Fig. 23.1
Gross appearance (a), macroscopic NIR fluorescence image (b), and X-ray CT image of the marker
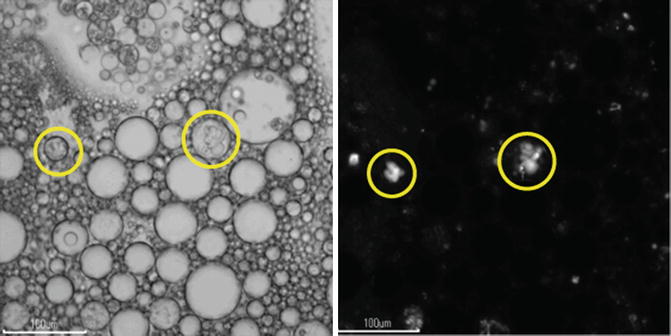
Fig. 23.2
Microscopic observation of the marker. (a) Phase contrast microscopy. (b) NIR fluorescence microscopy. Circles indicate vesicles which emit NIR fluorescence
In Vivo Analysis of the Marker
Next, we tested the usefulness of DI marker using a porcine model. Under the general anesthesia, gastroendoscopy of the pig was performed, and a metal clip was placed in each of the anterior and posterior sides of the middle stomach. Then, makers were injected into the submucosal layer at four points on a circumference of radius 1 cm around the clips. Approximately 300 μl of the marker was injected at each injection point. ICG aqueous solution of 64 μM was administered on the anterior side of the stomach and so did DI marker with the ICG-C18 concentration of 64 μM on the posterior side. Three hundred microliter of Lipiodol was injected at two points 1 cm apart from each other, in the lower stomach, as a positive control for X-ray CT examination.
Immediately after the marker injection, laparoscopic analysis of the animal was performed. Conventional laparoscopy could not reveal any alteration of the gastric serosa (data not shown). NIR laparoscopy showed bright fluorescence on each side of the stomach. The anterior side of the stomach showed some blurring already, and each injection point was barely distinguishable (Fig. 23.3a). In contrast, four injection points were independently observed on the posterior side of the stomach (Fig. 23.3b).
Fig. 23.3
NIR laparoscopic appearance of the stomach immediately after marker administration. (a) Anterior side where ICG aqueous solution was administered. (b) Posterior side where DI marker was administered
Then, an X-ray CT examination of the animal was followed. Nothing but a metal clip was observed on the anterior side of the stomach (data not shown); however, four injection points as well as a metal clip were individually detected in the posterior wall (Fig. 23.4a). Volume-rendered image of the X-ray CT examination showed each injection point and a metal clip separately (Fig. 23.4b).
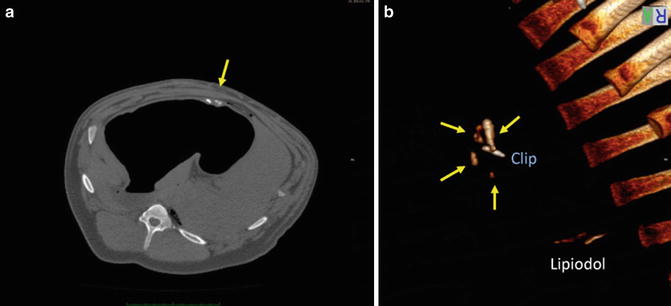
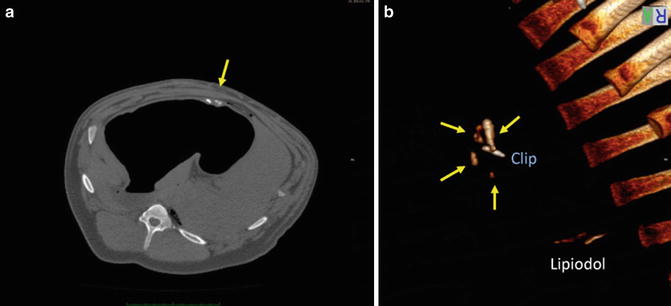
Fig. 23.4
X-ray CT images of the abdomen immediately after the marker administration. (a) Axial image for the level of the site of dual-imaging marker administration. (b) Volume-rendered images of the X-ray CT examination. Arrows indicate DI maker administered
Eighteen hours after marker administration, the animal was anesthetized and laparoscopy was performed again. NIR laparoscopy showed fluorescence of broad blurring over 7 cm on the anterior side of the stomach, and each injection point was not distinguishable (Fig. 23.5a). On the other hand, four injection points were still individually distinguishable on the other side of the stomach (Fig. 23.5b).
Fig. 23.5
NIR laparoscopic appearance of the stomach 18 h after marker administration. (a) Anterior side where ICG aqueous solution was administered. (b) Posterior side where DI marker was administered
Discussions
Preoperative marking of target lesion is essential for gastrointestinal surgeries when they are not palpable. Tattooing with India ink has been long used for the surgeries of colon and rectum since the first report by Ponsky and King in 1975 [27]. This technique is useful for rough estimate of locations of interest within such a long thin organ. However, it is not sufficient for the gastric surgeries that require precise setting of the resection line. Other dyes such as indocyanine green and indigo carmine and autologous blood have been tried to be administered preoperatively around early gastric cancer lesions to be localized intraoperatively [15, 17, 20]; however, a total volume of 2–5 ml of such markers was required to let them reach to the serosa and become visible. Therefore, these markers diffuse significantly through tissues, and resection margins varied among cases [20], suggesting these techniques remain not ideal to localize injection points in a pinpoint manner. Our technique required administration of only 0.3 ml of the marker in the submucosal layer to be visualized with NIR fluorescence laparoscope, and blurring was less than 1 cm even 18 h after administration.
So far, various other techniques to determine such precise resection line of the stomach during laparoscopic surgery have been reported. Park et al. first described the usefulness of intraoperative gastroscopy for laparoscopic gastric surgery. They detected target lesions by transillumination of scope or by pushing down the gastric wall with forceps and identifying the matching protrusion on the gastroscopy [11]. However, intraoperative gastroendoscopy is sometime cumbersome because of intratracheal intubation for general anesthesia and supine position which are not suitable for the procedure [19]. Furthermore, insufflation of the stomach and small bowel afterward with gastroendoscope might disturb subsequent laparoscopic procedures, and mobilization of the stomach sometimes causes acute alterations of the gastric mucosa such as redness and edema, hampering close observation of lesions.
In order to avoid such difficulties, combination of conventional imaging modalities such as intracorporeal ultrasonography [10] or portable radiograph [18] during laparoscopic surgery has been tried to detect preoperatively placed endoscopic marking clip. Although these techniques showed better results, they require complex procedure such as consideration of two image modalities (i.e., laparoscopic image and ultrasonographic or radiographic image) at the same time and the other space-occupying equipment and operating stuff in the OR.
The other new technologies have been also tested, as well. Ohdaira et al. introduced magnetic detection system to detect preoperatively placed marking clip [12]. This technique consisted of a small magnetic tag attached to marking clip with a nylon string and a magnetometer. It does not visualize the location of the clip; therefore, it requires a survey with the tip of a probe over the stomach. Choi et al. developed a novel fluorescent clip with NIR fluorochromes to be placed around target lesions [16]. Although it remains to be tested in an ex vivo animal model, it should be a fascinating method to detect preoperatively placed endoscopic clips in a pinpoint manner. However, these two techniques with marking clips should be considered with the risk to cause misfiring of linear staplers when they get stuck between the jaws of linear staplers during laparoscopic gastric resection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree