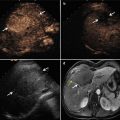
Fig. 29.1
Images in a 58-year-old man who underwent contrast-enhanced ultrasound (CEUS) guidance microwave ablation (MWA) of hepatocellular carcinoma (HCC). (a) Contrast-enhanced computed tomography (CT) shows a local nodule (arrows) in the right hepatic lobe. (b) Conventional ultrasound could not detect the tumor, but the CEUS arterial phase image shows a 2.1 ×1.6 cm tumor in the right hepatic lobe (arrow). (c) Arterial phase of contrast-enhanced magnetic resonance imaging (MRI) obtained 3 months after MWA shows complete necrosis of the tumor (arrow). (d) Arterial phase of CEUS obtained 3 months after MWA shows complete necrosis of the tumor (arrow)

Fig. 29.2
Images in a 50-year-old man who underwent CEUS guidance MWA of HCC. (a) Contrast-enhanced MRI shows a local nodule (arrow) in the left hepatic lobe. (b) Conventional ultrasound could not detect the tumor, but the CEUS arterial phase image shows a 2.1 × 1.4 cm tumor in the left hepatic lobe (arrow). (c) Arterial phase of contrast-enhanced MRI obtained 6 months after MWA shows complete necrosis of the tumor (arrow). (d) Arterial phase of CEUS obtained 6 months after MWA shows complete necrosis of the tumor (arrow)

Fig. 29.3
Images in a 56-year-old man who underwent CEUS guidance MWA with a 2.4 × 2.3 cm local residual lesion of HCC after TACE. (a) Contrast-enhanced CT shows a local residual lesion in the right hepatic lobe after TACE (arrow). (b) Conventional US could not detect the tumor, but the CEUS shows arterial phase adjacent to the TACE zone indicative of local residual lesion (arrow). And MWA was inserted along the guideline under CEUS guidance (arrow). (c) Arterial phase of contrast-enhanced MRI obtained 3 months after MWA shows complete necrosis of the local residual lesion (arrow). (d) Arterial phase of CEUS obtained 3 months after MWA shows complete necrosis of the local residual lesion (arrow)
With CEUS guidance, the tumor is localized, and microwave antennas are placed directly into the tumor. During MWA, the hyperechoic area of ablation is usually monitored using gray-scale sonography. The treatment session will be ended if the transient hyperechoic zone between antennas on gray-scale US merges and covers the target region. After ablation, every patient receives CEUS to evaluate treatment response. Successful treatment is defined when no focal and/or irregular enhancement within the treated lesion during the dynamic study is detected, whereas treatment failure is defined by the presence of nodular enhancement in arterial phase and washout in late vascular phase within the treated lesion.
29.4 Effect of CEUS in Guiding Ablation
MWA with CEUS guidance has demonstrated the potential to dramatically broaden the scope of US diagnosis of hepatic tumors [17, 18] and decrease the number of sessions required for ablation of HCC in difficult cases [19]. Masuzaki et al. [20] reported in a large-scale study that the detectability of tumor nodules was 83.5 % in conventional US and 93.2 % in contrast-enhanced US (P = 0.04). In a randomized controlled study [21], the number of treatment sessions was significantly lower in the contrast harmonic US group (mean, 1.1 ± 0.2 vs. 1.4 ± 0.6, P = 0.037). Treatment analysis showed that the complete ablation rate after a single treatment session was significantly higher in the CEUS group than in the B-mode US group (94.7 % vs. 65.0 %, P = 0.043).
Our previous studies evaluated the efficiency and feasibility of CEUS-guided MWA for hepatocellular carcinoma inconspicuous on conventional US [22]. In that study, we performed MWA under CEUS guidance for 109 patients with 109 HCC nodules inconspicuous on conventional US. We found that CEUS-guided microwave ablation is an efficient and feasible treatment method for patients with HCC inconspicuous on conventional US.
Before its application in MWA, CEUS has been used for a long time in guiding RFA. Other studies reveal that CEUS does allow a reliable and immediate assessment of therapeutic efficacy of percutaneous RFA of malignant liver lesions [23]. Meanwhile, pretreatment evaluation with CEUS is effective for percutaneous RFA of HCCs with poor conspicuity on conventional US [24].
29.5 Comparison with Other Guiding Techniques
Besides CEUS, CT or MRI guidance can also be used for the guidance of MWA. Compared with other techniques, CEUS guidance has many advantages: (a) US equipment is smaller, which makes it more convenient to use in clinical work. (b) CEUS guidance is real time. (c) CEUS is easy to operate and allows scanning the body from different positions and angles. (d) CEUS emits no ionizing radiation. (e) CEUS is less expensive than other guiding techniques. (f) Few allergies happen during CEUS guidance. (g) The therapeutic effect can be evaluated in real time under CEUS guidance (Table 29.1).
Table 29.1
The comparison among CEUS, CT, and MRI for the guidance of MWA
Features | Guiding techniques | ||
|---|---|---|---|
CEUS | CT | MRI | |
Convenience | Yes | No | No |
Multiangle scan | Yes | No | No |
Ionizing radiation | No | Yes | No |
Expensive | No | Yes | Yes |
Allergy | Few | More | More |
Real time | Yes | No | No |
Compared to CEUS, CT and MRI have been used for a long time in guiding MWA (Table 29.2). CT has high spatial resolution, good contrast, wide field of view, good reproducibility, and applicability to bony and air-filled structures. The use of a CT-guided method can be expected to reduce the rate of local tumor progression associated with percutaneous ablation therapy. We reviewed several well-performed studies. Laspas et al. [31] reported that the ablation success rate was 87.3 % (281/322 HCC nodules), and the survival rates at 1 year, 3 years, and 5 years were 94.8, 73.1, and 51.1 %, respectively. Despite the advantages of CT, there are several limitations such as the increased time that is necessary for the procedure and exposure of the patient to ionizing radiation.
Table 29.2
Ablation treatment results of HCC patients under different guiding techniques
Author | Guiding technique | No. of patient | Size (cm) | Technique effectiveness rate (%) | Locoregional recurrence rate (%) | 1-year survival rate (%) | 2-year survival rate (%) | 3-year survival rate (%) | Mean follow-up (month) |
|---|---|---|---|---|---|---|---|---|---|
Dong et al. [3] | CEUS | 234 | 4.1 | 93 | 31 | 92.70 | 81.60 | 72.85 | 27.9 |
Liang et al. [25] | CEUS | 288 | 3.75 | 91 | 35
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|