Fig. 1
The degree of stenosis from a distal left anterior descending coronary artery calcified plaque (white arrow) is difficult to determine due to blooming artifacts. Compare to the more proximal noncalcified plaque, more easily characterized as causing a 60 % stenosis (Image courtesy of Dr. Stefan Zimmerman, Johns Hopkins Hospital, Baltimore, Maryland, USA)
1.2.3 Limitations in the Currently Available Evidence for cCTA
There are increasing calls throughout medicine for high-quality evidence establishing the value of diagnostic tests, including cCTA. While the exact methodology for diagnostic imaging validation is not yet established, the evidence required to establish a test as valuable, both on an individual and societal level, generally follows a certain pattern. First, of course, the safety of the test must be established, followed by validation of diagnostic accuracy against a reference standard. The value of prognostic data are increasingly emphasized, as is the ultimate effect on clinical management and outcomes. Finally, the growing economic impact of healthcare throughout the developed world has led to greater emphasis on cost-effectiveness analyses. The quality of the evidence, of course, is also important, with greater weight given to data from large-scale, multicenter randomized trials.
Compared to other cardiac imaging techniques, cCTA is relatively young, and this is reflected in the quantity of available evidence. There are limited large-scale trials, especially regarding prognosis, outcomes, and cost-effectiveness. In addition, the data that are available are often subjected to heterogeneous patient populations (which do not clearly reflect the indications set forth in current clinical guidelines), referral bias, and marked variability in experimental design. More detailed limitations in the evidence are provided in Table 1. As such, the clinical role of cCTA is evolving rapidly as new data become available. Fortunately, several large-scale, well-designed trials are underway that should provide considerable value in optimizing cCTA utilization.
Table 1
Limitations in the currently available evidence for cCTA, stratified by generalized data parameters
Diagnostic accuracy |
Most reports consist of single-center studies conducted at academic centers with considerable experience in cCTA, limiting the applicability to mainstream clinical practice |
There are limited data for newer techniques utilizing dose-saving techniques; the high diagnostic accuracy seen in most studies is therefore accompanied by relatively high radiation exposure |
High variability in treatment of small, highly calcified, or otherwise uninterpretable coronary artery segments; i.e., some studies utilize intent-to-treat designs, others exclude these segments |
Technical advancements continue to occur at a rate that quickly renders results obsolete |
Anatomic endpoints may be inferior to functional endpoints in guiding patient care |
Most studies define “obstructive disease” as stenosis ≥ 50 %, and this endpoint is compared to ICA; however, management often relies on the identification of ≥ 70 % stenosis |
Outcome variables are heterogeneous and may not be clinically validated |
Most studies use populations referred for ICA, resulting in inherent referral bias |
Asymptomatic patients, acutely symptomatic patients, and/or those with known CAD are variably included and/or combined in analyses, limiting the applicability of data to established clinical indications |
Prognosis |
Limited large-scale trials currently available |
Significant inter- and intra-study heterogeneity in patient populations limits the applicability of data to established clinical indications |
CAD classification and reporting are variable and are not limited to standard/recommended clinical practice. In addition, the diagnostic accuracy of more advanced CAD reporting is not well established |
Most studies include coronary revascularization as an endpoint, which may not have been warranted or may have been performed as a result of cCTA findings, leading to verification bias |
There is low incidence of adverse cardiac outcomes, especially when revascularization is excluded or when all-cause mortality is used as the primary endpoint. Therefore, large cohorts with specific inclusion criteria and long follow-up is required |
Economic impacts and effects on clinical management and outcomes |
Limited large-scale randomized trials, with data primarily coming from small single-center observational cohorts, larger cohorts utilizing insurance claims data, or simulation models based on prior data |
Significant disagreement on the value of different endpoints (for example, cost/quality-adjusted life year, cost/correct diagnosis, incremental cost-effectiveness ratio, etc.) |
High variability in patient populations between studies (especially pretest probability) has led to significantly different conclusions |
The influence of cCTA utilization on the non-surgical management of CAD is particularly inconclusive from the available data |
The effects and optimal management of incidentally detected findings are not well established |
1.3 Current Use of Anatomic Data from cCTA
The high NPV of cCTA for the detection of obstructive CAD (≥ 50 % stenosis) forms the basis for currently accepted clinical utilization (Fig. 2). Of note, more advanced characterization of CAD (e.g. quantification, plaque morphological analysis, etc.) is considered experimental at this time. Broadly speaking, cCTA is considered acceptable to detect atherosclerosis in patients with suspected CAD, to rule out significant disease in patients presenting with acute chest pain, to rule out an ischemic etiology in patients without known CAD and new-onset heart failure, for the detection of CAD prior to noncoronary cardiac surgery, and for risk assessment in patients with prior percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG) (Taylor et al. 2010). Optimal integration of cCTA into clinical practice requires the ordering physician to consider all diagnostic and prognostic data available before the test is performed and integrate that information with cCTA results. In addition, the abilities (i.e., high sensitivity) and limitations (i.e., limited positive predictive value) of cCTA must be considered within the clinical situation. Finally, the relative value of alternative diagnostic strategies should be considered in each individual scenario.
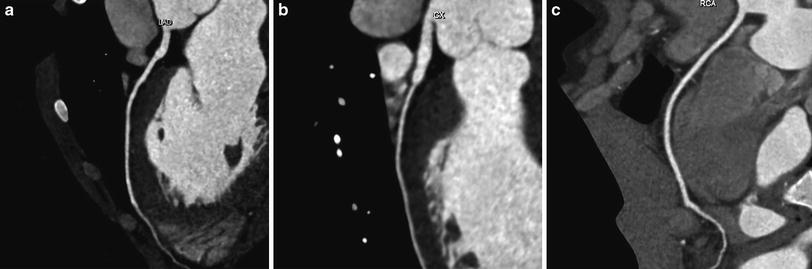
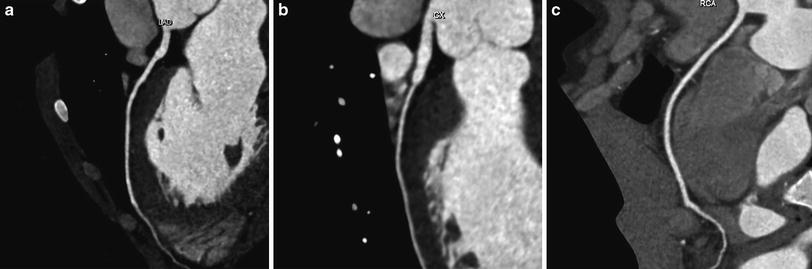
Fig. 2
Normal cCTA shows left anterior descending (a), left circumflex (b), and right (c) coronary arteries without evidence of atherosclerosis (Images courtesy of Dr. Stefan Zimmerman, Johns Hopkins Hospital, Baltimore, Maryland, USA)
The preceding considerations are reflected in the current guidelines for acceptable use of cCTA. The pretest probability (PTP) of disease is an integral component of diagnostic decision-making (Taylor et al. 2010). For example, a patient presenting to the emergency department with acute chest pain and high PTP of significant CAD will likely receive ICA regardless of cCTA results, resulting in increased costs with minimal effect on outcomes or management. Consider, however, a similar patient with low-to-intermediate PTP. The high NPV of cCTA results in the test being well suited to rule out significant CAD in a large proportion of this population, allowing fast, safe discharge (Bamberg et al. 2012). Similar Bayesian techniques should be used on an individual basis for other indications.
2 Technique
There are two basic goals in the acquisition, reconstruction, and interpretation of cCTA examinations: provide maximum diagnostic value while minimizing radiation dose. Newer technologies have increased the quality of anatomic imaging while decreasing ionizing radiation burden; however, proper patient selection, preparation, and post-processing are still vital for optimal performance. This section will highlight the most important considerations and advances in cCTA techniques.
2.1 Patient Selection and Preparation
As noted above, there are multiple patient-specific factors that have a dramatic effect on image quality. Obese patients will require increased tube output for adequate images, and very obese patients should not undergo cCTA. The patients must be able to hold their breath for the duration of the scan, which will be variable depending on the hardware and specific acquisition protocol employed. Patients with very high heart rates or irregular heart rhythms should be carefully assessed and possibly excluded. Preprocedural beta-blocker administration may be used in some cases to reduce heart rate. In addition, some institutions routinely administer nitroglycerin to promote coronary artery vasodilatation and improve image quality. Finally, optimal cCTA acquisition necessitates adequate opacification of the coronary artery lumen; therefore, vascular access must be adequate for high flow rate (4–6 mL/s) administration of intravenous contrast material. Appropriate contrast bolus timing is vital, and both test-bolus and automated bolus tracking techniques can be used.
2.2 Dataset Acquisition
The characteristics of the raw dataset are a major determinate of ultimate image quality. The major parameters influencing the quality of subsequently reconstructed axial 2D images will be spatial and temporal resolution. In addition, detector coverage and acquisition time play a role in the quality of the examination along the z-axis, affecting subsequent multiplanar and 3D reconstructions. It is important to note that while technical advances are often presented as a solution for a specific imaging parameter (e.g., increased volumetric coverage to improve quality along the z-axis), they usually affect other parameters as well, not always positively.
2.2.1 Temporal Resolution
Temporal resolution is largely a function of the time necessary to acquire a full 360° dataset. As noted above, some authors have proposed that temporal resolution of 30–50 ms will be necessary for true “motion-free” imaging (Lu et al. 2001; Otero et al. 2009). The most obvious method of improving temporal resolution is via faster gantry rotation times, which are now as low as 280–400 ms. However, further improvements will be limited by the mechanical properties of current components, as massive centrifugal forces are generated with such rotational speeds, especially with the increasing mass of wide-detector arrays. Additional techniques to improve temporal resolution include the utilization of half-scan reconstructions (since 360° of data may be acquired with one half gantry rotation). The advent of “dual-source” scanners, containing two sets of X-ray sources and detectors offset at 90°, has allowed further improvement via quarter-scan reconstructions. There are tradeoffs, as both half-scan and quarter-scan reconstruction is subject to misregistration artifacts, and dual-source CT techniques increase X-ray cross-scatter. Multisegment reconstruction, using combined data from adjacent slices, is also available, but has the disadvantage of necessitating decreased pitch, increasing dose, and overall acquisition time. Different commercial products provide specific combinations of these features, and temporal resolution varies accordingly, with the most popular current systems providing resolution of 75–175 ms.
2.2.2 Spatial Resolution
Both intrinsic limitations and reconstruction techniques contribute to the ultimate spatial resolution of cCTA. While spatial resolution is scientifically measured as the minimal allowable distance between 2 structures before they cannot be recognized as separate, voxel size is often used as an indirect surrogate for spatial resolution in cCTA. The x–y lengths are a function of intrinsic CT limitations (e.g., focal spot size and sampling density) and reconstruction techniques, while the z-axis length is largely a function of detector width. As explained above, current voxel dimensions of approximately 0.5 mm3 are considered adequate for qualitative assessment of the major coronary artery segments but are considered inadequate for quantitative imaging or evaluation of extremely small coronary vessels.
The signal-to-noise ratio, which is related to spatial resolution, is an important consideration as detector widths continue to decrease. Either increased dose, improved reconstruction techniques, or increased detector efficiency will be necessary to maintain adequate photon collection. Technical advances will also be required to compensate for photon loss with improvements in gantry rotation and scan acquisition times.
2.2.3 Volumetric Coverage
The advent of multidetector CT systems, providing increased volumetric (z-axis) coverage with each gantry rotation, was arguably the initial technical advancement that led to the growth of cCTA. While improvements in spatial and temporal resolution have led to improved diagnostic accuracy, the initial feasibility of coronary imaging necessitated full cardiac volume acquisitions in a single breath-hold. With increased detectors, fewer rotations of the gantry are necessary to provide complete coverage and total acquisition time is decreased. Continued advancements have led to decreased stair-step artifacts, respiratory motion artifacts, and misregistration artifacts. Faster acquisition times also reduce the significance of heart rhythm abnormalities. Currently, 256- and 320-channel systems have been developed, providing coverage up to 160 mm with a single gantry rotation. These wide-detector systems have made single heartbeat acquisitions a reality. However, while isophasic datasets may intuitively seem attractive, they may not be necessary for anatomic imaging, and the most recent advances in volumetric coverage are driven as much by the prospect of myocardial perfusion imaging as a desire for improved anatomic assessments. Indeed, the wide-cone X-ray beams used for extended z-axis coverage in some systems may come at the expense of decreased spatial resolution from cone-beam artifact, scatter, or roof-top effect. At this time, most of these systems have not been validated as thoroughly as more traditional 64-slice scanners.
Another technique has been introduced to decrease scan acquisition times by using a high-pitch (3.4) spiral acquisition rather than complete cardiac volumetric coverage. This acquisition protocol, which is available in patients with low (< 60 beats/minute) and stable heart rates, can acquire a complete dataset in 250 ms, within one cardiac cycle. The technique also results in very low-radiation dose (Fink et al. 2011).
2.3 Image Reconstruction and Interpretation
Multiple phases of the cardiac cycle will be available following a retrospectively ECG-gated cCTA acquisition. Either automated or manual means should be used to determine the optimal phase for coronary analysis. The appropriate cardiac phase may vary between the left and right coronary circulation. Traditional cCTA dataset reconstruction utilizes filtered back projection techniques; however, there is an increasing interest in iterative reconstruction, which has become more practical with increased computing power. Preliminary data suggest that the greatest role for iterative reconstruction may be in radiation dose reduction, as image quality is maintained at decreased tube currents (Leipsic et al. 2010). Iterative reconstruction may also result in improved image quality (Fig. 3), particularly in the assessment of heavily calcified vessels and stents (Renker et al. 2011).
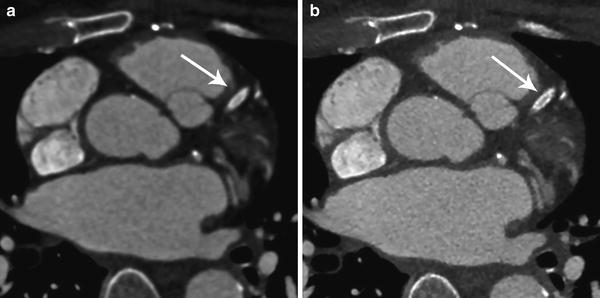
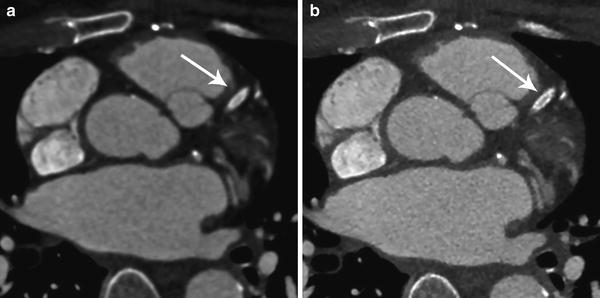
Fig. 3
Filtered back projection reconstruction (a) provides inferior spatial resolution compared to iterative reconstruction (b) in the assessment of a left anterior descending coronary artery stent (arrow) (Images courtesy of Dr. Stefan Zimmerman, Johns Hopkins Hospital, Baltimore, Maryland, USA)
Most authors advocate the use of several different reconstructions for cCTA anatomical interpretation. Axial images are traditionally used for primary analysis; furthermore, abnormalities seen on additional reformations should be confirmed with axial source images. Multiplanar imaging is available, allowing visualization of the coronary arteries in short- or long-axis, and curved multiplanar reformations allow single-image display of the entire coronary artery length and rotation of the artery along its long axis. Thick-slab maximum intensity projections provide a vascular map, while volume-rendered 3D images allow an overview of coronary anatomy, especially in cases of CABG, but are inadequate for assessment of the coronary artery lumen (Fig. 4).
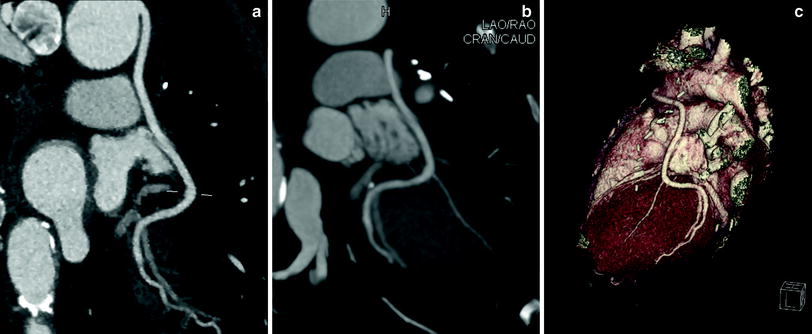
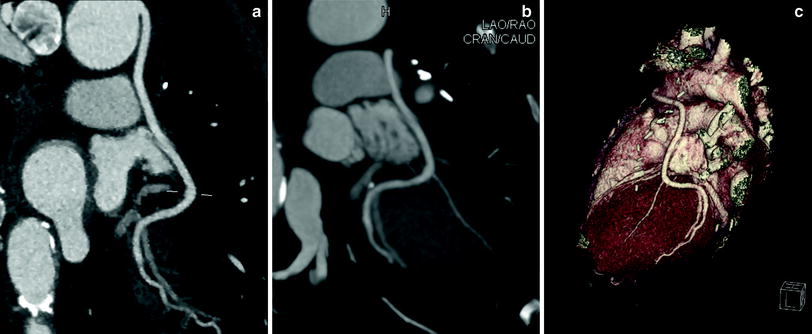
Fig. 4
Curved multiplanar reformation (a), thick-slab maximum intensity projection (b), and 3D volume rendering (c) reconstructions play a role in the assessment of a saphenous vein coronary artery bypass graft to the left circumflex territory (Images courtesy of Dr. Stefan Zimmerman, Johns Hopkins Hospital, Baltimore, Maryland, USA)
Computer-aided detection and automated atherosclerosis characterization and quantification programs are becoming increasingly available, and some have shown promising preliminary results (Arnoldi et al. 2009; Blackmon et al. 2009); however, manual assessment remains the mainstay of interpretation at this time. While the current evidence for cCTA is based on relatively simple reporting schemes (similar to ICA), several groups have published studies suggesting the value of more complicated reporting and scoring systems (Chow et al. 2011b ; Kazmi et al. 2011; Min et al. 2007). The Society of Cardiovascular Computed Tomography published a consensus document on cCTA interpretation and reporting in 2009 (Raff et al. 2009a), and we anticipate more guidance and standardization as techniques and data evolve.
3 cCTA in Stable Patients with Suspected CAD
The initial diagnostic evaluation of patients without known CAD presenting with stable chest pain or angina equivalent is complex. Optimizing diagnosis and management of these patients, however, is a major priority considering the scope of the disease and its current and future economic impact. Several strategies are available for initial diagnostic workup, including direct ICA, exercise ECG, exercise and pharmacologically stressed scintigraphy, exercise and pharmacologically stressed echocardiography, and stress magnetic resonance imaging. Anatomic imaging with cCTA has been proposed as a fast, reliable, and possibly cost-effective modality for the initial approach to suspected CAD; in addition, cCTA may have a role as a “gatekeeper” to ICA in certain patients with nondiagnostic or equivocal functional test results.
Currently available evidence on diagnostic accuracy, prognostic value, and effects on outcomes and costs highlight both the advantages and limitations of the technique. Repeatedly, the data show the importance of proper patient selection in order for cCTA to provide cost-effective therapeutic value. Patient populations with low to intermediate prevalence of disease are most likely to benefit from evaluation with cCTA, while high CAD prevalence increases costs and radiation burden without a positive effect on outcomes.
3.1 Diagnostic Accuracy
Hundreds of studies on various aspects of cCTA diagnostic accuracy have been published over the past decade. As highlighted in Table 1, there are multiple limitations in the available evidence; however, the available data are promising. cCTA consistently shows high diagnostic accuracy to detect obstructive CAD with ICA as the reference standard (Fig. 5). The reported sensitivity and NPV of cCTA are particularly notable, often approaching 100 % in meta-analyses (Mowatt et al. 2008; Sun and Ng 2012). Larger prospective multicenter studies are limited, with only 4 such studies using exclusively 64-slice scanners or higher currently available. Two of the studies include patients with known CAD (Miller et al. 2008) or unstable patients (Meijboom et al. 2008); predictably, the prevalence of CAD was high in these cohorts (56 and 68 %, respectively). Prevalence of 68 % might be expected to negatively impact NPV; however, the authors demonstrated an impressive NPV of 97 %. The other two studies are more applicable in our population. ACCURACY, which included only stable patients being referred to ICA for stable chest pain syndrome and/or abnormal stress test results, had the lowest prevalence of disease, 25 %. Predictable, NPV was excellent in this cohort (99 %) (Budoff et al. 2008).
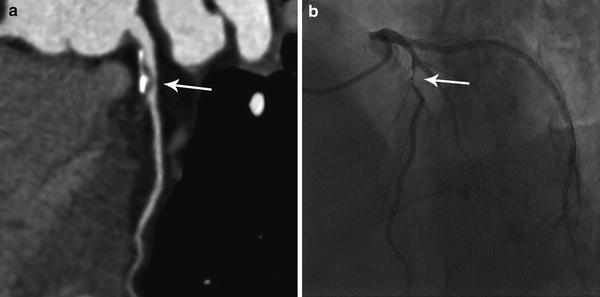
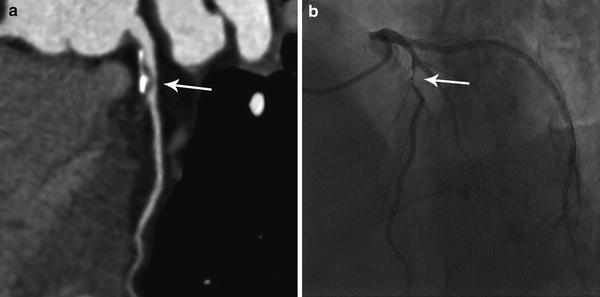
Fig. 5
An obstructive plaque (arrows) was detected in the proximal left anterior descending artery on cCTA (a), determined to represent an 80–90 % stenosis on subsequent ICA (b) (Images courtesy of Dr. Stefan Zimmerman, Johns Hopkins Hospital, Baltimore, Maryland, USA)
The positive predictive value (PPV) of cCTA is more limited (ranging from 64–97 % in the 4 prospective studies mentioned above), especially in higher prevalence populations. This could lead to unnecessary, costly, and possibly dangerous subsequent workup, and highlights the need for clinicians to perform robust pretest assessments and order the examination only when appropriate. Further study of cCTA diagnostic accuracy should also increase the evidence comparing cCTA to other noninvasive modalities, such as myocardial perfusion scintigraphy.
3.2 Prognostic Value
The highest-level evidence on the prognostic value of cCTA in stable symptomatic patients uniformly demonstrate the value of cCTA as a rule out test, with a normal scan associated with annualized major adverse cardiac event rates ranging from 0.17 to 0.4 % (Bamberg et al. 2011; Hulten et al. 2011) and all-cause mortality rates ranging from 0.28 to 0.36 % (Chow et al. 2011b; Min et al. 2011). These data support the evidence showing the high NPV of cCTA and compare favorably with other diagnostic strategies, including ICA, myocardial perfusion scintigraphy, and stress echocardiography (Lichtlen et al. 1995; Metz et al. 2007; Shaw and Iskandrian 2004). While the length of protection afforded by a normal cCTA examination is not well-established, one analysis of 1,816 patients with at least 4-year follow-up showed annualized death rates of only 0.22 % (Min et al. 2011), suggesting that 4 years may be a reasonable post-test interval. Current evidence also suggests that there is prognostic value in the detection of obstructive disease, with significantly increased rates of major adverse cardiac events (annualized rates up to 11.9 % in one meta-analysis (Bamberg et al. 2011)) and all-cause mortality (up to 2.9 % (Chow et al. 2011b)) in patients with obstructive disease. The prognostic value of more advanced analyses, such as plaque morphology and segmental stenosis scoring, is also being examined and is discussed below in Emerging Applications.
An ongoing goal is to establish the incremental prognostic value of cCTA beyond more established tests. Early data are favorable, with several studies showing increased prognostic value over coronary artery calcium scoring (Bamberg et al. 2011; Hadamitzky et al. 2011) and myocardial perfusion scintigraphy (Shaw et al. 2008; van Werkhoven et al. 2009). In addition, researchers are seeking to refine the population-specific prognostic value of cCTA, e.g., in younger patients, females, or diabetics.
3.3 Outcomes and Costs
There are substantial methodological weaknesses in all of the currently available data on outcomes and costs of cCTA in stable symptomatic patients; however, two large-scale randomized clinical trials are currently underway. The RESCUE trial will compare cCTA to myocardial perfusion scintigraphy in 4,300 patients with stable angina or angina equivalent and the PROMISE trial will compare cCTA to traditional stress testing (ECG, echocardiography, or scintigraphy) in 10,000 symptomatic patients with low to intermediate PTP of CAD. Both studies will follow patients to compare outcomes and costs.
Until then, we must rely on the available observational cohorts and simulation models, which currently suggest that cCTA provides incremental cost-benefit (cost/correct diagnosis) and cost-effectiveness (cost/quality adjusted life year) compared with alternative strategies in populations below a certain prevalence of disease. These data are variably driven by improved outcomes using cCTA-based strategies (Ladapo et al. 2009), decreased costs (Dorenkamp et al. 2011; Genders et al. 2009; Min et al. 2008a), or some combination. Importantly, no current data have shown adverse outcomes when cCTA is used. cCTA has not been shown to be cost-effective in populations with PTP greater than 37–55 % (Dorenkamp et al. 2011; Genders et al. 2009) or disease prevalence greater than 30–50 % (Min et al. 2010; Shreibati et al. 2011) due to high downstream resource utilization (particularly subsequent ICA) (Min et al. 2008a; Shreibati et al. 2011). Of note, real-world observational studies have shown decreased downstream resource utilization following clinical cCTA implementation, possibly due to more appropriate patient selection and clinical management (Karlsberg et al. 2010).
4 cCTA in Patients with Acute Chest Pain
The workup and triage of patients presenting to the emergency department with acute chest pain represents a common and difficult diagnostic dilemma across the developed world. While ECG, clinical decision rules, and sensitive cardiac biomarkers are available and can lead to rapid triage to ICA in a minority of cases, greater than 80 % of patients have a nondiagnostic initial workup and require either serial clinical and laboratory monitoring or additional testing (Anderson et al. 2007). Furthermore, approximately 80 % of those patients will eventually receive a diagnosis of non-cardiac chest pain (Roger et al. 2012), and a small but concerning percentage of discharged patients actually have ACS. The process is not only expensive but also results in a significant diversion of resources as patients are monitored or prepared for time-consuming tests such as cardiac scintigraphy. The speed and excellent NPV of cCTA form the basis for its utilization in these situations, with the primary goal of providing safe, rapid discharge for the large percentage of patients without ACS.
4.1 Diagnostic Accuracy and Prognostic Value
Many studies have been published on the diagnostic accuracy of cCTA; however, studies encompassing only patients presenting to the emergency department with acute chest pain and low to intermediate PTP of ACS are more limited. Nevertheless, early data again suggested that cCTA is very reliable in excluding CAD. Recently, more robust data have emerged that again displays the excellent NPV of cCTA for the detection of patients with ACS. Importantly, and in contrast to diagnostic studies in which other imaging is used as the reference standard, these investigations have used index hospitalization and follow-up data to determine positive findings (i.e., ACS) and calculate diagnostic accuracy and prognostic value.
One of the first large prospective observational studies evaluating cCTA in the setting of acute chest pain was the ROMICAT trial, which enrolled 368 patients with low to intermediate risk. The NPV of cCTA in the detection of any CAD (50 % of the subjects) was 100 %, while the NPV was 98 % when cCTA detected CAD but no significant stenoses (Hoffmann et al. 2006). Three multicenter randomized controlled trials have been performed that displayed similar data, all enrolling patients with low to intermediate PTP presenting to the emergency department with acute chest pain. The CT-STAT trial randomized 699 patients to either cCTA or myocardial perfusion scintigraphy and found no difference in adverse events after 6 months (Goldstein et al. 2011). The ROMICAT II trial randomized 1,000 patients to either cCTA or standard evaluation and demonstrated a 100 % NPV for cCTA in the exclusion of ACS. In addition, there was no difference in major adverse cardiac events between the two strategies after 28 days (Hoffmann et al. 2012). A 2012 study randomizing 1,370 patients to cCTA or standard care also showed the value of negative cCTA examinations, with zero deaths or MIs after 30 days in the 640 patients with a negative study (Litt et al. 2012).
As before, the PPV of cCTA in these situations is much more limited, hence the evolution of the test into a largely “rule-out” role. In addition, the ability of cCTA to detect functional stenoses in these patients is also limited; however, this fact per se does not undermine cCTA’s value as a rapid triage test.
4.2 Outcomes and Costs
The importance of proper patient selection is again emphasized in cost-effectiveness data for cCTA utilization in the emergency department. Several of the large observational studies presented in Sect. 3.3 included patients with acute chest pain, and some of the conclusions can justifiably be extrapolated to this population. Namely, patients with a high risk of ACS or CAD should not undergo cCTA, as downstream ICA utilization will be high and drive up costs without outcome benefits. Model-based analyses specific to the acute chest pain setting have shown cCTA-based strategies can be more cost-effective than stress ECG, stress echocardiography, and myocardial perfusion scintigraphy under certain conditions, including disease prevalence <70 % (Khare et al. 2008; Ladapo et al. 2008).
Fortunately, the randomized controlled trials mentioned above have also provided fairly robust data on the potential value of cCTA. While the CT-STAT trial demonstrated a 38 % cost savings per patient in the cCTA arm, ROMICAT II found no differences in cumulative per-patient costs between cCTA and traditional care. Importantly, however, there is strong data pointing to several other benefits of a cCTA-based approach. CT-STAT demonstrated a 54 % reduction in the time to diagnosis when cCTA was used, while ROMICAT II and the study by Litt et al. showed significant decreases in total length of stay compared to traditional care (median 8.6 vs. 26.7 and 18.0 vs. 24.8 h, respectively). In both of the latter studies, nearly half of patients undergoing cCTA were discharged directly from the emergency department, compared to 12–23 % of those patients in the standard care arms. Litt et al. also showed that while there was no difference in rates of subsequent ICA, patients who had undergone cCTA were more likely to have positive ICA findings, suggesting that cCTA may lead to more appropriate clinical decision-making.
5 Other Indications
5.1 Evaluation of Patients with New Heart Failure
The differentiation of ischemic cardiomyopathy from nonischemic dilated cardiomyopathy, the two major causes of heart failure in the developed world, has important prognostic and management implications. Perhaps most importantly, patients with systolic dysfunction secondary to CAD may be amenable to revascularization. As such, ICA is employed in the diagnostic workup of certain patients with new-onset or newly diagnosed heart failure. cCTA may represent a noninvasive alternative to ICA in some patients, especially considering its high NPV, and current guidelines consider cCTA use acceptable in patients without known CAD with low or intermediate PTP (Taylor et al. 2010). The justification for this is largely based on broader studies, with only limited population-specific evidence. However, the little data that are available are generally favorable, with sensitivities and specificities ≥ 90 % for the detection of CAD or ischemic heart disease. Furthermore, one small prospective study found that all patients with a negative cCTA examination could avoid ICA, suggesting some cost benefits (Ghostine et al. 2008; Hamilton-Craig et al. 2012). Further evaluation on prognosis, outcomes, and costs will be necessary to refine the role of cCTA in this situation.
5.2 Patients Prior to Noncoronary Cardiac Surgery
ICA is widely utilized prior to noncoronary cardiac surgery, especially valvular surgery, and is considered acceptable in this situation by current practice guidelines (Patel et al. 2012a). Again, cCTA may offer an attractive alternative in this situation, but population-specific data are limited. Several studies have shown high diagnostic accuracy in preoperative coronary evaluation (Mark et al. 2010); furthermore, two studies examining outcomes have shown that cCTA is safe, with one study finding no MACE in the perioperative period or at 3 month follow-up in patients with a negative cCTA (Buffa et al. 2010) and another study finding no difference in operative mortality or postoperative MI between patients who had received cCTA compared to those who had received ICA (Nardi et al. 2011). Again, the value of cCTA may lie in its ability to prevent unnecessary catheterization in a large number of patients. Of the two studies mentioned above, 81–85 % of patients undergoing cCTA had negative examinations and were able to safely avoid ICA.
5.3 Patients with Coronary Artery Stents
In-stent restenosis remains a considerable problem in modern cardiology practice. Unfortunately, there are several limitations associated with cCTA stent evaluation, and current guidelines consider cCTA acceptable only in the evaluation of left main coronary artery stents ≥ 3 mm in asymptomatic patients (Taylor et al. 2010). The main problem involves poor image quality rendering a significant proportion of stents unevaluable. High-density stent material is subject to beam-hardening and blooming artifacts, and partial volume averaging can result in artificial luminal narrowing of up to 60 %. The percentage of unevaluable stents varies widely between reports; however, even with specialized reconstruction techniques, at least 8 % of stents cannot be reliably assessed with current scanners (Mahnken 2012). Various parameters have been associated with stent evaluability, including strut thickness, stent location, and stent material; however, the strongest evidence points to stent diameter as the most important parameter, with accessability rates varying from 100 % in stents ≥ 3.5 mm to 33 % when diameter is <3 mm (Sheth et al. 2007).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree