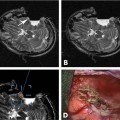
25 Over the past two decades, there have been significant advances in intraoperative MRI-guided (iMRI) neurosurgical applications. The first dedicated open interventional MRI system was developed at Brigham and Women’s Hospital during the mid-1980s. In 1996, the first intraoperative MRI-guided craniotomy was reported by the University Hospital in Heidelberg.1 The first neurosurgical operation in a dedicated 3.0 tesla (T) MRI suite was performed at the University of Minnesota,2 which also performed magnetic resonance spectroscopy (MRS) and functional MRI (fMRI) immediately prior to craniotomy.3 MRI-guided neurosurgical procedures now include stereotactic biopsy and resection of brain tumors, placement of deep brain stimulating electrodes, targeted drug and cell delivery, and various other procedures where localization of a probe, implant, or target structure is critical to the outcome.4–6 MRI is generally well suited for such neurosurgical interventions because the submillimeter spatial resolution available in multiple projections allows the clinician to determine the optimal surgical trajectory, to avoid critical neural structures, and to evaluate the status and efficacy of the procedure intraoperatively.7–9 MRI has an additional advantage over computed tomography (CT) because there is no radiation exposure to the patient or health care personnel. At the same time, the use of iMRI guidance has added several challenges to the already complex neurosurgery operating room (OR). The use of iMRI alters the surgical working environment and affects various diagnostic and surgical protocols and procedures in many ways. For example, sterile draping of the patient has to be modified, communications between OR personnel can be difficult because of noise from the scanner, and specialized MRI-compatible surgical instruments are often required because of the large magnetic fields and gradients produced by the scanner.10,11 As iMRI-guided procedures gain increasing acceptance in the neurosurgical community, medical centers around the world have launched evaluations of their investments in interventional MRI suites. Multiple interested parties, including insurance companies, hospital administrators, physicians, patient advocacy groups, and government representatives have become active participants in the ongoing debate about the cost effectiveness of MRI-guided interventions. However, to date, only a few studies have provided comparisons of the financial costs and clinical benefits of iMRI guidance relative to procedures performed in a conventional OR in terms of patient length of stay, hospital charges and costs, net health outcome, and other technology assessment criteria now generally demanded by managed care organizations, third-party coverage agencies, hospital administrations, and the relevant regulatory entities. In this chapter we summarize the available data on the cost efficacy of iMRI-guided neurosurgery and discuss the potential future role of iMRI guidance in the diagnosis and management of various neurologic diseases and disorders. In the modern managed care environment, medical and surgical treatments are increasingly being subjected to evaluations of economic efficiency. A conventional cost-effectiveness analysis essentially measures the cost of a medical technology per unit of a defined health output. Such an analysis is useful for directly comparing competing medical treatments and enabling them to be ranked based on economic efficiency.12 Components of a cost-effectiveness analysis typically include the costs of the procedure, the use of discounting for both costs and benefits, an appropriate viewpoint of the analysis, and a sensitivity analysis of the assumptions and probabilities that drive the analysis and underlie the results. The cost of adding an iMRI system to a hospital must also take into account its benefits to physician users, its ability to improve patient clinical outcome, and its capacity to favorably impact other hospital costs, including those associated with risk management. Cost-benefit analysis can be further complicated if an interventional MRI unit is purchased for multipurpose use, including diagnostic MRI, MRI-guided interventions, as well as iMRI-guided neurosurgery. At many hospitals and medical centers, multipurpose use of interventional MRI is in fact mandated as a practical economic requirement because MRI-guided neurosurgery is still performed relatively infrequently. Consideration of such detailed information is necessary to objectively evaluate whether iMRI-guidance is cost effective (particularly in terms of capital equipment expenses, suite constructions and renovations, and the associated personnel and maintenance costs). iMRI-guided systems were developed initially to facilitate safer and more effective neurosurgical procedures for brain biopsy and tumor resection. MRI guidance generally enables the neurosurgeon to take into account brain-shift after opening the skull, to more accurately localize the lesion to be resected, to determine the full extent of the lesion, and to establish a safe surgical approach to the lesion with reduced operative morbidity. However, with both frame-based and frameless neuronavigational systems, the radiologic images obtained before surgery do not necessarily provide the surgeon with information during the actual surgery that reflects the dynamic changes in the operative lesion and surrounding structures, especially brain-shift. During stereotactic brain biopsies, shift of the target by 5 mm or more has been reported,13 which can result in significant loss of navigational accuracy. Many neurosurgical procedures have a very small margin for anatomic error, which has led to the development of several Food and Drug Administration-approved stereotactic computer-assisted guidance systems for various procedures. Successful biopsy rates of 80 to 99% have been reported in recent studies of stereotactic biopsy procedures aided by iMRI guidance.6 Bernays et al14 obtained a histologic yield of 100% and a diagnostic yield of 97.4% in 114 consecutive frameless stereotactic biopsy procedures with iMRI guidance. Brain-shift was detected in 45% of the patients. Six complications, including one death and one case of a new neurologic deficit, were reported. An early cost-effectiveness analysis of stereotactic radiosurgery versus resection for patients with solitary metastatic brain tumors revealed a lower uncomplicated procedure cost ($20,209 versus $27,587), a lower average complication cost per case ($2,534 versus $2,874), a lower total cost per procedure ($22,743 versus $30,461), a better overall cost effectiveness ($24,811 versus $32,149 per life year), and a better incremental cost effectiveness ($40,648 versus $52,384 per life year) for radiosurgery than for surgical resection.15 However, controversy remains regarding the relative efficacy of radiosurgery in comparison to open surgery for metastatic disease, adding further complexity to attempts at comparing the two management alternatives. Another early study that analyzed the cost effectiveness of anterior temporal lobectomy for intractable temporal lobe epilepsy found that surgery provided an average of 1.1 additional quality-adjusted life years (QALYs) compared with continued medical management at an additional cost of $29,800.16 Anterior temporal lobectomy yielded a cost-effectiveness ratio of $27,200 per QALY, which was comparable to various high-volume therapeutic procedures such as total knee arthroplasty ($16,700/QALY) or coronary artery balloon arthroplasty ($40,800/QALY).16 An evaluative study performed at the University of Minnesota17 compared the financial costs and clinical benefits of brain tumor resection performed in an interventional MRI suite compared with a conventional operating room (OR). To evaluate the comparative cost efficacy, financial data for 51 tumors resected under iMRI were compared with conventional OR data. Eighteen patients had a first brain tumor resection and another 29 patients underwent 33 tumor resections for recurrent disease. The iMRI data were analyzed together with 35 pediatric and 118 adult tumor resections performed in the OR. Comparisons were made for adults and children for length of stay, hospital charges and payments, hospital total direct and indirect costs, readmission rates, repeat resection interval, and net health outcome. For adults, the length of stay associated with iMRI-guided surgery (3.7 days) was significantly shorter than for conventional OR surgery (8.2 days) for first resections. iMRI hospital charges were 12.2% lower ($4,063) for first resections and 4.1% lower ($922) for repeat resections than for OR surgery. Total MRI suite hospital costs associated with iMRI-guided procedures were 14.4% lower ($3,415) than for OR surgery for first resections and 3.3% lower ($723) than costs for repeat resections. Cost-to-charge ratio for first resections was 69.6% for iMRI procedures and 71.4% for OR procedures, but was not different for repeat resections. For children, the length of stay associated with iMRI-guided surgery (4.5 days) was significantly shorter than for OR surgery (14.1 days) for first resections, as well as for repeat resections (8.0 days vs 13.3 days, respectively). Hospital charges associated with iMRI-guided surgery were significantly lower than for OR surgery for both first resections and repeat resections. The iMRI-guided surgery costs were also significantly lower for first resections and repeat resections compared with OR surgery. Operative morbidity and mortality were not different with use of the iMRI procedures. Notably, no repeat resections followed iMRI surgery, whereas the OR repeat resection rate was 20% (adults) and 30% (children). The mean time from iMRI-guided surgery was 11.3 months (adults) and 18.0 months (children). For OR surgery, the mean time to repeat resection rate was 9.3 months (adults) and 13.3 months (children). The results of the University of Minnesota study17 provided some early evidence that iMRI-guided surgery can improve net health outcomes in terms of reduced hospital length of stay, reduced resection rate, and reduced hospital charges and costs. The length of stay for iMRI-patients was 31 to 68% lower compared with that of brain tumor patients undergoing resection in the OR. Hospital charges were 3 to 44% lower for iMRI-patients than for OR patients. Costs for iMRI-resection admissions were 3 to 46% lower for iMRI patients compared with OR patients. Patients that had iMRI-guided surgery were also found to have a lower repeat tumor resection rate after the initial resection or subsequent resections. Interpretation of the Minnesota study results is limited by the fact that the data was not obtained from a randomized, controlled trial. Nonetheless, the results do suggest that compared with conventional OR surgery, iMRI-guided surgery can reduce hospitalization length of stay, associated hospital charges, and repeat resection rate. Moreover, although neurosurgery for brain tumor resection performed in a conventional OR generally has a 20 to 50% repeat resection rate within one year, the Minnesota results found that iMRI-guided neurosurgery can have a much lower repeat resection rate during a comparable period. Several studies have demonstrated that iMRI-guidance improves the extent of tumor resection for both low-grade and high-grade gliomas.18–25 Most of these studies found no differences in outcome between the use of high-field versus low-field MRI guidance, although there are two reports that high-field iMRI-guidance led to a significant improvement in the extent of tumor resection compared with low-field MRI.20,26 Survival studies suggest that iMRI can usefully guide total surgical resection of gliomas. The risk of low-grade glioma recurrence during a median follow-up of 3 years was found to be 1.4 times higher for patients who underwent subtotal resection, and the risk of death was 4.9fold higher compared with patients who underwent gross total resection.27 Wirtz et al25 found that the mean survival time for patients with glioblastoma multiforme was 15.7 months for patients without residual tumor, which was an 83% improvement over the 8.6-month survival time for patients with residual tumor. However, not all studies have found benefits associated with iMRI-guidance for surgical treatment of gliomas. Hirschberg et al,28 for example, reported that although iMRI guidance can improve imaging of residual grade IV gliomas, it did not increase the efficacy of surgery or reduce the complication rate in patients compared with more conventional neurosurgery. The benefits of iMRI guidance for resection of nonglioma intracranial tumors have been mixed. Gralla et al29 reported that in 26 patients with supratentorial cavernomas, there was no difference in extent of tumor resection between patients undergoing iMRI-guided surgery versus conventional neurosurgery. In another study of 21 patients undergoing resection of craniopharyngiomas, iMRI-guidance (0.2 T) facilitated monitoring of cyst puncture and aspiration and complete resection, but did not exclude recurrence of the tumor.30 Yrjana et al31 recently reported their 7-year experience with 160 craniotomies in an operating theater equipped with a 0.23 T MRI scanner, which could be turned on and off during surgery. The tumors undergoing iMRI-guided resection included 87 low-grade and high-grade gliomas, 16 meningiomas, 13 benign tumors, along with various histologically miscellaneous subgroups. The authors of this study concluded that for many patients conventional neurosurgery, possibly aided by neuronavigation, offers benefits comparable to iMRI-guided surgery. However, Yrjana et al also found that for some patients with deep-seated tumors, or with tumors in critical locations, prognosis may be significantly enhanced by iMRI-guidance. The impact of iMRI on surgical outcomes has also been evaluated in studies in which imaging updates were used during the procedure to see if further surgery was necessary. Measurements of usage rate or frequency (the percentage of procedures in which the surgeon decided to use intraoperative imaging) ranged from 17.5 to 73.6% in three studies reporting on 309 procedures.32–34 Among 419 tumor resection procedures where iMRI was available, further resection based on updated imaging was beneficially performed in 14.8 to 63.4% of cases. In a recent analysis of the impact of iMRI on health care costs, outcomes were compared in 102 patients who had undergone intracranial tumor resection with the use of preoperative and postoperative MRI alone versus 160 patients that underwent tumor resection with iMRI guidance.35 Mean total costs, OR costs, and intensive care unit (ICU) costs were not significantly different between the two groups, although, importantly, length of hospital stay was reduced in glioma patients that had tumor resection with iMRI-guidance. Lycette et al36 compared hospital charges for iMRI-guided surgery with standard neurosurgery for 18 patients with glial neoplasms who underwent craniotomies. The iMRI group had an average operation time of 9.9 hours with an associated hospital charge of $8,840 and average material costs of $17,180. The standard OR group had an average operation time of 6.3 hours, hospital charge of $4,390, and material costs of $16,900. The majority of the cost difference between the two groups was attributable to the longer operation time for the iMRI group for which the hospital charged an hourly rate. The impact of neuronavigation without iMRI update on surgical resection of brain tumors has also been evaluated in several studies.37–41 These studies reported rates of 81.2 to 100% total removal of lesions. Extent of resection was confirmed with operative MRI or computed tomography (CT) within 48 hours of the surgical procedure. Three additional studies involved biopsies of cranial tumors with a combined sample size of 258 patients. Diagnostic accuracy, defined as the percentage of intraoperative smear diagnoses later corroborated by definitive histologic study, ranged from 87 to 96%.42,43 Medical and surgical complication rates ranged from 8.8 to 14%. In a prospective nonrandomized study, Dorward et al42 compared 76 frameless procedures with 79 frame-based procedures, all without intraoperative imaging updates. Histopathologic results and the accuracy of smear diagnosis were comparable in the two groups. The frame-based group had a complication rate of 22%, significantly higher than the 14% complication rate in the frameless group. Germano et al40 reported a mean of 7.5 days hospital length of stay when neuronavigation without imaging update was used for surgical resection of tumors, versus 10.8 days in patients undergoing conventional surgery, a more than 30% difference. The standard treatment for glioblastoma remains biopsy and resection followed by radiotherapy and, in some cases, systemic chemotherapy. However, newer therapies, including local chemotherapy using implantable biodegradable polymers, immunotherapy, gene therapy, and anti-angiogenic agents, are under active, ongoing development.44,45
Cost and Benefit Analysis of Intraoperative MRI-Guided Neurosurgery
Analyzing Cost Effectiveness
MRI-Guided Brain Biopsy and Tumor Resection
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree