Fig. 18.1
PDE imaging system
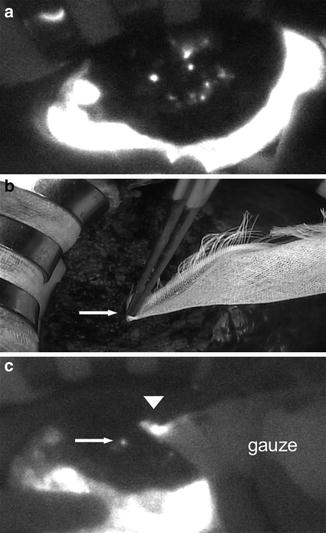
Fig. 18.2
Fluorescent images obtained using the PDE system. (a) White spots (possible bile leakage) on the cut surface of the liver. (b) Minor leakage (leaking duct) that is not visible to the surgeons (arrow) is compressed with gauze. (c) Fluorescent imaging after the application of gauze shows minor leakage on the cut surface of the liver (arrow), as fluorescence is detected through the gauze (arrowhead). With permission from Kaibori M, Ishizaki M, Matsui K, Kwon AH. Intraoperative indocyanine green fluorescent imaging for prevention of bile leakage after hepatic resection. Surgery 2011; 150: 91–8 (25)
Postoperative bile leakage (Fig. 18.3) was diagnosed by the following findings: detection of bile leakage from the wound or through the drainage tube (total bilirubin level in the drainage fluid >3 times the serum level), intra-abdominal accumulation of bile confirmed by drainage, or demonstration of bile leakage on postoperative cholangiography.
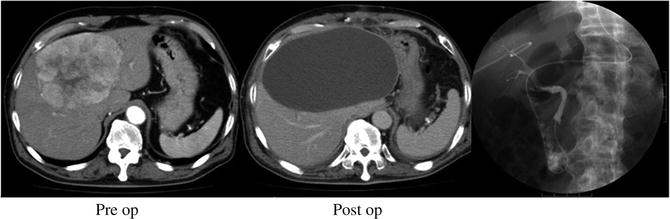
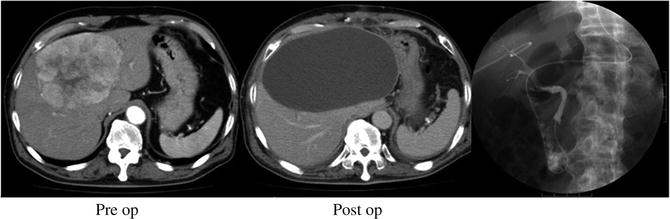
Fig. 18.3
Patient with postoperative bile leakage. A 67-year-old male underwent extended left hemihepatectomy for hepatocellular carcinoma. He was discharged uneventfully on postoperative day 12, and was readmitted on postoperative day 22 with severe abdominal pain and persistent fever. His bile leakage was treated by abdominal paracentesis and endoscopic biliary drainage, and was resolved on postoperative day 72
Results
Thirty-two of the 132 patients (24 %) had major leakage of ICG, defined as leakage of green dye without fluorescent imaging. Repair was performed by z-suturing with 6-0 non-absorbable sutures in 28 patients, and by ligation with 4-0 absorbable sutures in 4 patients. The leaks were all successfully repaired during surgery, and were further tested with fluorescent imaging.
Patterns of Fluorescence
In 37 of the 132 patients (19 %), no fluorescence was detected on the cut surface of the remnant liver on ICG fluorescent cholangiography, suggesting absence of bile ducts at the surgical margin (Type A pattern of fluorescence). In the remaining 95 patients, the pattern of fluorescence was classified into the following three types: intact bile duct type (Type B, fluorescence showed one or more intact bile ducts on the cut surface of the liver; n = 51) (Fig. 18.4), injured bile duct type (Type C, leakage of dye from one or more bile duct stumps on the cut surface; n = 31) (Fig. 18.5), and unconfirmed type (Type D, leakage of dye from the cut surface, but the source was unclear; n = 13) (Fig. 18.6 and Video 18.2). In Type D pattern, the minor dye leaks could not be visualized by the surgeon, and could only be detected by viewing the fluorescent images on the monitor.
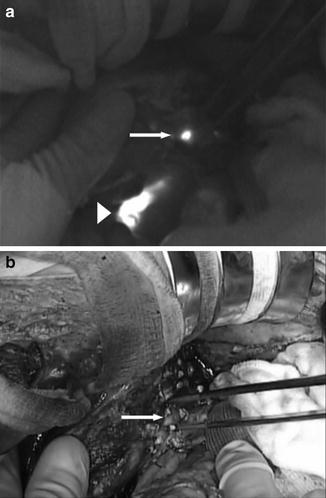
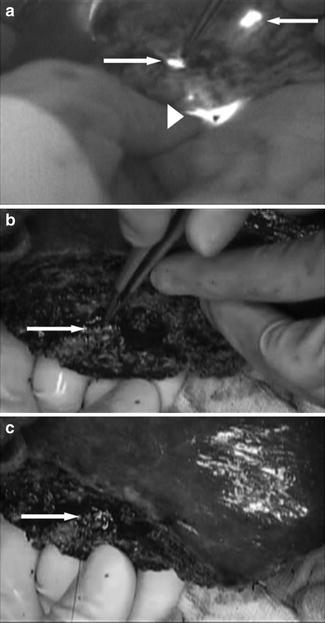
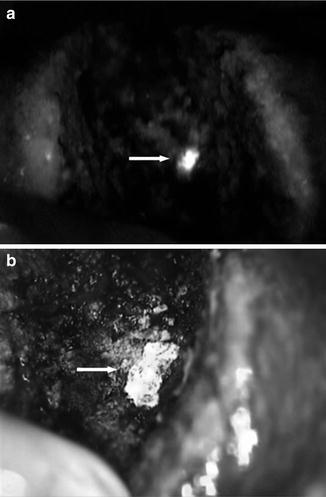
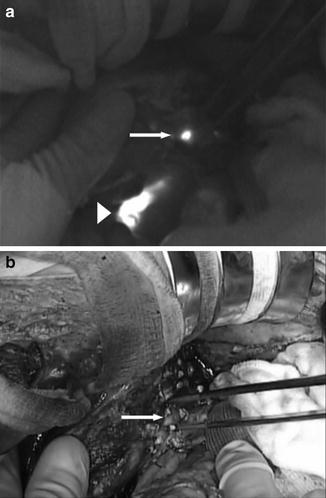
Fig. 18.4
Type B pattern of fluorescence (intact bile duct type). (a) Fluorescent imaging showed one fluorescent duct on the cut surface of the liver (arrow). Arrowhead: common bile duct. (b) There was an intact bile duct corresponding to the fluorescent area on the cut surface (arrow). With permission from Kaibori M, Ishizaki M, Matsui K, Kwon AH. Intraoperative indocyanine green fluorescent imaging for prevention of bile leakage after hepatic resection. Surgery 2011; 150: 91–8 (25)
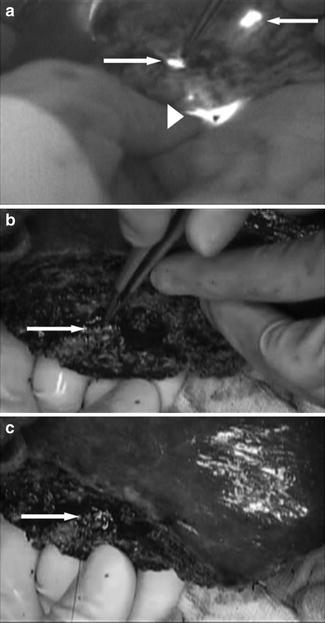
Fig. 18.5
Type C pattern of fluorescence (injured bile duct type). (a) Fluorescent imaging showed two areas of fluorescence corresponding to ducts on the cut surface of the liver (arrows). The upper bile duct was intact (upper arrow). Arrowhead: common bile duct. (b) The lower area of fluorescence corresponded to a partly closed bile duct stump (arrow). (c) The bile duct stump was repaired by z-suturing with 6-0 nonabsorbable sutures (arrow). With permission from Kaibori M, Ishizaki M, Matsui K, Kwon AH. Intraoperative indocyanine green fluorescent imaging for prevention of bile leakage after hepatic resection. Surgery 2011; 150: 91-8 (25)
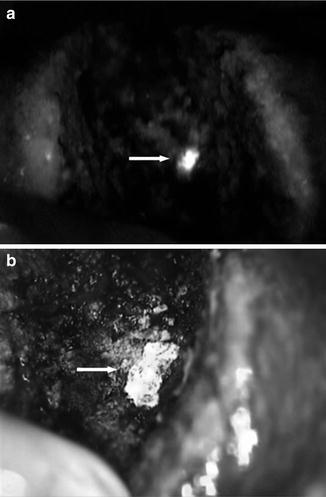
Fig. 18.6
Type D pattern of fluorescence (unconfirmed type). (a) Fluorescent imaging showed an area of fluorescence on the cut surface of the liver (arrow). (b) Fibrin sealant was applied to the fluorescent area (arrow). With permission from Kaibori M, Ishizaki M, Matsui K, Kwon AH. Intraoperative indocyanine green fluorescent imaging for prevention of bile leakage after hepatic resection. Surgery 2011; 150: 91–8 (25)
No repair was performed in patients with Type A pattern of fluorescence. In patients with Type B pattern, repair was performed by z-suturing with 6-0 non-absorbable sutures in 42 patients (1.5 ± 0.8 (mean ± SD) sutures per patient) and by ligation with 4-0 absorbable sutures in the remaining nine patients (1.0 ± 0.2 ligatures per patient). In the three patients with Type D pattern, fibrin sealant was applied to the area showing leakage (two pieces of 2.0 × 1.5 cm sealant per patient). The fluorescence imaging findings were used to guide treatment in the patients with Type D pattern.
Postoperative Bile Leakage
Postoperative bile leakage occurred in 7 of the 132 hepatectomy patients (5 %) and persisted for a median period of 6 weeks (range, 2–15 weeks). Table 18.1 shows the incidence of each pattern of fluorescence. The rate of Type D pattern differed from the rates of the other three patterns.
Table 18.1
Incidence of postoperative bile leakage for each pattern of fluorescence
Indocyanine green fluorescent imaging | Number of patients | Number with postoperative bile leakage | % | |
|---|---|---|---|---|
Type A | No fluorescence was detected on the cut surface | 37 | 0 | 0 |
Type B | Intact bile duct type | 51 | 1 | 2
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|