CYSTIC LESIONS OF BONE
KEY POINTS
- Cystic bone lesions in the head and neck region most commonly involve the mandible and maxilla.
- Giant cell tumors, giant cell granulomas, and brown tumors are difficult to distinguish on a pathologic basis.
- Pathology of bone lesions should almost always be read together with the imaging findings to produce the best diagnoses and optimize medical decision making.
- Aneurysmal bone cysts have a distinct imaging appearance once magnetic resonance imaging is done.
- Subperiosteal hematic cysts have a distinctive appearance.
- Bone cysts likely have more than one etiology, and some may cause significant symptoms.
- If a bone lesion of the mandible or maxilla is believed to be due to a vascular malformation, the treating doctor must be informed and a study to evaluate its vascular nature performed before any operative intervention.
GIANT CELL TUMORS, GIANT CELL GRANULOMAS, AND BROWN TUMOR OF HYPERPARATHYROIDISM
Clinical Perspective and Pathology
Giant cell tumors (GCTs), giant cell granulomas (CGCs), and brown tumors are all focal osteolytic-appearing, sometimes aggressive, still with a narrow zone of bony transition, lesions that affect primarily the mandible and maxilla1(Fig. 41.1). Cortical penetration is frequent. GCGs have also been reported in ethmoid, sphenoid, and temporal bones. The modifier “reparative” has been dropped from the GCG. These lesions may only be distinguishable from each other on the basis of parathormone assay, clinical factors such as age, subtle histopathologic differences, and tendency to recur following curettage since recurrence is likely if a GCT is just curetted. GCT occurs later in life than GCG, usually in the second and third decades.2,3 Brown tumors are associated with either primary or secondary hyperthyroidism and are discussed in Chapter 43 related to metabolic bone disease.4
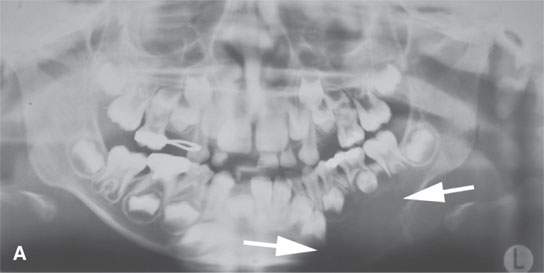
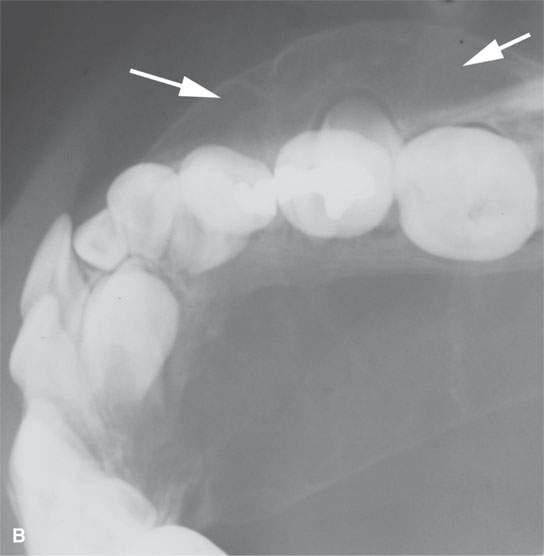
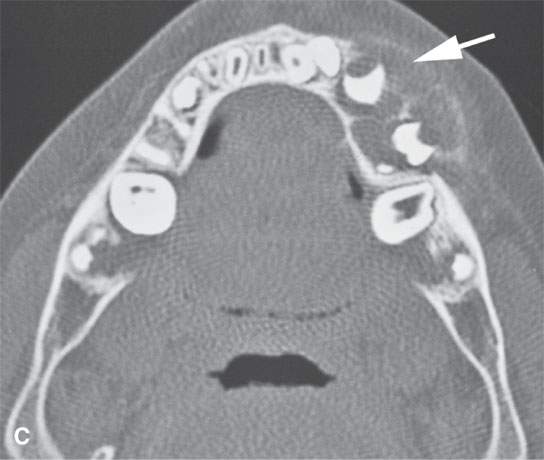

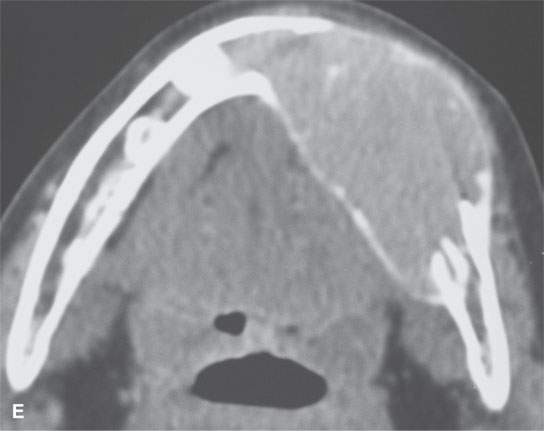
FIGURE 41.1. A patient with giant cell granuloma. A: Orthopantomography showing a large cystic-appearing lesion of the mandibular body (arrows). B: Dental occlusal views showing the remaining cortical margin of thin bone (arrows). C: Computed tomography (CT) for correlation with (B), where a thin margin of cortical bone remains around the remodeled tissue within the granuloma. D: CT of the bone window to show overall extent of the lesion. E: CT of soft tissue windows to show the compact cellularity of the lesion creates a tissue density somewhat more than that of skeletal muscle.
Pathologically, these three lesions are a mix of proliferating giant cells or osteoclasts in a generally well-vascularized background of fibrous tissue; this accounts for their looking somewhat alike on images with a few possibly distinguishing characteristics on occasion.
The differential diagnosis typically includes several other lesions, including dental-, osteoid-, chondroid-, and fibrous-origin bone lesions as well as metastases and the medullary form of plasmacytoma.
Imaging Appearance and Differential Diagnosis
These are all “expansile”-appearing lesions of bones with bony margins able to remain mineralized and/or show narrow margins of indistinct transition. Soft tissue interfaces generally remain sharp but may be slightly indistinct as well. The extent of bony abnormality is best studied with computed tomography (CT).1,5 Of the three, the GCT is most likely to show the more aggressive range of bony margins.
The masses may appear solid or “multiloculated” and enhancing internally on both contrast-enhanced CT and contrast-enhanced magnetic resonance (MR). GCG may show patchy areas of mineralization (Fig. 41.1E). GCT and brown tumors should not mineralize unless healing of residual bone is being mistaken for tumor mineralization (Fig. 14.11). Sometimes, fairly diffuse subtle mineralization in a trabecular type of pattern that can be seen in the brown tumors as they begin healing.
The internal contents are usually isointense or hypointense to muscle on non–contrast-enhanced T1-weighted MR images. All tend to be more between muscle and fat in signal intensity on non–fat-suppressed T2-weighted images because of their fibrous tissue content unless truly cystic change usually related to necrosis or hemorrhage is present.
Hemorrhage is a part of the natural history of all these entities; thus, blood products, in all phases of evolution, may be visible on MR studies; the evolutionary appearance of blood products were discussed in Chapters 10 and 11. If actual fluid levels and an essentially entirely cystic nature are present, those findings strongly suggest aneurysmal bone cyst (ABC) discussed subsequently. GCT may have a minority ABC internal component.
Radionuclide scanning will generally show increased uptake and is nondefinitive and cost additive unless one is trying to distinguish solitary from multifocal disease.6
Angiography will show these to be vascular blood pool–type lesions and is infrequently performed.
ANEURYSMAL BONE CYST
Clinical Perspective and Pathology
ABCs are nonneoplastic lesions that most commonly involve the mandible, maxilla, cervical spine, and skull.7 They are a true rarity in other facial bones, sinuses, larynx, and hyoid bone. They are made up of many blood-filled spaces that do not have an endothelial lining. Numerous theories with regard to their etiology have been advanced. The most prominent of these is a relationship to a precursor benign tumor, including GCT, and some sort of response to trauma.8 Rapid enlargement is likely related to hemorrhage.
ABCs may require low-dose radiation in combination with surgery to control recurrences. The recurrence rate following curettage is about 25% to 30%. Recurrences tend to occur within 6 months.
Imaging Appearance and Differential Diagnosis
The combined CT and MR appearance make the preoperative diagnosis almost unmistakable even though the lesions are infrequent. A multilocular, expansile lytic lesion with sharp or dehiscent margins is seen on bone detail CT. The margins with soft tissue are sharp since they are delimited by bone and/or periosteum. On MR, the contents are fluid and may contain obvious fluid–fluid levels due to layering of blood products, as discussed in Chapter 119,10
Differential diagnosis is usually firm after MR imaging is obtained. On the basis of plain films or CT, it would include cystic-appearing versions of dental-, osteoid-, chondroid-, and fibrous-origin bone lesions as well as possibly intraosseous vascular malformations, telangiectatic osteosarcoma, metastases, and the medullary form of plasmacytoma.
INTRAOSSEOUS VASCULAR LESIONS
The venolymphatic and other vascular malformations and vascular tumors discussed separately in Chapters 9 and 25 and all types may affect bone either primarily or secondarily. In extreme cases, this may create a very large expansile lesion of bone, and it can be likened to or actually be Gorham disease of a facial bone.11
It is extremely important to notice when a lytic lesion in the mandible or maxilla has a morphology that suggests it is vascular in origin. The oral/maxillofacial or other treating surgeon should always have been warned and a definitive vascular study considered (Figs. 9.1A and 9.24). CT angiography, MR imaging and MR angiography, or a radionuclide blood pool scan may be sufficient to exclude a vascular lesion and may be substituted in some cases for catheter angiography. In fact, in slower flow vascular malformations, catheter angiography may not be definitive. If the lesion is vascular, endovascular techniques may be used for definitive or adjunctive treatment.
These lesions may bleed considerably if approached by an unwarned surgeon. Treatment with embolization or percutaneous ablative techniques for control or cure may be preferred over surgery.
HEMATIC/HEMORRHAGIC AND TRAUMATIC BONE CYSTS
Clinical Perspective and Pathology
Hematic, hemorrhagic, or traumatic bone cysts are usually posttraumatic due to intraosseous bleeding in the case of traumatic bone cyst and subperiosteal bleed in the case of hematic subperiosteal cysts usually of the orbit12(Figs. 10.39 and 41.2). Other etiologies such as “burned-out” bone tumors, growth disturbances, and osteonecrosis, among others, have been suggested as mechanistic or alternative explanations. These occur in all age ranges. Cavitatory osteonecrosis can create bone cysts and has been associated with the syndrome called neuralgia neuralgia-inducing cavitatory osteonecrosis. This is discussed in conjunction with osteonecrosis in Chapter 43 and dental lesions in Chapter 100.


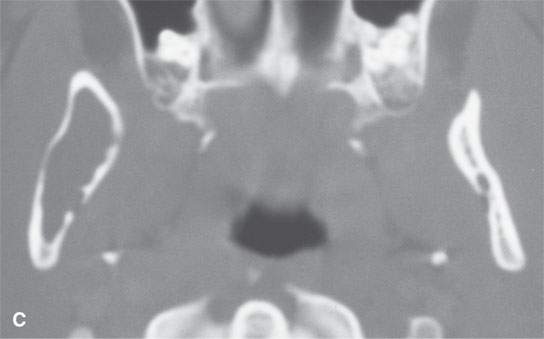
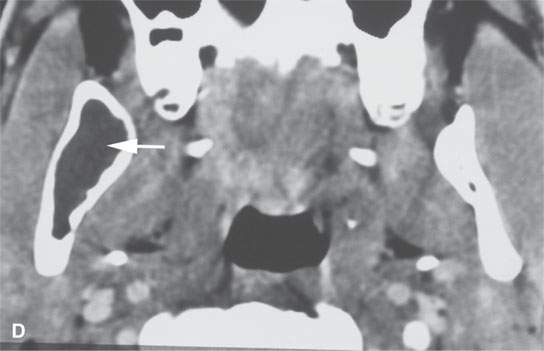
FIGURE 41.2. Bone cyst of the mandible. A: Orthopantomography showing the cystic lesion of the ascending ramus and the body of the mandible (arrow) with a well-defined sclerotic margin (arrowheads). B, C: Computed tomography (CT) showing the overall bony morphology of the lesion; its expansile quality and the well-corticated margins also demonstrated in (C). D: Contrast-enhanced CT study showing the contents of the cystic lesion of the mandible to be fluid equivalent with no discernable related soft tissue enhancement.The lesion was treated surgically, and the final diagnosis was bone cyst. The specific etiology of the bone cyst is still uncertain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








