3 Degenerative Changes
Degenerative Arthritis
Primary Degenerative Arthritis (Figs. 3.1, 3.3)
Osteoarthritis of the Shoulder
Definition
A primary osteoarthritis refers to a genetic, age-related, or function-related articular degeneration of a normally developed joint with altered microscopic and macroscopic anatomy that reflects wear and tear and consecutive functional impairment. This is observed as increasing destruction of cartilage and transformation of bone such as sclerosis, osteophytes, and cysts, possibly also as inflammatory changes of the surrounding soft tissues.
Pathology
 Macroscopic:
Macroscopic:
– Joint-space narrowing
– Osteophytes
– (Detrital) cysts
– Subchondral sclerosis
– Cortical irregularity
– Chondral abrasions
– Joint effusion
– Upward displacement of the humeral head
 Microscopic:
Microscopic:
– Splitting of the articular cartilage
– Chondral abrasions
– Chondrocytic regeneration
– Hyperostotic endplate transformation
– Osteonecroses/detrital cysts
– Replacement of hyaline cartilage with fibrocartilage
– Hypertrophy and atrophy of the synovial villi
– Reactive inflammatory muscle and tendon changes
Clinical Findings
 Feeling of tension
Feeling of tension
 Articular stiffness
Articular stiffness
 Pain on initiation of motion and with weight bearing
Pain on initiation of motion and with weight bearing
 Limitation of motion
Limitation of motion
 Muscle atrophy and contracture
Muscle atrophy and contracture
 Tendon lesions, including tear
Tendon lesions, including tear
 Crepitation
Crepitation
 Joint swelling and effusion
Joint swelling and effusion
 Articular malposition and mutilation
Articular malposition and mutilation
Diagnostic Evaluation
 (→ Method of choice)
(→ Method of choice)
Recommended views
 Standard projections:
Standard projections:
– Anteroposterior (AP) projection relative to scapula
– Tangential glenoid projection
– Axial projection
– Transscapular (“Y”) projection
– Transthoracic projection
– Oblique apical projection
 Special projections:
Special projections:
– Tangential projection of the humeral head according to Hill-Sachs-Chuinard
– AP projection in abduction or elevation and external rotation (Stryker’s notch view)
– Supraspinatus outlet view
– West Point view
– Tangential view of the bicipital groove
 Conventional tomography:
Conventional tomography:
– To visualize articular destruction, cysts, and loose bodies
Findings
 Joint-space narrowing
Joint-space narrowing
 Osteophytes
Osteophytes
 Detrital cysts
Detrital cysts
 Subchondral sclerosis
Subchondral sclerosis
 Cortical irregularity
Cortical irregularity
 Joint effusion
Joint effusion
 Upward migration of the humeral head
Upward migration of the humeral head
 Old traumatic lesions (Hill-Sachs or Bankart lesion)
Old traumatic lesions (Hill-Sachs or Bankart lesion)
 Loose bodies
Loose bodies
 Tendon and muscle calcifications
Tendon and muscle calcifications
 (→ Supplementary method)
(→ Supplementary method)
Recommended planes
 Posterior axial and longitudinal section
Posterior axial and longitudinal section
 Lateral coronal section
Lateral coronal section
 Anterior and anteromedial axial section
Anterior and anteromedial axial section
 Longitudinal section over the AC joint
Longitudinal section over the AC joint
Findings
 Joint-space narrowing
Joint-space narrowing
 Osteophytes
Osteophytes
 Joint effusion
Joint effusion
 Old traumatic lesions (Hill-Sachs or Bankart lesion)
Old traumatic lesions (Hill-Sachs or Bankart lesion)
 Possibly loose bodies
Possibly loose bodies
 Tendon and muscle calcifications
Tendon and muscle calcifications
 (→ Supplementary method)
(→ Supplementary method)
Recommended protocol (See p. 16, Standard Parameters)
 Standard computed tomography (CT):
Standard computed tomography (CT):
– Section thickness: 1–2 mm
– Table feed: 1–2 mm
 Spiral CT:
Spiral CT:
– Section thickness: 1–2 mm
– Table feed: 2–5 mm
– Increment: 1–2 mm
– Sagittal and coronal 2-D reconstruction
– Possibly 3-D reconstruction
Findings
 Joint-space narrowing
Joint-space narrowing
 Osteophytes
Osteophytes
 Detrital cysts
Detrital cysts
 Destruction of the articular surface
Destruction of the articular surface
 Old traumatic lesions (Hill-Sachs or Bankart lesion)
Old traumatic lesions (Hill-Sachs or Bankart lesion)
 Possibly loose bodies
Possibly loose bodies
 Extent of tendon and muscle calcifications
Extent of tendon and muscle calcifications
Goals of Imaging
 Visualization of the osseous anatomy of the humeral head
Visualization of the osseous anatomy of the humeral head
 Visualization of its relationship to the glenoid process
Visualization of its relationship to the glenoid process
 Visualization of its relationship to the acromion (acromio-humeral distance, AHD)
Visualization of its relationship to the acromion (acromio-humeral distance, AHD)
 Visualization of the osseous anatomy of the glenoid fossa (anterior and posterior blunting)
Visualization of the osseous anatomy of the glenoid fossa (anterior and posterior blunting)
 Evaluation of the rotator cuff (tendon degeneration, partial tear of the bursal or articular surface, tendon retraction with full-thickness tear, muscle degeneration with chronic tear)
Evaluation of the rotator cuff (tendon degeneration, partial tear of the bursal or articular surface, tendon retraction with full-thickness tear, muscle degeneration with chronic tear)
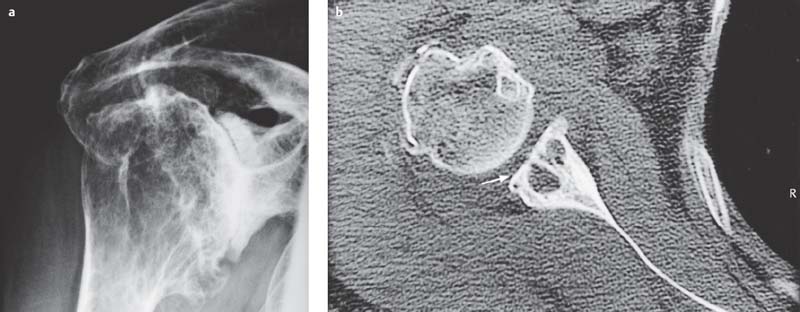
Fig. 3.1 a, b  Primary osteoarthritis of the glenohumeral articulation
Primary osteoarthritis of the glenohumeral articulation
Primary osteoarthritis of the right shoulder with obliteration of the glenohumeral joint space, osteophytes of the humeral head, cystic and sclerotic changes of the joint-forming osseous structures, and deformity of the glenoid process and humeral head (tangential view of the glenoid process) (a). CT of another patient also shows severe osteoarthritic changes with definite cyst formation in the glenoid process (b, arrow).

Fig. 3.2  Prosthetic replacement
Prosthetic replacement
Advanced osteoarthritis with severe clinical problems is an indication for prosthetic replacement (AP view of the right shoulder).
Therapeutic Principles
Depends on the patient’s age, severity of the osteoarthritis, and clinical complaints (Fig. 3.2)
Conservative
 Analgesics
Analgesics
 Physical therapy
Physical therapy
 Local/intra-articular injections/infiltration with analgesics/corticosteroids
Local/intra-articular injections/infiltration with analgesics/corticosteroids
Surgical
 Arthroscopy
Arthroscopy
 Arthroscopic subacromial decompression (ASD)
Arthroscopic subacromial decompression (ASD)
 Open subacromial decompression
Open subacromial decompression
 Rotator-cuff reconstruction
Rotator-cuff reconstruction
 Prosthesis
Prosthesis
 (→ Supplementary method)
(→ Supplementary method)
Recommended sequences
 Short time inversion recovery (STIR) sequence
Short time inversion recovery (STIR) sequence
 T1-and T2-weighted turbo spin-echo (TSE) or gradient-echo (GE) sequences (possibly with fat suppression)
T1-and T2-weighted turbo spin-echo (TSE) or gradient-echo (GE) sequences (possibly with fat suppression)
 Administration of contrast medium to detect inflammatory changes and their extent
Administration of contrast medium to detect inflammatory changes and their extent
Findings
 Unenhanced T1 -weighted sequence:
Unenhanced T1 -weighted sequence:
– Hypointense visualization of osteophytes
– Hypointense visualization of detrital cysts
– Hypointense visualization of loose intra-articular bodies
– Hypointense visualization of calcifications
– Hyperintense visualization of fatty transformation within bones and soft tissues
 T2-weighted spin-echo (SE) sequence:
T2-weighted spin-echo (SE) sequence:
– Hyperintense visualization of detrital cysts
– Hyperintense visualization of inflammatory changes(activeosteoarthritis)
– Hypointense visualization of loose intra-articular bodies
– Hypointense visualization of calcifications
– Hyperintense visualization of joint effusion
– Hyperintense visualization of fatty transformation within bones and soft tissues
 GE sequence:
GE sequence:
– Cartilage thinning, ulceration, denudation
– Hyperintense visualization of fatty transformation within bones and soft tissues (with fat suppression, hypointense visualization)
 Enhanced T1-weighted sequences:
Enhanced T1-weighted sequences:
– Hypointense visualization of osteophytes
– Hypointense visualization of detrital cysts
– Hyperintense visualization of inflammatory changes (activeosteoarthritis)
– Hypointense visualization of loose intra-articular bodies
– Hypointense visualization of calcifications
– Hyperintense visualization of fatty transformation within bones and soft tissues (with fat suppression, hypo-intense visualization)
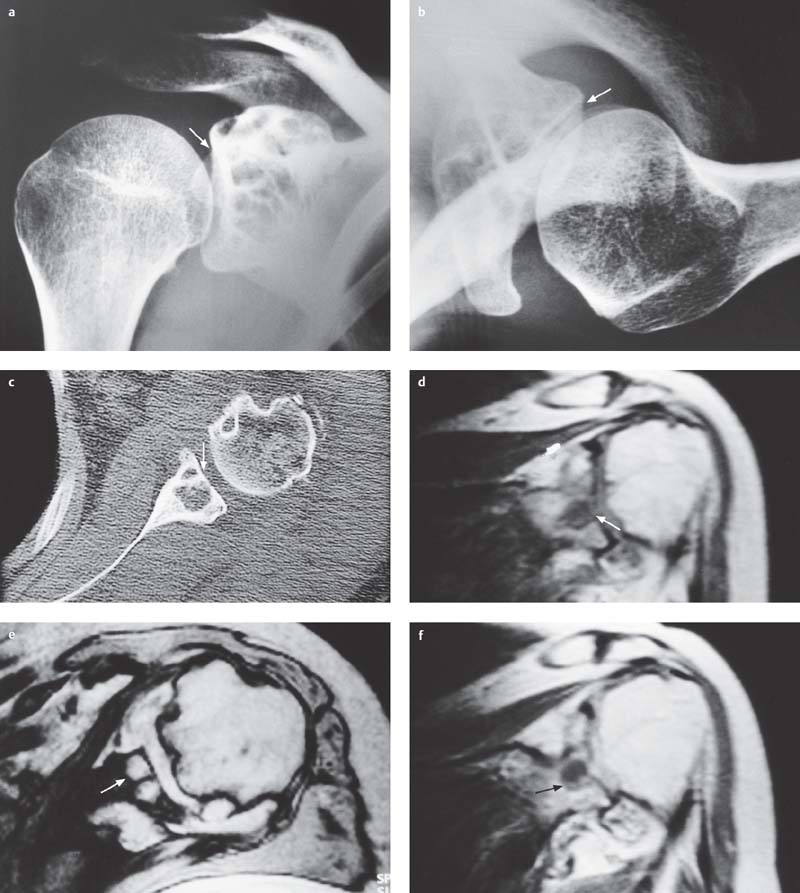
Fig. 3.3 a–f  Degenerative changes in the glenoid process with cyst formation
Degenerative changes in the glenoid process with cyst formation
Degenerative changes in the glenoid process and extensive degenerative and/or genuine cyst formation.
a, b Already tangential (a, arrow) and axial (b, arrow) radiographic views of the glenoid process show multiple cysts in the glenoid process and subchondral sclerosis and articular irregularities of the glenoid fossa.
c Axial CT demonstrates the extent of the cystic changes (arrow) in the glenoid process and in the anterior humeral head to better advantage.
d-f Furthermore, magnetic resonance imaging (MRI) clearly shows the cystic component of the degenerative changes in the glenoid process, which are hypointense on the sagittal T1-weighted sequence (d, arrow) and hyperintense on the axial gradient-echo (GE) sequence (fast low angle shot [FLASH] 2-D; e, arrow). Contrast enhancement is at most discrete rim-like or reactive around the cyst (f, enhanced T1-weighted, arrow). In addition, the T1-weighted sequence (d) shows early osteophytic apposition at the rotator-cuff insertion in the region of the major tuberosity and hyperintense degeneration of the supraspinatus tendon in the subacromial space as seen in impingement syndrome. The humeral head is already migrated upward as seen with rotator-cuff insufficiency.
Degeneration of the Acromioclavicular (AC) Joint (AC Osteoarthritis)
Therapeutic Principles
Depends on the patient’s age, severity of osteoarthritis, clinical complaints
Conservative
 Analgesics
Analgesics
 Physical therapy
Physical therapy
 Local/intra-articular injections/infiltration with analgesics/corticosteroids
Local/intra-articular injections/infiltration with analgesics/corticosteroids
Surgical
 Arthroscopic resection of the AC joint (ARAC)
Arthroscopic resection of the AC joint (ARAC)
 Open AC resection
Open AC resection
Definition
Usually occurs with primary osteoarthritis of the AC joint together with osteoarthritis of the glenohumeral joint. The changes of the microscopic and macroscopic anatomy are the same as described at the beginning of this chapter (see p. 57).
Pathology
 Macroscopic:
Macroscopic:
– Joint-space narrowing
– Osteophytes
– Rarely (detrital) cysts
– Rarely and mostly slight joint effusion
– Subchondral sclerosis
– Cortical irregularity
 Microscopic:
Microscopic:
– Hyperostotic endplate transformation
– Osteonecroses/detrital cysts
– Apposition of fibrocartilage
– Reactive inflammatory tendon changes
– Subacromial rotator-cuff impingement
Clinical Findings
 Joint stiffness
Joint stiffness
 Pain on initiation of motion and with weight bearing, point tenderness
Pain on initiation of motion and with weight bearing, point tenderness
 Functional impairment
Functional impairment
 Rotator-cuff lesions (especially of the supraspinatus muscle and its tendon), including tear
Rotator-cuff lesions (especially of the supraspinatus muscle and its tendon), including tear
 Crepitation
Crepitation
 Joint swelling and effusion
Joint swelling and effusion
 Articular malposition and mutilation
Articular malposition and mutilation
Diagnostic Evaluation
 (→ Method of choice)
(→ Method of choice)
Recommended views
 Standard projections:
Standard projections:
– AP projection relative to scapula
– Axial projection
– Oblique apical projection
 Special projections:
Special projections:
– Supraspinatus outlet view
– West Point view
– Oblique view of the AC joint
– Tangential view of the bicipital groove
– Special view according to Janda
 Conventional tomography:
Conventional tomography:
– To visualize articular destruction, cysts, and old fragments
Findings
 Joint-space narrowing
Joint-space narrowing
 Osteophytes
Osteophytes
 Cysts
Cysts
 Subchondral sclerosis
Subchondral sclerosis
 Cortical irregularity
Cortical irregularity
 Old traumatic lesions, old fragments
Old traumatic lesions, old fragments
 Tendon and muscle calcifications
Tendon and muscle calcifications
 (→ Supplementary method)
(→ Supplementary method)
Recommended planes
 Longitudinal section over the AC joint
Longitudinal section over the AC joint
Findings
 Joint-space narrowing
Joint-space narrowing
 Osteophytes
Osteophytes
 Joint effusion
Joint effusion
 Possibly old fragments
Possibly old fragments
 Tendon and muscle calcifications
Tendon and muscle calcifications
 (→ Supplementary method)
(→ Supplementary method)
Recommended protocol
 Standard CT:
Standard CT:
– Section thickness: 1–2 mm
– Table feed: 1–2 mm
 Spiral CT:
Spiral CT:
– Section thickness: 1–2 mm
– Table feed: 2–5 mm
– Increment: 1–2 mm
– Sagittal and coronal 2-D reconstruction
– Possibly 3-D reconstruction
Findings
 Joint-space narrowing
Joint-space narrowing
 Osteophytes
Osteophytes
 Cysts
Cysts
 Destruction of the articular surface
Destruction of the articular surface
 Old traumatic lesions (fragments)
Old traumatic lesions (fragments)
 Extent of tendon and muscle calcifications
Extent of tendon and muscle calcifications
 (→ Supplementary method, together with visualization of the shoulder)
(→ Supplementary method, together with visualization of the shoulder)
Recommended sequences
 STIR sequence
STIR sequence
 T1-and T2-weighted TSE or GE sequences (possibly with fat suppression)
T1-and T2-weighted TSE or GE sequences (possibly with fat suppression)
 Administration of contrast medium to detect inflammatory changes and their extent
Administration of contrast medium to detect inflammatory changes and their extent
Findings (Fig. 3.4)
 Unenhanced T1-weighted sequence:
Unenhanced T1-weighted sequence:
– Hypointense visualization of osteophytes
– Hypointense visualization of cysts
– Hypointense visualization of old fragments
– Hypointense visualization of calcifications
– Hyperintense visualization of fatty transformation within bones and soft tissues
 T2-weighted SE sequence:
T2-weighted SE sequence:
– Hyperintense visualization of cysts
– Hyperintense visualization of inflammatory changes (active osteoarthritis)
– Hypointense visualization of old fragments
– Hypointense visualization of calcifications
– Hyperintense visualization of fatty transformation within bones and soft tissues
 GE sequence:
GE sequence:
– Cartilage damage
– Hyperintense visualization of fatty transformation within bones and soft tissues (with fat suppression, hypointense visualization)
 Enhanced T1-weighted sequences:
Enhanced T1-weighted sequences:
– Hypointense visualization of osteophytes
– Hypointense visualization of cysts
– Hyperintense visualization of inflammatory changes (active osteoarthritis)
– Hypointense visualization of old fragments
– Hypointense visualization of calcifications
– Hyperintense visualization of fatty transformation within bones and soft tissues (with fat suppression, hypointense visualization)
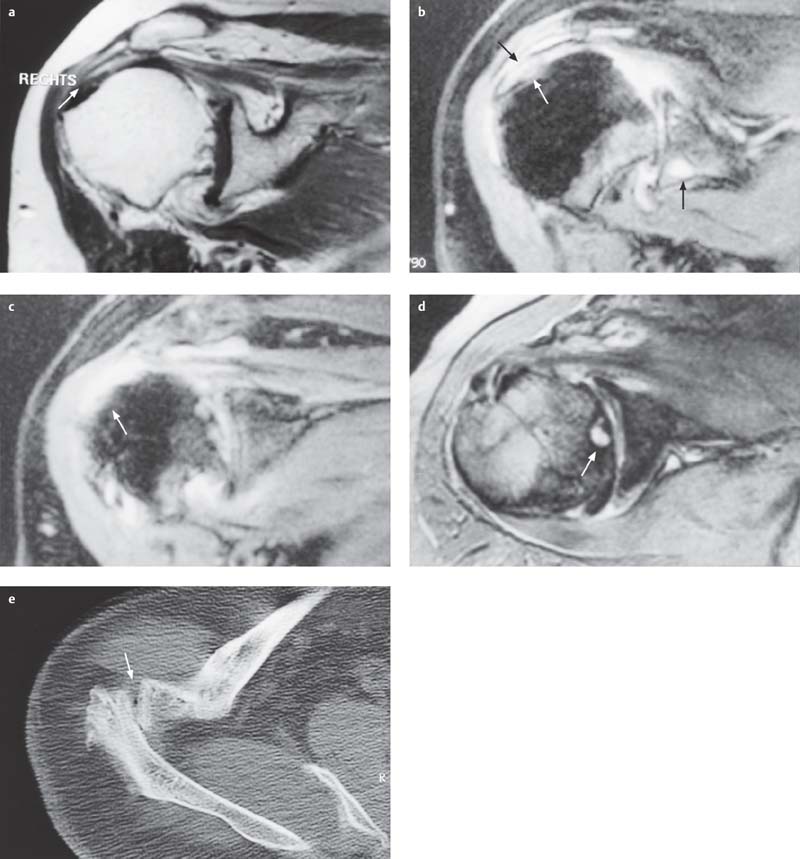
Fig. 3.4 a–e  AC osteoarthritis
AC osteoarthritis
In addition to impingement of the rotator cuff in the subacromial space in the presence of AC osteoarthritis, the shoulder exhibits definite reactive inflammatory changes, with degenerative destruction of the supraspinatus tendon (long arrow) and detrital cysts in the glenoid process (short arrow) (a, T1-weighted sequence, intravenous injection of 15 mL Magnevist, oblique coronal section; b, fat-saturated proton density-weighted sequence, oblique section), as well as osseous changes of the tendinous insertion at the major tuberosity (c, fat-saturated proton density-weighted sequence, oblique section, arrow).
In addition, degenerative changes are seen at the glenoid labrum and detrital cysts in the humeral head (d, GE sequence, flip angle 25°, TR 700 ms, TE 20 ms, axial section, arrow).
The axial CT section (e) shows the osteoarthritic deformity of the AC joint (arrow).
Secondary Osteoarthritis (Fig. 3.5)
Definition
A secondary osteoarthritis arises on the basis of congenital articular dysplasia, metabolic disorders (articular chondro-dystrophy), preceding trauma, or inflammation. The arthropathy induced by a rotator-cuff defect represents a unique entity of the shoulder. In addition to the resultant deformity of degenerated and eroded articular cartilage as manifestation of the underlying primary osteoarthritis, the microscopic and macroscopic anatomy shows subchondral cortical sclerosis and destruction as well as possibly reactive inflammatory synovial changes.
Pathology
 Macroscopic:
Macroscopic:
– Joint-space narrowing
– Osteophytes
– (Detrital) cysts
– Subchondral sclerosis
– Cortical irregularity
– Chondral abrasions
– Joint effusion
– Rotator-cuff tear
– Upward displacement of the humeral head
 Microscopic:
Microscopic:
– Splitting of the articular cartilage
– Chondral abrasions
– Chondrocytic regeneration
– Hyperostotic endplate transformation
– Osteonecroses/detrital cysts
– Replacement of hyaline cartilage with fibrocartilage
– Hypertrophy and atrophy of the synovial villi
– Reactive inflammatory muscle and tendon changes
– Possibly inflammatory changes of rheumatoid arthropathies
Clinical Findings
 Feeling of tension
Feeling of tension
 Joint stiffness
Joint stiffness
 Pain on initiation of motion and with weight bearing
Pain on initiation of motion and with weight bearing
 Nocturnal pain
Nocturnal pain
 Restricted function
Restricted function
 Muscle atrophy and contracture
Muscle atrophy and contracture
 Tendon lesions, including tear
Tendon lesions, including tear
 Crepitation
Crepitation
 Joint swelling and effusion
Joint swelling and effusion
 Articular malposition and mutilation
Articular malposition and mutilation
 Dysfunction
Dysfunction
Diagnostic Evaluation
 (→ Method of choice)
(→ Method of choice)
Recommended views
 Standard projections:
Standard projections:
– AP projection relative to scapula
– Tangential glenoid projection
– Axial projection
– Transscapular (“Y”) projection
– Transthoracic projection
– Oblique apical projection
 Special projections:
Special projections:
– Tangential projection of the humeral head according to Hill-Sachs-Chuinard
– AP projection in abduction or elevation and external rotation (Stryker’s notch view)
– Supraspinal outlet view
– West Point view
– Tangential view of the bicipital groove
 Conventional tomography:
Conventional tomography:
– To visualize articular destruction, cysts, and loose bodies
Findings
 Joint-space narrowing
Joint-space narrowing
 Osteophytes
Osteophytes
 Detrital cysts
Detrital cysts
 Subchondral sclerosis
Subchondral sclerosis
 Cortical irregularity
Cortical irregularity
 Joint effusion
Joint effusion
 Upward migration of the humeral head
Upward migration of the humeral head
 Old traumatic lesions (Hill-Sachs or Bankart lesion)
Old traumatic lesions (Hill-Sachs or Bankart lesion)
 Loose bodies
Loose bodies
 Tendon and muscle calcifications
Tendon and muscle calcifications
 Posttraumatic or postinflammatory destruction or step deformity of the articular surface
Posttraumatic or postinflammatory destruction or step deformity of the articular surface
 Dislocation or subluxation
Dislocation or subluxation
 Osseous destruction
Osseous destruction
 Rotatory or axial malpositions
Rotatory or axial malpositions
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


