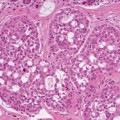
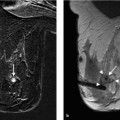
12 Cytologic Evaluation Fine needle aspiration biopsy (FNAB) was introduced by H.E. Martin for the diagnosis of solid tumors almost 80 years ago (Martin and Ellis, 1930). Following the analysis of over 3000 FNAB of palpable mammary lesions by Franzén and Zajicek (1968), this noninvasive method was used to replace diagnostic excision biopsy. Until the early 1990s, this was the only established minimally invasive method available for making a preoperative diagnosis of mammary carcinoma. FNAB essentially yields single cells and cell clusters, and only in rare cases also tiny pieces of tissue. For this reason, one of the most important criteria in pathologic diagnosis—the evaluation of invasive growth—cannot be used here. FNAB is based on the recognition of malignant cells, without the possibility of evaluating their relationship to the surrounding tissue. The method thus requires that the evaluating cytologist has special training and the corresponding experience and expertise in histologic diagnosis. The cytologic criteria of malignancy (Table 12.1) vary in their expression, both qualitatively and quantitatively. This makes it necessary that the evaluating cytologist considers the findings carefully and matches them consistently to the clinical and imaging findings using the triple approach (physical examination, mammography, and FNA cytology). Palpable tumors are the domain of FNAB. The method is less effective for the diagnosis of small, nonpalpable tumors, even under ultrasonic or stereotactic guidance, and even less so in cases of architectural distortion and microcalcification of the tissue.
Basics of Cytologic Diagnosis
History
Material and Criteria
Criterion | Expression |
Cell count | High |
Cell arrangement | Overlapping 3D |
Cell types | Uniform |
Cells with naked nuclei | Missing |
Background | Necrotic material, desmoplastic stroma |
Size of nuclei | Variable, mostly increased |
Nuclear pleomorphy | Severe |
Nuclear demarcation | Irregular |
Nucleoli | Mostly prominent, often multiple |
Chromatin structure | Irregular, clumpy |
C Categories
The aim of the cytologic examination is to differentiate between benign and malignant lesions as accurately as possible. The histologic findings of both types of lesions vary considerably, and the same is true for the cytologic material obtained by FNAB. Difficulties with interpretation not only occur because of insufficient yield of cells. To better understand the results of FNAB, the following C categories for cytologic malignancy have been published and recommended for the screening program (NHSBSP, 1992; Shabot et al, 1982). In addition to the verbal diagnosis, they should help determine—unambiguously and for all persons involved—the various degrees of reliability of the statement.
C1—Inadequate (Insufficient Material)
Inadequate aspirates include:
 samples with very few cells and with less than five cell clusters
samples with very few cells and with less than five cell clusters
 compromised samples (too bloody material, very thick smears, air-drying artifacts, and the like)
compromised samples (too bloody material, very thick smears, air-drying artifacts, and the like)
The reasons for classification as C1 should always be stated.
C2—Benign
Benign aspirates are moderately rich in cells. They may contain cohesive clusters of uniform epithelial cells with bland cytologic properties, naked bipolar cells (myoepithelial cells), and stromal fragments. Cystic lesions may contain, in addition to the above, apocrine cells with nuclei of various sizes and prominent nucleoli and with a distinctly eosinophilic, granulated cytoplasm, as well as foam cells, cell detritus, and microcalcification.
Category C2 requires a minimum amount of five cell clusters. Some findings, such as fatty tissue necrosis, fibroadenoma, lymph nodes, abscesses, and granuloma may permit a definitive diagnosis based on their cytology.
C3—Equivocal / Atypia Probably Benign
Equivocal aspirates may show all findings listed under C2. In addition, the following changes are observed, either individually or in combination: high cell density, polymorphic nuclei, loss of cohesion, reduction in the number of cells with naked nuclei, and nuclear changes due to proliferation, involution, or lactation.
C4—Suspicious of Malignancy
This category includes atypical findings highly suspicious of malignancy, but do not permit a definite diagnosis of malignant growth. Three principal constellations of findings prompt classification as C4:
 highly atypical cells present in low numbers or in a cohesive arrangement
highly atypical cells present in low numbers or in a cohesive arrangement
 cell-rich benign aspirate with solitary, but highly atypical cells
cell-rich benign aspirate with solitary, but highly atypical cells
 compromised aspirate with recognizable, highly atypical cells All atypical criteria in this group surpass the ones listed under C3; nuclear criteria are identical to those under C5.
compromised aspirate with recognizable, highly atypical cells All atypical criteria in this group surpass the ones listed under C3; nuclear criteria are identical to those under C5.
C5—Malignant
This category indicates that the aspirate is derived from a malignant tumor. The atypical cells meet all criteria of malignancy (Table 12.1) and are present in high numbers. Incomplete fulfillment of malignancy criteria and low cell numbers exclude classification as C5.
Quality Indicators for Cytologic Diagnosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree