Abstract
Purpose
To evaluate the impact of patient, tumor and surgical factors affecting pre-radiotherapy (RT) aesthetic outcome.
Methods
The study cohort comprised of 377 patients planned for adjuvant RT from March 2020 to October 2021 after breast conserving surgery (BCS) at Tata Memorial Centre. Patient and physician rated cosmesis pre-RT and at each visit up to 2 years were recorded. Currently we report only pre-RT cosmetic outcome.
Results
The median size of breast, tumor-bed and breast-tumor ratio were 700 cc (130–1603), 80 cc (17.9–216) and 11.68% (1.88–34.07) respectively. Oncoplastic breast surgery (OPBS) was done in 40.8% patients, 23% patients had prior history of breast surgery while post-operative complications were documented in 4.5%. The proportion of excellent-good (E-G) cosmesis was 80%, 74.5% and 69.7% by physician, patients and BCCT.core (Breast Cancer Conservation Treatment. cosmetic results) respectively.
On multivariate analysis, overall cosmesis by physician was found to be better in women with large breast (p-0.002, OR-0.431, CI 0.253–0.735); without prior history of breast surgery (p-0.007, OR-0.456, CI 0.257–0.809); and age less than 60 years (p-0.019, OR-2.492, CI 1.162–5.344). According to patient reported outcome, breast-tumor ratio (p-0.038, OR-1.04, CI 1.002–1.079) and post operative complication (p-0.025, OR-3.2, CI 1.15–8.85) were the predominant factors affecting overall cosmesis. Favorable cosmesis by BCCT.core was attributed to age less than 60 years (p-0.013, OR-2.366, CI 1.162–4.816) and prior history of breast surgery (p-0.022, OR-0.427, CI 0.206–0.886).
Conclusion
Large majority of patients have E-G cosmetic outcome. Various patient and tumor related factors were found to correlate with it.
Highlights
- •
Vos scale is a reliable method for subjective assessment of cosmesis.
- •
BCCT.core, an objective method of cosmetic evaluation using breast photographs is comparable well with the physician rating.
- •
The factors like smaller breast size, older age, higher breast-tumor ratio adversely affected pre-RT cosmetic outcome.
- •
Surgical factors like presence of postoperative complications and prior history of breast surgery worsened cosmetic outcome.
- •
It is important to document pre-RT outcome for future longitudinal evaluation of cosmetic worsening.
- •
This will help to evaluate the differential role of surgical and radiotherapeutic factors in worsening of cosmesis.
1
Introduction
Numerous randomized trials have established the oncological safety of breast-conservation therapy (BCT). BCT comprises of breast conserving surgery (BCS) and adjuvant radiotherapy (RT) of the conserved breast [ , ]. Although its non-inferiority to mastectomy has been proven for early-stage breast cancer, BCT is also offered in locally advanced breast cancer (LABC) [ ]. Patients with LABC who have good response to neoadjuvant systemic therapies become amenable to BCS [ , ]. Achieving an optimal balance between oncological safety and aesthetic outcomes is of paramount importance in such cases.
With advancements in surgical and oncoplastic techniques, it is now possible to offer BCS to increasing numbers of patients. Oncoplastic procedures range from simple closure of tumor cavity to complex procedures involving tissue rearrangements, with or without the use of local or free flaps. Local control and reoperation rates in oncoplastic surgery are comparable to those of conventional open cavity surgery [ ]. Breast conservation leads to better quality of life and improved psychological well-being because the procedure is less disfiguring than mastectomy [ ]. Oncoplastic breast surgery (OPBS) has increased the BCS eligibility because it is now possible to conserve breast in patients with multiple tumors or unfavorable breast-tumor ratios. Koppiker et al. recently published reports of extreme oncoplasty that showed encouraging aesthetic outcomes and high satisfaction [ ].
The overall cosmetic outcome of BCT relies not only on the interplay of different patient, tumor and treatment -related factors but also on the method by which cosmesis is assessed [ ]. Relating various therapeutic factors such as type of surgery, neoadjuvant chemotherapy, hormonal therapy, radiotherapy, etc with toxicity development and aesthetic outcome is important. Surgical and radiotherapeutic factors predominantly impact aesthetic outcomes though systemic therapies are also known to have an adverse impact on the same [ ]. Hence, we initiated a prospective longitudinal study to evaluate the temporal variation in aesthetic outcomes in a homogenous cohort of women who received whole breast radiation and tumor bed boosts at our institute. We report aesthetic outcomes collected prior to radiotherapy (referred to as the baseline). The objectives were to report the pre-RT cosmetic outcome and evaluate the various factors that affect it. This will serve as a baseline to analyze the temporal changes in cosmetic outcome following receipt of adjuvant radiotherapy.
2
Materials and methods
2.1
Study design
The study cohort comprised of 377 consecutive patients who were planned to receive adjuvant RT after BCS at Tata Memorial Center (TMC). This study was initiated in January 2020 with the aim of accruing patients planned for moderately hypofractionated RT (mHFRT) to the whole breast and tumor bed boosts. However, due to COVID-19 pandemic, we immediately adopted ultra-hypofractionated (uHFRT) regimens for all patients meriting adjuvant RT, as per international guidance [ ]. After the pandemic, mHFRT was resumed. As a result, this study comprises two cohorts: one treated with uHFRT and the other treated with mHFRT. We currently report pre-RT cosmetic outcomes in the patient cohort with uHFRT from March 2020 to July 2021. We have considered the pre-RT timepoint as baseline which is at least 4 weeks after surgery but prior to receiving radiotherapy.
The patients were accrued in this study after careful screening according to the inclusion and exclusion criteria mentioned in Table S1 , which is provided in the supplementary data.
2.2
Subjective rating of cosmetic outcome
Subjective assessment scales are simple, inexpensive, easier to use on routine basis, and do not require expertise. Patient and physician rated overall cosmesis using the method reported by Vos et al. [ ] were reported at baseline (pre-RT) i.e. at the time of radiation planning and on subsequent follow up visits. The photographs were acquired in three positions as described in “European Organization for Research and Treatment of cancer (EORTC) Boost versus No boost” trial [ ] as shown in Fig. 1 in the supplementary data.

Vos scale [ , ] consisting of 11 parameters was used for physician scoring. It consists of parameters like- Overall cosmetic result, Appearance of the surgical scar, Size of the breast, Shape of the breast, Position of the nipple-areola complex, Position of inframammary fold, Color of the skin, Telangiectasia and Symmetry. Telangiectasia is however not significant prior to radiotherapy. As medical terms like infra-mammary fold and telangiectasia are difficult for patients to understand, these were not reported by them. Therefore, they were excluded from the patient reported outcome. Instead, satisfaction with the appearance of breast and satisfaction from breast conserving surgery were captured. All of these parameters are given a score from 0 to 3 as defined by Harris et al. [ ] Here, 0 = excellent result (without visible treatment sequelae), 1 = good result (slight sequelae with minimal difference between treated and untreated breast), 2 = fair result (obvious difference between treated and untreated breast but without major distortion) and 3 = poor result (major aesthetic sequelae) as depicted in Fig. 1 .
The assessment was done using the frontal photographs, which is a gold standard method followed in randomized trials [ ]. A single physician rating was considered for the current analysis to rule out interobserver bias. Currently we report only baseline cosmetic outcome and factors impacting it. The early (1 and 2-year) and late (3 and 5-year) cosmetic outcomes will be reported in future as the cohort matures.
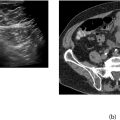
2.3
Objective rating of cosmetic outcome
Inter-observer discrepancies are known to occur in subjective assessment, and they can be excluded with an objective form of assessment. Another advantage is that a universal standard can be achieved. We have used BCCT.core [ ] software which is a computerized program developed by the Breast Research Group (INSEC Porto, the University of Porto), to objectively assess the aesthetic outcome of breast conservation treatment photographs. The BCCT.core analyzes several parameters related to asymmetry, color differences and scar appearance. BCCT.core [ ] software provides an objective method for the aesthetic evaluation of breast cancer conservative treatment that yields reproducible results.
2.4
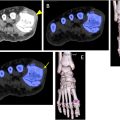
Estimation of breast and tumor bed volume
The patients underwent computed tomography (CT) simulation for radiotherapy planning. The target volumes of the breast were contoured on Treatment Planning System (TPS) according to Groupe Européen de Curiethérapie and the European SocieTy for Radiotherapy & Oncology (GEC-ESTRO) guidelines [ , ]. These comprised of Clinical target volume breast (CTV_BR), Planning Target volume breast (PTV_BR), Clinical target volume tumor bed (CTV_TB) and Planning Target Volume Tumor bed (PTV_TB). The Breast and tumor bed ratio (B:T) was calculated by dividing PTV_TB by CTV_BR. The CTV_BR has been used to estimate the breast size and the B:T ratio. The volumes were calculated on the Eclipse version 16.1 of Treatment planning system by Varian.
2.5
Statistical analysis
Patient demographics were reported as numbers and percentages. This includes clinico-pathological and surgical details. The rating of cosmesis was dichotomized into two categories and reported as a percentage of Excellent-Good (EG) and Fair-Poor (FP). The physician and patient rating were cross-tabulated using Cohen’s kappa statistics for interpreting agreement between the two as well as with the objective method. Univariate and multivariate analysis was carried out for the factors affecting the baseline cosmesis using Chi square test and linear regression modeling respectively in International Business Machines (IBM®) SPSS® software version 25.
3
Results
3.1
Demographic profile
The mean age of the study cohort was 46 years (SD-22 to 78), 52.3% of patients were premenopausal, and 87.3% of the population was literate. One-third (27.6%) of the patients had co-morbidities and only 2.7% of the patients were smokers/tobacco chewers. There were 56% of patients with left-sided breast cancer. The majority (80.6%) of the cohort had early clinical T-stage cT1-2, and 41.6% patients were clinically node negative. 15.4% belonged to Stage I of TNM staging, 61% belonged to Stage II and 23.6% belonged to Stage III. 31.5% of all underwent only axillary node sampling or sentinel lymph node biopsy. Remaining 68.5% comprised of axillary clearance I-III. The median size of the breast, tumor bed and breast tumor ratio were 700 cc (130–1603), 80 cc (17.9–216) and 11.68% (1.88–34.07) respectively. Supplementary Table S2 (provided in supplementary material) describes the demographic parameters of our cohort in detail. Open cavity surgery was done in 59.2% and oncoplastic breast surgery in 40.8%. Eighty-seven (23%) patients from the cohort presented with prior history of breast surgery, out of them 13.8% (12 out of 87) patients operated outside underwent only axillary dissection at our center due to adequate initial lumpectomy. The rate of re-excision of the primary was 14.2% (54 out of 377) in the overall study population but the same was 62% (54 out of 87) in the cohort with prior history of breast surgery. The remaining 38% (33 out of 87) patients had undergone complete breast conserving surgery outside. Around 4.5% of patients had post-operative complications like surgical site infection, hematoma or seroma. Out of the 17 patients having post-operative complications, 10 (58.8%) patients required secondary surgical intervention for these complications, while the rest were managed by conservative measures like antibiotic administration and wound care. The median time from date of surgery to date of radiotherapy simulation was 20 weeks. Only 13.5% patients received RT immediately after surgery while the rest received adjuvant chemotherapy followed by RT.
3.2
Baseline cosmesis data
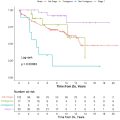
A total of 370 patients’ photographs were available for physician and patient assessment at baseline. Seven patients were excluded from assessment as frontal photographs were missing. In the overall group, the proportion of patients with E-G category as per physician, patient, and BCCT.core rating was 80%, 74.5%, and 69.7% respectively ( Table 1 and Fig. 2 ). There was no poor overall cosmesis according to the patient ( Fig. 2 ). The overall cosmesis rating according to physician was impacted by majority of factors except color of skin, and telangiectasia. Similarly, the overall cosmesis by patients was significantly contributed by all the components of rating as shown in Table 1 .
| Variable | Physician (N = 370) | P value | Patient (N = 370) | P value |
|---|---|---|---|---|
| Overall cosmetic result E-G | 296 (80%) | 276 (74.5%) | ||
| Appearance Scar | 321 (86.8%) | <0.001 | 239 (64.5%) | <0.001 |
| Size of breast | 319 (86.2%) | <0.001 | 241 (65%) | <0.001 |
| Shape of breast | 342 (92.4%) | <0.001 | 259 (70%) | <0.001 |
| Color of skin | 367 (99.2%) | 0.127 | 277 (74.8%) | <0.001 |
| Symmetry | 302 (81.6%) | <0.001 | 318 (85.9%) | <0.001 |
| Position NAC a | 294 (79.5%) | <0.001 | 257 (69.4%) | <0.001 |
| Position of IMF a | 345 (93.2%) | <0.001 | ||
| Telangiectasia | 370 (100%) | 1.0 |
a Abbreviations: NAC- Nipple-areola complex, IMF- Infra-mammary fold.

A physician will rate the treated breast as excellent cosmesis when its appearance is similar to that of untreated breast. But the patients do not know the objective standards a physician has in mind while assessing the cosmesis. As seen from the bar chart ( Fig. 2 ), 25.1% of patients were rated excellent cosmesis by physician but only 15% patients found their cosmesis as excellent.
3.3
Agreement between physician and patient reported outcome
Only slight concordance (kappa agreement 0.206, p value < 0.001) was observed between the overall cosmetic outcome of patient and physician ( Table 2 ). Agreement with objective score and physician rating was 0.348 (p value < 0.000).
| Comparison of Physician rating with Patient rating | Kappa | P-value |
|---|---|---|
| Overall cosmesis | 0.206 | <0.001 |
| Appearance of scar | 0.180 | <0.001 |
| Breast size | 0.120 | 0.006 |
| Breast shape | 0.054 | 0.151 |
| Color of skin | 0.025 | 0.103 |
| Symmetry | 0.197 | <0.001 |
| Position of NAC | 0.200 | <0.001 |
| BCCT.core overall score with physician rating | 0.348 | <0.001 |
| BCCT.core overall score with patient rating | 0.105 | 0.045 |
Breast size, location of nipple-areola complex and appearance of scar significantly contributed to overall cosmesis according to both patient and physician. While there was a discordance between patient and physician rating for the subjective domain of breast shape and color of skin.
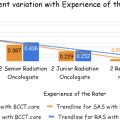
3.4
Univariate and multi-variate analysis
The results of multivariate linear regression analysis for physician rating showed that large breasted women had better overall cosmesis compared to small breasted women; women with an age less than 60 years had better cosmesis; and women undergoing single-stage surgery also experienced positive aesthetic results. Similarly, multivariate linear regression analysis for patient rating showed favorable aesthetic results for women with a lower breast-tumor ratio and women not having a history of post-operative complications. These bar charts shown in Fig. 3 a, b and 3c report the results in various subgroups.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree