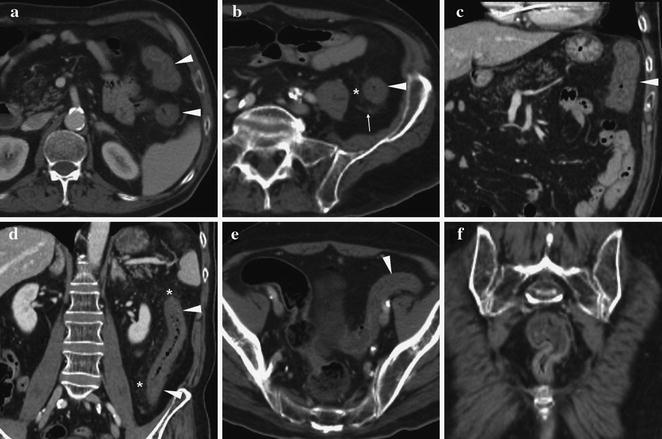
Fig. 7.1
48-year-old male with multifocal ileo-colic Crohn’s disease. Water enema multidetector CT including multiplanar image reformations shows short non-distensible bowel segments with stratified mural thickening involving the splenic flexure (arrows in a and b), descending colon (arrowheads in b and c) and distal ileum (thin arrows in c and d)
Both chronic IBD conditions involve a significant degree of colon mural thickening, which is usually more pronounced in CD (mean 11 mm) than in UC (7−8 mm). Furthermore, wall thickening in UC is symmetric and continuous, whereas in granulomatous CD colitis it usually appears eccentric or asymmetric, with segmental distribution and spared “skip” tracts (Fig. 7.1) [2, 6, 7].
The thickened colon wall in IBD usually demonstrates a stratified pattern. The “target” or “water halo” sign refers to a triple-layered appearance of the bowel when seen in a plane perpendicular to its main axis, with an outer soft-tissue ring representing the muscularis mucosa and serosa, a middle ring of intermediate density caused by the thickened oedematous submucosa and an inner ring of enhancing, inflamed mucosa (Fig. 7.2). Although unspecific, this CT sign is invariably associated with acute bowel injury (usually from an infectious or inflammatory cause), and virtually excludes malignancy [2].


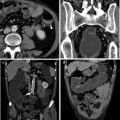
Fig. 7.2
Urgent contrast-enhanced MDCT (a, b) in a 65-year-old woman with clinical suspicion of acute diverticulitis shows extensive involvement of the descending colon by circumferential mural thickening with “target sign” stratification due to oedematous submucosa, consistent with acute infectious colitis. In another 50-year-old male patient with known chronic ulcerative colitis, the rectum (c) shows mural stratification with “fat halo” sign corresponding to submucosal adipose deposition, associated with mesorectal fat proliferation
The water halo sign should be differentiated from the “fat halo” sign, which is seen more often (61 %) in patients with UC, than in CD colitis (8 %). The thickened bowel wall demonstrates three layers with different CT density: the inner soft-tissue attenuation layer represents the enhancing mucosa, the intermediate fat-density (-65 Hounsfield Units (HU) to -10 HU) layer results from widening and fatty infiltration of the submucosa, and the outer soft-tissue layer corresponds to the muscularis propria and serosa (Fig. 7.2). This CT sign may be observed on both unenhanced and post-contrast acquisitions because of the marked differences in tissue attenuation, and should suggest a diagnosis of IBD with fatty infiltration of the submucosa, particularly UC. Alternatively, this sign has been reported in patients undergoing cytoreductive chemotherapy and in graft-versus-host disease [6–8].
Other helpful features to distinguish UC from CD colitis involve the pericolonic structures. In UC, proliferation of perirectal fat is frequently observed, with a slightly increased attenuation (10−20 HU) compared to the normal mesenteric fat, and traversed by nodular and streaky soft-tissue attenuation structures (Fig. 7.2). In CD, fibrofatty proliferation and lymphadenopathy involves the mesentery, often in an extensive way. Observed more frequently in association with CD, is the “comb sign” corresponding to tubular opacities aligned on the mesenteric side of the involved bowel segment corresponding to hypervascularity with vascular dilatation, tortuosity and wide spacing of the vasa recta, secondary to increased flow related to the acute inflammation. Finally, internal fistulas and abscess collections are relatively specific to CD [6, 7, 9].
7.2 Colonic Infections
Cross-sectional imaging appearances similar to those described in IBD may be observed in many different colonic infections, that are usually diagnosed clinically, on the basis of stool cultures and endoscopy. Significant overlap exists between the imaging appearances of most colonic infections, since they all share the common MDCT features of mural thickening, most usually with a stratified appearance due to submucosal oedema and enhanced inflamed mucosa, associated with pericolonic fat stranding and variable ascites (Figs. 7.3, 7.4) [2, 6].

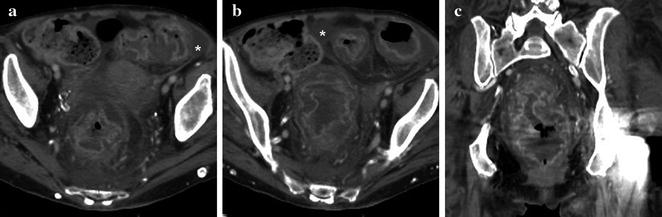

Fig. 7.3
42-year-old woman from East Europe suffering from acute febrile infectious enteritis with bloody stools. Axial (a) and coronal reformatted (b) contrast-enhanced MDCT images show mural thickening of the right colon with hyperenhancing mucosa (arrowheads), mild pericolonic inflammatory fat stranding with tiny lymph nodes
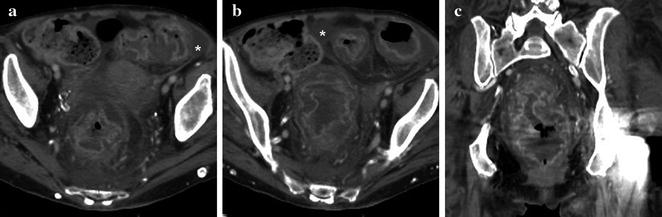
Fig. 7.4
Elderly 81-year-old woman with Clostridium difficile pseudomembranous colitis following antibiotic therapy. Axial (a, b) and coronal (c) contrast-enhanced MDCT images show severe rectosigmoid colon thickening with prominent “target sign” due to severely oedematous submucosa and strong mucosal enhancement, associated with perivisceral fat stranding and moderate ascites (*)
Sometimes, the involved causative organism may be suggested by the distribution of CT abnormalities along the colon. A diffuse (“pan-colitis”) involvement is observed with pseudomembranous colitis (PMC), cytomegalovirus and Escherichia coli infections. Resulting from Clostridium difficile overgrowth following antibiotic therapies, PMC produces the most severe degree of colon wall thickening, with prominent target/water halo appearance, associated with mild ascites and pericolonic fat infiltration (Fig. 7.4). Although insensitive, the suggestive “accordion” sign refers to positive intraluminal contrast entrapped between the thickened haustral folds [2, 6].
An ileal and right colon predominance suggests Salmonella, Yersinia, tuberculosis or amoebiasis, with the latter two conditions increasingly encountered in patients from endemic countries. Conversely, a left-sided predominance may be related to Shigella infection. Sexually transmitted infections such as gonorrhoea, herpesvirus and Chlamydia tend to involve typically the rectosigmoid. Although the distribution and mural changes in severe colonic infections such as PMC may mimic those of UC or colonic CD, the key associated findings of peritoneal effusion and pericolonic changes suggest an acute intestinal inflammation and are rather unusual in patients with chronic IBD (Fig. 7.4) [2, 6].
7.3 Ischaemic Colitis
Ischaemic colitis (IC) is increasingly encountered in the ageing Western population, and may result from a sudden loss of arterial or venous blood flow or conversely from a low-flow state such as in cardiac arrhythmias. Whereas intestinal infarction due to total vascular occlusion is a dramatic event causing severe acute abdomen and shock, non-transmural IC with reperfusion presents with minor abdominal pain and rectal bleeding and with CT features that may be easily misinterpreted as chronic IBD. IC may be diffuse or segmental, more commonly involving the left-sided colon when due to hypoperfusion (Fig. 7.5). Additionally, watershed areas of the colon such as the splenic flexure and rectosigmoid are particularly susceptible to ischaemia, because they are situated at the borders of major vascular territories. MDCT imaging shows circumferential, symmetric wall thickening with haustral fold enlargement, the target sign due to oedema or otherwise high attenuation indicating intramural haemorrhage, pericolonic stranding, fascial and/or peritoneal fluid (Fig. 7.5). Coupled with appropriate clinical history, the absent involvement of the rectum favours ischaemia over UC [2, 6].