Asymptomatic hyperuricemia
Acute arthritis
Intercritical phase
Chronic tophaceous gout
The patient may then enter the intercritical phase, an asymptomatic phase between attacks of gout. The length of this phase is variable, from months to years. During this phase, the patient may have normal blood levels of uric acid.
Chronic tophaceous gout has become less common with adequate treatment. Tophi, extracellular deposits of MSU surrounding giant cells and mononuclear cells, take many years to develop. These deposits can be within the periarticular soft tissues such as ligaments or bursa, within the joint involving the capsule, synovium, cartilage or subchondral marrow or be distant from any joint such as the helix of the ear. Uncommonly tophi may cause significant local mass effect and compress adjacent structures, e.g. carpal tunnel syndrome with compression of the median nerve or tendon rupture. Tophi, although uncommon, may calcify.
Imaging
Radiographs (Figs. 8.1, 8.2, 8.3, and 8.4)

Fig. 8.1
Periarticular tophus, magnified left 2nd MCPJ from AP radiograph of the hand demonstrating soft tissue swelling (arrows) with subtle central calcification

Fig. 8.2
An 87-year-old male with bilateral polyarticular gout of the feet. (a–c) AP radiographs of the bilateral feet demonstrating extensive chronic radiographic changes of gout with periarticular erosions, some with overhanging edges. Note the sclerosis on the osseous margins erosions. Marginal erosions, partially calcified gouty tophi and intra-osseous gout deposition with secondary bone loss (arrow)
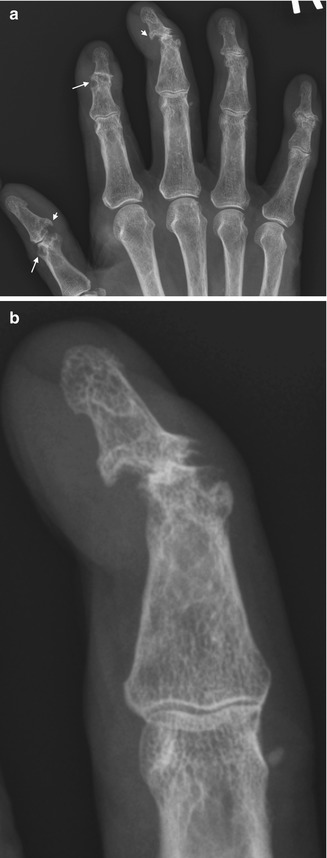
Fig. 8.3
An 80-year-old male with polyarticular gout of the hands. (a) AP radiograph, magnified, of the right hand and (b) magnified AP 3rd DIPJ demonstrating marginal erosions (small arrows) and subchondral cysts in keeping with intra-osseous gout deposition (long arrows)


Fig. 8.4
Radiographic changes of gout in different patients. (a) AP knee periarticular large erosion (arrow) of the lateral femoral condyle with overhanging edge and sclerotic margin, (b) another example of polyarticular gout, bilateral AP radiograph of the feet, (c) AP ankle with extensive central and marginal erosions, secondary degenerative change with subchondral sclerosis and joint space loss
Radiographic changes of gout are usually delayed by up to 10 years from the first clinical onset of gout. Initially gout is usually oligoarticular but may progress to an asymmetric polyarticular involvement. The lower limb is more often affected. The feet, hands, wrist, elbows and knees are the commonest joints to be involved. The first tarsometatarsal joint is involved in up to 75 % at some time during the course of the disease. The tarsometatarsal and intertarsal joints in the feet, the distal and proximal interphalangeal joints in the hand and less commonly the metacarpophalangeal joints, all compartments in the wrist, the olecranon process at the elbow, the patella, medial and lateral tibia and femur in the knee are most often involved.
Radiographic changes can be divided into early, intermediate and late. In the early stage, corresponding to acute gouty arthritis clinically, radiographs may demonstrate no bony abnormality and may show only periarticular soft tissue swelling. With progression into the intermediate phase, soft tissue tophi deposition occurs which may be visible as nodular soft tissue thickening, of slightly increased attenuation when compared to adjacent normal soft tissue. The adjacent periosteum may develop a lacelike appearance, which may progress to an erosion. Classically these extra-articular erosions have a punched-out appearance with a sclerotic margin and an overhanging edge. The sclerotic margin represents the osteoblastic response to the slowly developing erosion.
Erosions in gout may be intra-articular or para-articular or occur distant from the joint margin. Those distant from the joint are as described above. Articular erosions start marginally and progress centrally, whereas para-articular erosions are usually deep to soft tissue tophus.
Joint space is maintained in the early and intermediate stages of the disease. Bone density is normal although in acute attacks there may be associated mild periarticular osteopenia. Reactive new bone proliferation may cause localised bone enlargement or mushrooming. Subchondral tophi are seen as lucent relatively well-defined foci. Because of the reabsorption of supporting trabeculae, the bone is weakened in these areas, and osteochondral compressions, essentially collapse of the overlying cortical bone into subchondral tophi, can occur. In the late radiographic stage, which is now rarely seen, the soft tissue tophi become confluent and calcify, and joint space is lost with secondary degenerative changes developing. Progressive tapering deformities of the phalangeal shafts may develop. Rarely joint subluxation or ankylosis may occur.
A modified Sharp/van der Heijde scoring method for rheumatoid arthritis was developed as a radiographic damage index in chronic gout. This scoring system assesses erosions and joint space narrowing in the hands and feet, including the distal interphalangeal joints, and is able to discriminate between early and late disease. In addition it strongly correlates with hand function.
Ultrasound (Fig. 8.5)
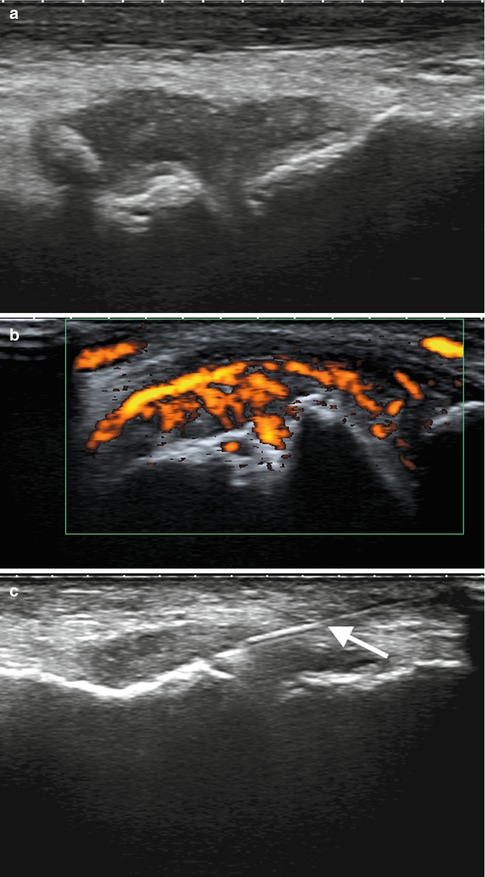
Fig. 8.5
Ultrasound gout of a 50-year-old male presenting with acute left 1st MTPJ pain, swelling and erythema, (a) longitudinal ultrasound demonstrating joint distension with soft tissue and minute hyperechoic foci within and underlying cortical irregularity, (b) with colour Doppler demonstrating marked internal flow and (c) ultrasound-guided aspiration with linear hyperechoic needle (arrow)
Ultrasound has a role in acute gout, intercritical periods, chronic tophaceous gout and asymptomatic hyperuricemia. Ultrasound has significant advantages over radiographs as it can identify pathology before radiographic changes. MSU crystals can be identified within both soft tissues and joints. Crystals, as described above, may aggregate in tendons, ligaments, bursae, soft tissues, synovium, cartilage and bone. MSU crystals deposit on the surface of cartilage and can be identified as a linear hyperechoic (bright) contour upon the normal underlying hypoechoic (dark) cartilage forming the “double contour sign”; CPPD crystals deposit within the substance of the cartilage and can thus be differentiated.
Synovial deposition, where MSU crystals are deposited within the synovial lining, incites an acute synovitis. The thickened synovium may have a heterogeneous appearance with hyperechoic micro-foci within representing the crystals. Intra-articular tophi appear hyperechoic with a surrounding hypoechoic rim or halo of inflammatory cells. Extra-articular tophus has a similar imaging appearance. Occasionally calcification may occur within the tophus, appearing hyperechoic with posterior acoustic shadowing. The tophus may be more diffuse in appearance. Erosions, focal pathological cortical disruption, should be confirmed in orthogonal planes. Erosions represent chronic disease. A tophus may be identified at the site of the erosion.
Acute gout usually presents as a monoarthritis with localised soft tissue oedema, joint effusion and acute synovitis. One should assess the synovium carefully for hyperechoic foci as described above as well as for tophi and the cartilage double contour sign. Intercritical periods and chronic gout show similar findings excluding the soft tissue oedema. There may be a low-grade chronic synovial thickening present. Tophi size and volume can be measured and may involute and disappear with therapy. Similar changes with decreased cartilage crystal deposition occur particularly if serum urate levels below 6 mg/dl can be achieved.
CT (Fig. 8.6)
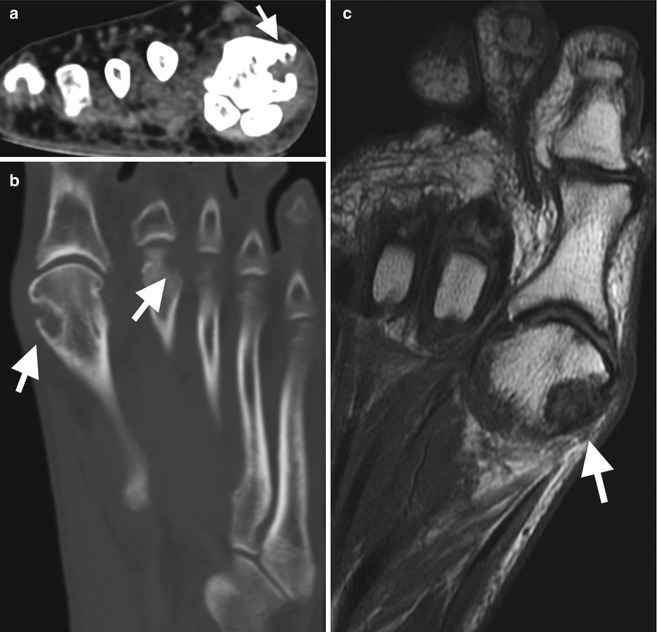
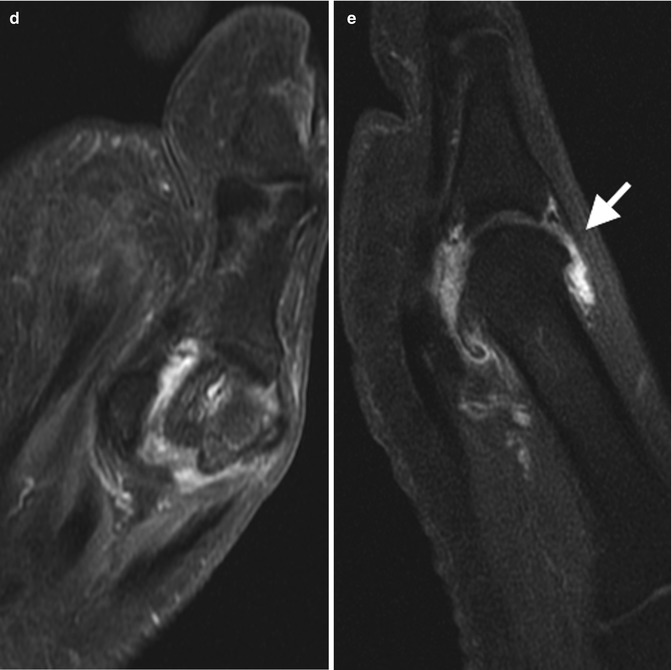
Fig. 8.6
CT and MRI gout. (a) Axial and (b) coronal reformatted unenhanced CT demonstrating erosions of the 1st and 2nd MTPJs (arrows) with sclerotic margin and overhanging edge. (c) Cor T1, (d) Cor T2FS and (e) Sag reformatted T1FS PG of the left 1st MTPJ in different patient demonstrating joint effusion with active synovitis (arrow in e) and pre-erosive change of the medial margin metatarsal head (arrow in c)
Conventional CT is excellent in demonstrating bony anatomy in fine detail and hence in the detection and measurement of erosions. CT is less efficient in evaluating the musculoskeletal soft tissues but can identify tophi from soft tissue due to their intrinsic higher attenuation. Tophi have attenuation values of approximately 170 HU, whereas soft tissues including tendon and muscle have an attenuation of 100 HU and 50 HU, respectively. Dual-energy CT (DECT) uses two x-ray tubes and detectors, exposing tissues to two different x-ray energies. Different tissues will attenuate the x-rays differently, and by assessing this difference in attenuation, the composition of tissues can be determined. Attenuation values can be assigned a colour chart, and MSU crystals can be identified with high sensitivity and specificity. DECT is most commonly used in clinical trials where the volume of MSU deposition can be assessed against different therapeutic options. DECT is at early stages of use in clinical practice and usually confined to cases with a usual clinical picture where alternate imaging has not helped. Limitations of DECT in general practice are related to limited availability DECT, related radiation exposure and the availability of nonionising imaging such as US and MRI.
MRI (Fig. 8.6)
MRI is an excellent imaging modality with the ability to image both osseous and soft tissue structures. MRI can assess both intra- and extra-articular pathology such as joint effusion, synovitis, tophus, cartilage erosion, bone marrow oedema and tendon pathology. A classical erosion and tophi are the best discriminating factors from alternate pathologies. MRI is significantly more sensitive in the detection of erosions than plain radiographs; in one study erosions were detected in 56 % of patients with normal radiographs. Typical gout erosions are as described above. In gout there is usually limited bone marrow oedema related to erosions than what can be seen in other erosive arthropathies. If extensive bone marrow oedema is present, a superimposed infection should be considered.
Tophi on MRI have a variable imaging appearance due to varying fluid and calcific composition. On T2 tophi are usually heterogeneous and of intermediate to low signal intensity but may be diffusely of high or low signal intensity. On T1 there is less variability with tophi usually of low to intermediate signal intensity. Post-gadolinium enhancement is again variable but is usually mild to moderate and homogeneous. In acute gouty arthritis, joint effusion, enhancing synovitis, bone marrow oedema and periarticular oedema can be seen, although nonspecific, but may be helpful when combined with the clinical presentation. Tophi and/or typical erosions are the most helpful in differential diagnosis.
Calcium Pyrophosphate Deposition (CPPD)
Overview
CPPD is a crystal depositional disease. CPPD crystals are deposited in articular and periarticular tissues including hyaline cartilage, fibrocartilage, synovium, ligaments and tendons. Cartilage deposition usually occurs first. The exact pathogenesis is unclear, but it is thought that crystals are deposited in susceptible individuals in areas of cartilage degeneration related to ageing or prior trauma (Table 8.2). Crystals may then accelerate degenerative changes or can be shed into the joint inciting an inflammatory response. Both men and women are affected equally. CPPD is rare under 50 years and doubles every decade thereafter. Presentation in younger patients should raise the possibility of predisposing familial or metabolic disorder. Definitive diagnosis is achieved by confirming CPP crystals in synovial fluid. On polarised light microscopy, CPP crystals are rod shaped and smaller than urate crystals and demonstrate weakly positive birefringence. It is the third commonest inflammatory arthritis and may coexist with other arthropathies in up to 25 % cases.
Table 8.2
Risk factors for CPPD
Risk factors for CPPD |
|---|
Ageing |
Osteoarthritis |
Trauma |
Haemochromatosis |
Hyperparathyroidism |
Hypomagnesaemia |
Familial |
There is considerable variation in the terminology for CPPD disease and its varied clinical presentation. The European League Against Rheumatism (EULAR) task force developed, via evidence-based recommendations, a unified terminology and diagnosis for CPPD. This forms the foundation for the approach adapted in this chapter (Table 8.3).
Table 8.3
European League Against Rheumatism (EULAR) terminology and diagnosis of CPPD
Asymptomatic CPPD | OA with CPPD | Acute CPP crystal arthritis (previously pseudogout) | Chronic CPP crystal inflammatory arthritis |
Presentation
As outlined above, CPPD may have variable clinical presentations. Occult CPPD, where the patient is asymptomatic and is discovered incidentally, is likely the commonest. Chondrocalcinosis with or without osteoarthritis may be identified on radiographs. CPPD may present with features of osteoarthritis with a recurring low-grade inflammatory component. Acute CPP arthritis, previously termed pseudogout, presents nonspecifically as an acute onset self-limiting arthritis with swelling, pain, tenderness and effusion. The differential diagnosis at presentation includes gout and infection. Chronic CPP inflammatory arthritis usually presents as a chronic oligoarthritis with low-grade chronic inflammation and may have a superimposed acute arthritis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree