Thyroid nodules are a common clinical problem encountered in an endocrine practice. More and more thyroid nodules are now being detected on unrelated imaging studies, leading to an increased diagnosis of low-risk thyroid cancers. There is therefore a greater emphasis on risk assessment based on clinical and sonographic features to avoid morbidity secondary to unnecessary therapy. Molecular diagnostics are also being widely used to further characterize indeterminate nodules. The American Thyroid Association and American College of Radiology-Thyroid Imaging Reporting and Data System guidelines are the most commonly used in clinical practice for risk assessment.
Key points
- •
Thyroid nodules are a common clinical problem, and the increased use of imaging techniques has led to increased diagnosis of thyroid incidentalomas and low-risk thyroid cancers.
- •
Greater emphasis is being placed on risk assessment and sonographic features to avoid unnecessary evaluation and therapy.
- •
Ultrasound-guided fine need aspiration cytology remains the gold standard test to evaluate thyroid nodules.
- •
Molecular diagnostics are being widely used for further risk assessment and characterization of indeterminate thyroid nodules.
Introduction
Epidemiologic studies show that about 5% women and 1% men have palpable nodules in the iodine-sufficient areas of the world. With the advent of high-quality imaging techniques and more patients undergoing radiological imaging for a myriad of clinical problems, thyroid nodules have become a common clinical issue. Most of these nodules are benign; however, the clinical importance lies in the need to exclude cancer.
As per the Surveillance, Epidemiology and End Results (SEER) data, thyroid cancer constitutes 3.0% of all newly diagnosed cancers, and there were an estimated 52,070 new cases diagnosed in 2019. However, the prognosis is excellent, with an overall 5-year survival of 98.2%.
Greater use of thyroid ultrasound has led to an increased diagnosis of low-risk thyroid cancer. Thus, there is a greater emphasis on risk assessment and outcome prediction to minimize morbidity and unnecessary therapy. This strategy led to the changing paradigm in thyroid cancer management from the traditional model of one size fits all to a risk adapted paradigm that involves management based on individualized risk assessment.
Thyroid nodules
A thyroid nodule is a discrete lesion within the thyroid gland that is radiologically and histologically different from the surrounding thyroid parenchyma. Both benign and malignant thyroid disease can cause thyroid nodules. Thyroid cancer occurs in 7% to 15% of any thyroid nodule. ,
Palpable and nonpalpable nodules
The estimated annual incidence rate of thyroid nodules is 0.1% in the United States. The frequency of thyroid nodules, about half of which are solitary on physical examination, increases throughout life. Thyroid nodules are more common in elderly persons, females, people from iodine-deficient geographic areas, and in those with a history of radiation exposure. Single nodules are about 4 times more common in women than in men. Nodules are 10 times more frequent when the gland is examined at autopsy, during surgery, or by ultrasonography. Clinically unrecognized thyroid nodules are common and can be found in up to 50% to 60% of patients at autopsy.
Detection
Thyroid nodules can be detected during palpation by the patient or on physical examination by a physician. They are often diagnosed during work-up for hypothyroidism or hyperthyroidism. They are also commonly noted incidentally on imaging studies performed for an unrelated condition. A thyroid nodule discovered during either imaging study or surgery performed because of an unrelated thyroid gland pathology is known as a thyroid incidentaloma. The prevalence rate of a thyroid incidentaloma is 67% with thyroid ultrasound imaging, 16% with computed tomography (CT) or MR imaging, 9.4% by carotid duplex ultrasound, and 2% to 3% with fluorodeoxyglucose (FDG) positron emission tomography (PET). Thyroid incidentalomas, thus, represents a large proportion of patients seen for evaluation of thyroid nodules in an endocrine practice.
Initial evaluation
History and Physical Examination
The initial evaluation for thyroid nodule(s) is comprised of a thorough history and physical examination. Any personal or family history of benign or malignant thyroid disease should be obtained. The patient should be evaluated for symptoms of hypothyroidism or hyperthyroidism. Pertinent history that increases the risk of malignancy includes a history of head or neck radiation, presentation at extremes of age (less than 14 or more than 70 years), history of rapid growth of the nodule, persistent dysphonia, male gender, and significant family history of differentiated thyroid cancer, medullary thyroid cancer, or multiple endocrine neoplasia (MEN), Type 2.
A complete thyroid examination with palpation of the thyroid gland should be performed. The location, size, and consistency of any palpable nodules should be assessed. Any neck tenderness or cervical adenopathy should also be noted. A complete review of systems for any signs and symptoms of hypothyroidism and hyperthyroidism should also be performed ( Table 1 ).
| Hyperthyroidism | Hypothyroidism |
|---|---|
| Palpitations | Dry skin and hair |
| Heat intolerance | Cold intolerance |
| Weight loss | Weight gain |
| Frequent bowel movements | Constipation |
| Anxiety | Fatigue |
| Oligomenorrhea | Menorrhagia |
| Increased appetite | Decreased appetite |
Diagnosis
Laboratory Studies
The initial laboratory step in the work-up to evaluate a thyroid nodule is obtaining a TSH (thyroid-stimulating hormone) level. A suppressed or low TSH, which signifies a hyperthyroid state, is associated with a decreased probability of malignancy. The management of patients with a low serum TSH is described later in this article. On the other hand, an increased level of serum TSH, even when the level is still within reference limits, is statistically associated with an increased risk of cancer in thyroid nodular disease. Routine measurement of serum thyroglobulin and serum calcitonin is not recommended in the initial evaluation of thyroid nodules.
Imaging
Thyroid ultrasound
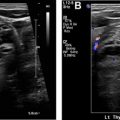
All patients with a suspected thyroid nodule, a known nodular goiter, or a thyroid nodule incidentally diagnosed on any other imaging study should undergo a diagnostic thyroid ultrasound . High-resolution ultrasound is the most sensitive imaging technique to detect thyroid nodules, and it is well-suited to evaluate the gland architecture. Thyroid ultrasound should be used to determine the size and number of nodules and provide a description of any abnormal lymphadenopathy in the neck. The size and sonographic features of the nodules (eg, composition, echogenicity, shape, margins, and echogenic foci) are taken into consideration while deciding the need for fine needle aspiration (FNA) as described later in this article. ,
Thyroid ultrasound is not indicated in patients with medical thyroid disease if the gland is normal in size without evidence of a palpable nodule on physical examination. It is also not indicated as a screening test except in patients with high genetic risk or possibly in those with history of radiation to the head or neck region.
Ultrasound elastography, which uses both sonography and a computational module to measure tissue stiffness, has been used in some institutions to assess cancer risk. Recently, larger clinical trials show that ultrasound elastography has been inferior to gray scale sonography, especially with partially cystic or cystic nodules. Patients with multinodular goiter, coalescence of nodules, obese patients, or those with nodules that are inferior or posterior are not candidates for ultrasound elastography.
Other imaging modalities
A chest radiograph is not useful and therefore not recommended for evaluation of the thyroid gland, although it may indicate a substernal goiter, which typically presents as a mass associated with tracheal narrowing, tracheal stenosis, and mediastinal widening causing shortness of breath.
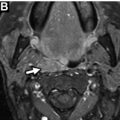
Cross-sectional imaging with CT scan is recommended to evaluate and confirm substernal extension and tracheal compression. It is also recommended in suspected advanced thyroid cancer to assess for nodal disease and widespread metastases. Iodinated contrast administration should be avoided in patients with suspected thyroid cancer, as it will delay therapy with radioactive iodine (RAI).
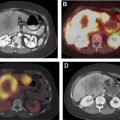
FDG-PET imaging is not recommended for the evaluation of patients with newly detected thyroid nodules or thyroid disease. Incidental FDG-PET uptake in the thyroid gland is seen in 2% to 3% patients and can be either focal or diffuse. Focal FDG-PET uptake in the thyroid is associated with an approximately 35% risk of being cancerous. For PET-positive nodules greater than 1 cm diameter, a dedicated ultrasound and FNA are recommended. However, diffuse FDG uptake in conjunction with sonographic and clinical evidence of chronic lymphocytic thyroiditis does not require further imaging or FNA.
Multinodular goiter and toxic nodules
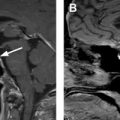
A radioactive iodine uptake and scan should be obtained if the TSH is low to assess whether the nodule is hyperfunctioning. The pattern of uptake in a patient with a single hyperfunctioning nodule generally shows focal uptake in the adenoma with suppressed uptake in the surrounding and contralateral thyroid tissue ( Fig. 1 ).

No further cytology evaluation is generally recommended for a hyperfunctioning nodule, as these nodules rarely harbor malignancy. However, the prevalence of thyroid cancer in hyperfunctioning nodules is approximately 3%. Therefore, in clinical practice, FNA of a hyperfunctioning nodule should be considered in patients with risk factors for thyroid cancer, any nodules with suspicious sonographic features, and those that show growth on surveillance.
Patients with a suppressed TSH who are noted to have one or more hyperfunctioning nodules on uptake and scan should also undergo thyroid ultrasound to evaluate the presence of nodules concordant with the hyperfunctioning areas on the scan and other nonfunctioning nodules that might be present ( Fig. 2 ).

A multicenter study looked at association of thyroid cancer in patients with nodular Graves’ disease and found the rate of carcinoma in a cold nodule was 15% (n = 140 patients). In patients with nodular Graves’ disease, ultrasound-guided FNA is useful before radioiodine therapy or surgery.
The risk of thyroid cancer in patients with a multinodular goiter is the same as in those with a solitary nodule. , Therefore, all nodules within a multinodular goiter that meet sonographic and size criteria concerning for malignancy should undergo biopsy.
Fine Needle Aspiration
FNA is the procedure of choice in the histologic evaluation of thyroid nodules. The nodule size at initial ultrasound, the ultrasound characteristics, and definite increase in size during follow-up are generally considered as reasonable criteria for deciding whether to proceed with FNA. FNA should be performed under ultrasound guidance to ensure optimal placement of the needle tip for nodule sampling.
In the United States, the two commonly used guidelines to estimate risk of malignancy, and thus assess a need for FNA, are the ATA (American Thyroid Association) guidelines and the ACR TI-RADS (American College of Radiology Thyroid Imaging Reporting and Data System). ,
Table 2 shows the ATA ultrasound features and criteria for biopsy as per the guidelines. In comparison, Fig. 3 shows thyroid nodule imaging features and guidelines for biopsy as recommended by the ACR TI-RADS reporting system.