Chapter 5 Coronary artery disease
Coronary artery disease
Non-invasive imaging has become a valuable method for cardiovascular assessment in atherosclerotic coronary artery disease. It plays a crucial role in:
 the initial detection of coronary artery disease
the initial detection of coronary artery disease
 determining prognosis
determining prognosis
 therapeutic decision-making.
therapeutic decision-making.
A range of techniques using stress protocols are now available to assess myocardial ischaemia or viability in patients with coronary artery disease.
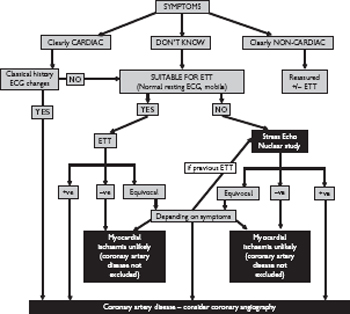
Basic investigations
Careful clinical assessment is an essential prerequisite to the imaging of coronary artery disease (Fig. 5.1). Setting the pre-test probability of a patient having ischaemic heart disease is useful for determining which test is most appropriate, or indeed whether it is appropriate to proceed to non-invasive imaging.
A detailed history for classic symptoms of angina and risk factors, along with a baseline ECG may provide the necessary information to diagnose coronary artery disease. The ECG may also determine which imaging technique is most appropriate and whether there is other unexpected pathology. Baseline blood tests may be important prior to invasive coronary imaging to identify issues such as pre-existing renal dysfunction and anaemia which affect procedural risk and may require investigation before imaging is performed. Assessment of troponin levels is essential in the patient with acute presentation to give a guide to the presence and severity of myocardial infraction.
Cardiovascular imaging
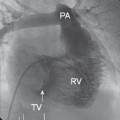
 Direct coronary imaging with angiography may be indicated in patients with stable angina to allow identification of prognostically important coronary disease (such as triple-vessel disease or disease of the left main-stem). Such patients may benefit prognostically from surgical revascularization. Other patients with stable symptoms may undergo invasive coronary imaging with a view to potential revascularization on symptomatic grounds or non invasive coronary imaging with cardiac CT may be appropriate.
Direct coronary imaging with angiography may be indicated in patients with stable angina to allow identification of prognostically important coronary disease (such as triple-vessel disease or disease of the left main-stem). Such patients may benefit prognostically from surgical revascularization. Other patients with stable symptoms may undergo invasive coronary imaging with a view to potential revascularization on symptomatic grounds or non invasive coronary imaging with cardiac CT may be appropriate.
 In other situations a functional assessment of the extent of inducible myocardial ischaemia is warranted to provide further information on diagnosis and prognosis without the need for invasive investigation or exposure to ionizing radiation and other risks of angiography.
In other situations a functional assessment of the extent of inducible myocardial ischaemia is warranted to provide further information on diagnosis and prognosis without the need for invasive investigation or exposure to ionizing radiation and other risks of angiography.
 Imaging in patients who have had acute coronary events or myocardial infarction is usually performed:
Imaging in patients who have had acute coronary events or myocardial infarction is usually performed:
• to confirm or exclude a clinical diagnosis of atheromatous coronary disease, often as a prerequisite to appropriate revascularization by either percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG)—echocardiography, coronary angiography
• to determine the extent of disease and damage to the myocardium and the viability of the myocardium for longer-term management—echocardiography, CMR.
Fig. 5.1 Schematic diagram demonstrating an approach to the management of a patient with suspected coronary artery disease based on symptoms, coronary angiography, and non-invasive imaging. In practice, the choice of non-invasive imaging is largely dependent on local expertise and availability. ETT, exercise tolerance test.
Myocardial ischaemia
The rationale for stress protocols in coronary artery disease is to look for evidence of myocardial ischaemia to aid diagnosis of coronary disease and decide on how to manage the patient i.e. need for revascularization or medical therapy. Ischaemia is identified as a relative reduction in myocardial blood flow on stress sufficient to cause a decrease in myocardial perfusion or contraction. In a normal subject, coronary and myocardial blood flow increases three- to fourfold during stress to match increased myocardial oxygen demand. This can occur because myocardial arteriolar resistance reduces. If there is a coronary stenosis, the arteriolar resistance is already reduced at rest to preserve coronary blood flow. Therefore at rest severe occlusions do not result in wall motion abnormalities, but on stress the blood flow cannot be increased further and the myocardial oxygen delivery is reduced. The more severe the stenosis, the smaller is the possible increase in coronary blood flow and the earlier wall motion abnormalities occur.
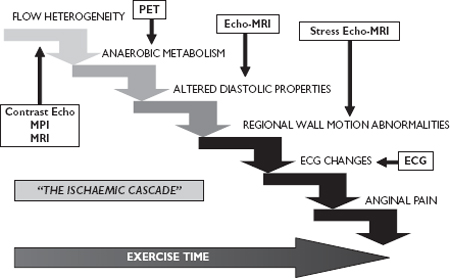
Ischaemic cascade: wall motion and perfusion
The ischaemic cascade suggests that perfusion changes occur before regional wall motion abnormalities, which occur before ECG changes, which occur before angina (Fig. 5.2). Therefore techniques which image perfusion may be more sensitive than those relying on regional wall motion abnormalities. In practice the transition through the ischaemic cascade is often quite rapid so that the patient develops perfusion changes, wall motion abnormalities, and angina at a certain ‘tipping point’ in their stress protocol.
Which technique for ischaemia assessment
Non-invasive imaging techniques have similar sensitivity and specificity for assessment of ischaemia so the choice of test often depends on local availability and expertise. The indications for stress echo-cardiography widely overlap with the indications for myocardial scintigraphy and stress CMR.
There are clinical situations where myocardial scintigraphy is relatively contraindicated (left bundle branch block, bifascicular block, and ventricular paced rhythms). In these situations dynamic exercise leads to perfusion abnormalities of the septum and adjacent walls in the absence of obstructive coronary disease. If there is local expertise, stress echocardiography is an option.
For assessment of viability/hibernation stress echocardiography and myocardial perfusion imaging are joined by MRI and PET. All are potential methods and currently there is no consensus as to whether one of these methods is superior. The decision depends on local availability and expertise.
Fig. 5.2 The ‘ischaemic cascade’ with superimposed imaging modalities positioned to demonstrate the different aspects of developing ischaemia that they are optimized to identify.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree