papillary muscles. The image was modified from Adachi I, Uemura H, McCarthy KP, et al. Surgical anatomy of atrioventricular septal defect. Asian Cardiovasc Thorac Ann. 2008;16:497-502.
Imaging of AVSD: Anatomy
Two-dimensional (2D) echocardiography (ECHO) is the current standard noninvasive imaging tool used for the morphologic and functional assessment of the AVSD and provides global preoperative data in the majority of cases.12 Figure 18–2 and the related Moving Image show the 2D image of the primum AVSD. The morphology of the defect and atrioventricular valve is presented.
Figure 18–2.
A. Anatomy of the atrioventricular septal defect (AVSD) imaged using two-dimensional echocardiographic imaging. Apical four-chamber view shows the premium AVSD defect between the atria and the common atrioventricular (AV) junction with left and right parts of the common AV valve. See also Moving Image 18–2A. B. Subcostal short axis view shows the anatomy of the left part of the atrioventricular valve. Bridging leaflets and mural leaflet are depicted. Moving Image 18–2B shows the function of the left atrioventricular valve with insufficiency through the apposition of the bridging leaflets.
Apical 4 chamber view shows the primum AVSD defect between the atria, common atrioventricular junction with left and right part of the common AV valve.
Play Video
Subcostal short axis view shows the anatomy of the left part of the atrioventricular valve. Bridging leaflets and mural leaflet are depicted.
Play Video
With advances in imaging technology, three-dimensional (3D) ECHO has been shown to primarily facilitate the accurate anatomic and functional assessment of complex spatial anatomic features and relationships of the anatomic and functional abnormalities involved in AVSD.12 3D ECHO provides more detailed information about anatomic and functional assessment of the atrioventricular valve, the relationships between the leaflets of the valves, with each other and with other heart structures.13 Figure 18–3 and the related Moving Image show an example of the assessment of the anatomy of the atrioventricular valve by using 3D ECHO imaging. Relationships between the leaflets and dynamics of the valve leaflet motion can be seen on the cine image. This anatomic information is of value for the clinician in planning surgical treatment because it provides a more detailed anatomic definition of interrelations between structures.14
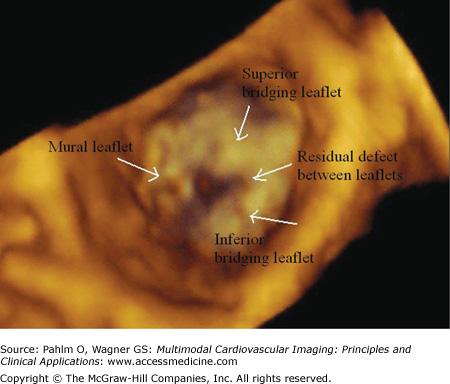
Figure 18–3.
Anatomy of the atrioventricular valve in atrioventricular septal defect (AVSD) imaged using three-dimensional echocardiography. Mural and anterior and posterior bridging leaflets are visualized. The picture is taken after suturing of the bridging leaflets. Residual defect is seen between the bridging leaflets. See also Moving Image 18–3.
Anatomy of the atrioventricular valve in AVSD by using 3D ECHO imaging.
Play Video
The atrioventricular valve apparatus consists of the annulus, leaflets, chordae, and papillary muscles. Because the atrioventricular valve apparatus is complex, 2D ECHO is often not sufficient to provide full information of the atrioventricular valve relationships. Real-time 3D imaging permits display of the entire circumference of the atrioventricular annulus. This is important information in surgical repair of the valves (eg, annuloplasty). Whereas 2D imaging shows the edges of the leaflets in multiple different views, real-time 3D imaging shows the entire surface of the leaflet in a single display. Leaflets can be inspected from either the atrial side or the ventricular side, depicting, for example, buckling, cleft, or deficiencies. The advantage is that all of the information can be obtained from a single data set without the need to scan and sweep from different windows, as is required in 2D imaging.15 3D ECHO provides new insight into the dynamic morphology of the left-sided atrioventricular valve and left ventricular outflow tract anatomy.16,17 In the clinical scenario, it clarifies the pathology, particularly in complex lesions where the incremental information has an impact on therapeutic decision making.
Morbidity of the left atrioventricular valve remains an important concern.18-20 Reoperation of valve failure is complex and involves annular reduction, commissurotomy, closure of the residual defect in the apposition of the bridging leaflets, and patch enlargement of the atrioventricular valve. Although the surgeon has the opportunity to inspect the atrioventricular valve and test its competency with saline, this latter technique is nonphysiologic and might provide an incomplete evaluation of the true nature of the valve failure. 2D ECHO with color Doppler scanning is the current standard for both preoperative and postoperative assessment of patients with AVSD. Figure 18–4 and the related Moving Image show the color Doppler ECHO used for assessment of the function of the atrioventricular valve. The limitation of the 2D perspective is its difficulty to provide details regarding the status of the commissures, the precise location of the regurgitant jets, sites of poor coaptation, and the presence of clefts. Color Doppler scanning is a helpful adjunct, but the true extent and location of the regurgitant jets might be difficult to appreciate in a 2D image, particularly in cases with multiple jets caused by the phenomena of jet entrainment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree