Fig. 1 a–d.
Patient with a fracture of Th12 and consecutive cage interposition. a Coronal single photon emission computed tomography/computed tomography (SPECT/CT), b coronal CT. There is slight activity at the left lateral osseous bridge between Th12 and L1 indicating noncomplete bridging. c Coronal SPECT/CT, d axial SPECT/CT. There is additional uptake in the right facet joint of L2/3, indicating infrafusional activated arthrosis. SPECT/CT shows a higher degree of activation compared with CT, where there is no major difference morphologically concerning the degree of arthrosis (for color reproduction see p 314)
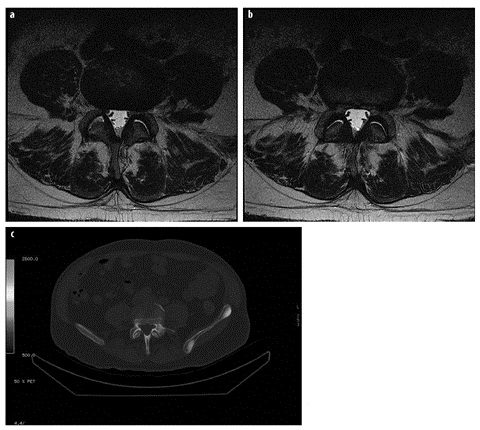
Fig. 2 a–c.
a, b Axial T2 magnetic resonance imaging of the L4/5 facet joints shows slight arthrotic changes in both facet joints, with synovial thickening, slight bony irregularities and minimal fluid. c The corresponding axial single photon emission computed tomography/computed tomography (SPECT/CT) shows no activation (for color reproduction see p 315)
Pelvis/Hip
There are clear differences, as well as some overlap, concerning MRI and SPECT/CT in pelvic and hip degenerations. MRI is mainly used for evaluation of the cartilage of the acetabulum and femoral head, for the evaluation of femoral acetabular impingements, as well as for the evaluation of the surrounding soft tissue structures. Enthesiopathies of the gluteal muscles attached to the greater trochanter, as well as evaluation of avascular necrosis (AVN) of the femoral head, especially in the pediatric population, are shown well by MRI. SPEC/CT can show some information about AVN, but the main indication for SPECT and SPECT/CT is degenerative osteoarthritis and prosthesis evaluation. However, there are studies indicating that SPECT/CT can also be used to assess viability of the femoral head. In a study by McMahon et al., the usefulness of SPECT/CT after Birmingham hip resurfacing was evaluated [8]. After the procedure, all study patients fell into category N (normal) (i.e., activity with the Birmingham prosthesis was 60–85% of activity shown with the normal contralateral femoral head). This was interpreted as preserved vascularity. Also in three patients with preoperative segmental AVN, scans were evaluated as category N (normal). There was no visual evidence of AVN of the femoral head during the average follow-up of 26 months. Thus, SPECT was able to show the preserved intra-osseous blood supply, probably based on the metaphyseal vessels in these arthritic hips. This important ability of SPECT/CT has also been shown in experimental studies in which stepwise artificial damage was inflicted on the structure supplying blood to the femoral head and neck. As a result, SPECT/CT identified the group in which the femoral head turned avascular and necrotic. The decrease in perfusion after the operation and the return to normal supply levels were also monitored. Thus, SPECT/CT was able to assess the perfusion of the femoral head semiquantitatively, which might be useful in predicting the development of traumatic AVN [9]. However, there are experimentally and clinically established techniques in MRI that can show the same results as those with SPECT/CT in such patients [10]. The advantage of SPECT/CT in those patients might be that the patient has a shorter examination time (SPECT/CT can be done in 8 min). Furthermore, no research protocols are needed; the evaluation can be done within routine clinical protocols. By far the largest and most important indication is the evaluation of hip prosthesis (infection versus loosening) in patients with recurrent or ongoing pain after surgery. First, one has to determine the physiologic uptake pattern after implantation of a hip prosthesis. Generally, cemented implants can have surrounding physiological uptake up to 1 year after surgery. In uncemented implants, physiological uptake of longer than 1 year has been described as not unusual, and should not lead to an incorrect diagnosis of loosening. Early studies showed that bone scan and conventional X-ray should be evaluated in consensus, since this can increase the sensitivity in detecting prosthetic loosening (combined evaluation: sensitivity 84%, specificity 92%) [11]. When evaluating SPECT/CT in patients with suspected mechanical loosening, SPECT/CT was significantly better than planar scanning for the acetabular cup, but not for the femoral stem [12]. The advantage of current state-of-the art SPECT/CT compared with X-ray and bone scan side-by-side is of course the higher resolution, exact anatomical localization of the increased bony uptake, as well as the morphological information from CT. This additional component allows for more precise evaluation of additional causes of hip pain, e.g., periprosthetic fractures, osteolyses and heterotopic ossifications (Fig. 3). Consequently, planning of possible subsequent surgery can be determined and planned more precisely [13].
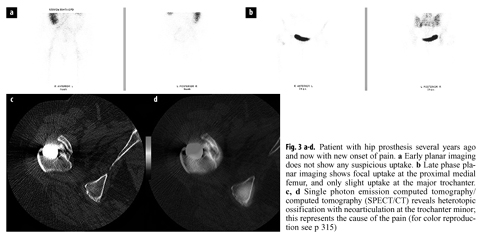
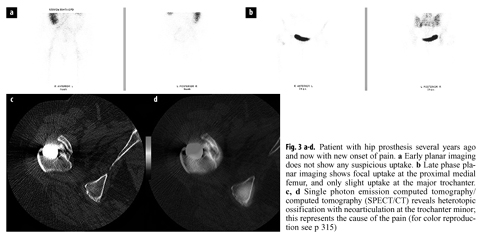
Fig. 3 a–d.
Patient with hip prosthesis several years ago and now with new onset of pain. a Early planar imaging does not show any suspicious uptake. b Late phase planar imaging shows focal uptake at the proximal medial femur, and only slight uptake at the major trochanter. c, d Single photon emission computed tomography/ computed tomography (SPECT/CT) reveals heterotopic ossification with neoarticulation at the trochanter minor; this represents the cause of the pain (for color reproduction see p 315)
Knee
MRI is the primary diagnostic modality in a wide range of indications in degenerative knee disorders. In particular, it shows soft tissue injuries such as meniscal tears, anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) (partial) tears, as well as cartilage thinning or erosions, with high sensitivity and accuracy. Diagnosis in most of the patients with these knee disorders is carried out primarily with MRI. However, SPECT/CT has a role in selected indications in knee disorders. Evaluation of (over)loading of knee compartments and subsequent correlation with the underlying cartilage conditions has been demonstrated in a study with 100 cases. A statistically very significant relationship was demonstrated between SPECT and the macroscopic cartilage condition at surgery. SPECT excluded significant chondral changes (grade II–IV) with a sensitivity rate of 97%. The sensitivity of SPECT scans in detecting severe chondral lesions was 100% (medially). Overall, a SPECT bone scan provides very useful information regarding the degree of osteoarthritis in weight-bearing compartments of the knee for pre-operative planning [14]. Similar findings have been shown in several other studies that demonstrated that pre-arthroscopic or presurgical evaluation of the degree of osteoarthritis with SPECT and SPECT/CT was reliable and helpful concerning the planning of the procedure. In particular, the medial compartment can be investigated with high accuracy. Jeer et al. described significant associations between scan findings and osteoarthritis in all compartments of the knee (P >0.05); however, the strongest association was demonstrated in the medial compartment, while the weakest association was found in the patellafemoral compartment and lateral tibial plateau. Thus, the study found SPECT to be particularly helpful in the planning of medial tibiofemoral unicompartimental arthroplasty to confirm unicompartmental disease [15]. Correlations between the osteoarthritis and increased tracer uptake in the associated compartment were demonstrated, and correlation of the degree of osteoarthritis with the degree of tracer uptake was also established in several studies. In one study, a positive and statistically significant correlation was found between the intensity of uptake on SPECT and the severity of the arthroscopic findings in the menisci and medial femoral condyle. An r value of 0.663 (P >0.001) was shown for the medial meniscus, an r value of 0.67 (P >0.001) for the lateral meniscus, and an r value of 0.7 (P >0.001) for the medial femoral condyle, indicating that the uptake intensity positively correlated with the severity of pathology seen at arthroscopy [16]. Furthermore, the intensity of the tracer uptake correlated with the degree of malalignment, and thus SPECT/CT reflects the specific loading pattern of the knee with regard to its alignment. In the postoperative setting, SPECT/CT has also proved to be useful for a variety of indications. Interestingly, when evaluating patients after ACL repair, tracer uptake on SPECT/CT showed no correlation with instability, pivot shift or clinical laxity testing. However, the tracer uptake correlated significantly with the position and orientation of the ACL graft (e.g., a more horizontal femoral graft position showed significantly increased tracer uptake within the superior and posterior femoral regions, and a more posteriorly placed femoral insertion site showed significantly more tracer uptake within the femoral and tibial tunnel regions etc.). Thus, SPECT/CT tracer uptake intensity and distribution showed a significant correlation with the femoral and tibial tunnel position and orientation in patients with symptomatic knees after ACL reconstruction [17]. In another study that investigated the use of SPECT for displaying bone remodeling after knee arthroplasty, there was a significant correlation between 12-month SPECT uptake and preceding bone marrow density change in the medial tibia (r = 0.5, P = 0.044) [18]. At 12 months, SPECT uptake in the operated knee was notably higher compared with that of the control knee. SPECT uptake showed a statistically significant decrease from 12 months to 24 months, while SPECT uptake in the control knee remained stable. The authors concluded that increased SPECT uptake during the first 2 years after uncomplicated total knee arthroplasty is most likely to be a result of normal postoperative bone remodeling. A leveling of SPECT uptake might indicate a new balance between bone loss and regain [18]. Lastly, in another study SPECT/CT was able to change the suspected diagnosis and consequent treatment in a significant number of patients with painful knee arthroplasty. SPECT/CT imaging changed the suspected diagnosis and the proposed treatment in 19/23 (83%) knees based on, for example, identifying progression of osteoarthritis or loosening, and thus it proved to be a helpful tool in establishing the diagnosis and guiding subsequent management [19]. There has recently been a further technical development with the introduction of SPECT/CT arthrography, which overcomes the drawbacks of SPECT/CT compared with MRI by making it possible to evaluate osteochondral lesions, meniscal tears, loose bodies and tears of the cruciate ligaments [20].
Foot/Ankle
Because of the complex anatomy, the evaluation of osseous lesions of the foot and ankle presents clinical and diagnostic challenges. Currently, as in the aforementioned indications, MRI is the imaging gold standard, especially for soft tissue lesions. Detailed, high-resolution imaging can be done on a routine basis to evaluate joint cartilage, tendons, ligaments, fascial and neuronal pathologies, impingement syndromes and stress fractures. Although bone marrow edema (a misnomer) is very nonspecific, it contributes to the diagnosis of the underlying pathology [21]. However, one of the main problems of MRI in general is its nonspecificity. In several studies and in several anatomical locations, SPECT/CT has been shown to have higher specificity as well as higher intraobserver and interobserver agreement, which is important in clinical investigations for which there is no specific musculoskeletal radiologist available. In patients with osteoarthritis of the foot and ankle, SPECT/CT has demonstrated a significantly superior intraobserver diagnostic precision for the site of active arthritis. The mean intraobserver reliability for SPECT/CT was excellent (κ = 0.86; 95% confidence interval 0.81 to 0.88) and significantly higher than that for CT and bone scanning combined. The authors concluded that SPECT/CT was a very useful imaging tool in localizing active arthritis, especially when the configuration of joints is complex [22]. Also in direct comparison with MRI, SPECT/CT proved to be partly superior in evaluation of the activity of osteochondral lesions of the talus. SPECT/CT helped preoperative planning by identifying the exact location of the active lesion, especially in multifocal disease or revision surgeries, while showing the depth of the active lesion. Patients had partly conservative treatment instead of surgery due to minimal or no activity at the evaluated lesion. In comparison, repeat MRI in this group (new onset of pain) confirmed the diagnosis of an osteochondral lesion, but did not provide further meaningful information. Also in the group of patients who did not undergo operation, while SPECT made a diagnosis of a nonactive osteochondral lesion, MRI provided only a „morphological” diagnosis without helpful information about the activity of the lesion [23]. Other studies have confirmed the influence of SPECT/CT in comparison with MRI in these patients. In comparison with MRI alone, treatment decision making was changed in 48% of cases with SPECT/CT alone, and 52% with SPECT/CT and MRI combined. While interpretation of cartilage shows good correlation between MRI and SPECT/CT, assessment of the subchondral bone plate and subchondral bone has shown substantial differences in correlation that highlight the different information provided by these imaging techniques. Overall, compared with MRI, SPECT/CT provides additional information and influences the decision making of osteochondral lesion treatment and therefore it might be useful to perform both procedures. Lastly, SPECT/CT has been found to be useful in guidance of local infiltration in patients with foot and ankle pain. When infiltrating the area with elevated tracer uptake, a response rate of 90% could be achieved. When assessing the agreement on pain-initiating structures determined by standard clinical assessment versus SPECT/CT, a disagreement in 16 of 30 (53%) cases was found, especially in patients with pain in the midfoot. Thus, SPECT/CT had a higher predictive value of the clinical outcome than the clinical assessment. In the clinical setting, SPECT/CT might overrule the clinical assessment in cases where there is disagreement on the target lesion [24].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree