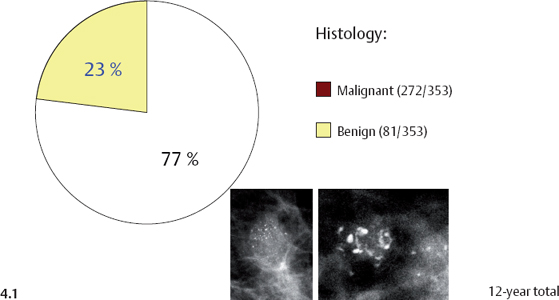
Differential Diagnosis of Breast Diseases Producing Clustered, Discernible Calcifications
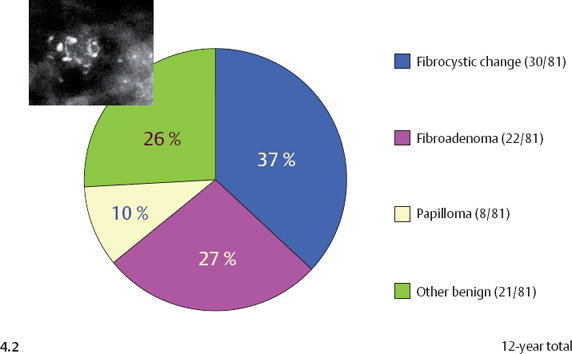
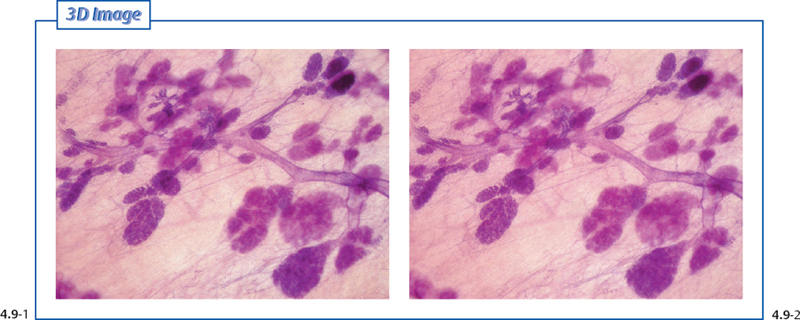
Clustered, discernible calcifications with a crushed stone-like appearance may be associated with both malignant and benign processes in the breast. Crushed stone-like calcifications are the most frequent among the malignant type calcifications. The most frequent benign, hyperplastic breast changes that may be associated with discernable crushed stone-like calcifications are fibrocystic change, fibroadenoma, and papilloma, all of which may cause considerable differential diagnostic problems (see Fig. 4.2). A better understanding of these underlying benign and malignant pathophysiological processes can be gained through the study of subgross, 3D histological images. This understanding will greatly assist in the interpretation of the images and in determining the most likely etiology of the calcifications.
Introduction
Fibrocystic Change: Pathophysiology, Imaging, and Differential Diagnosis
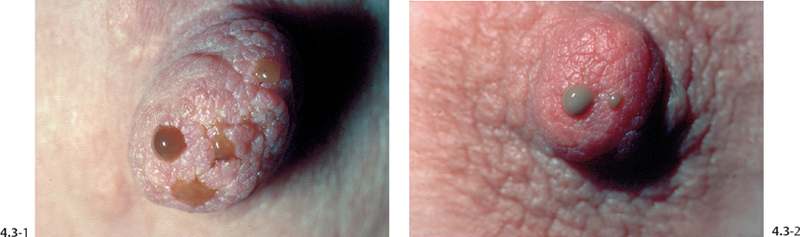
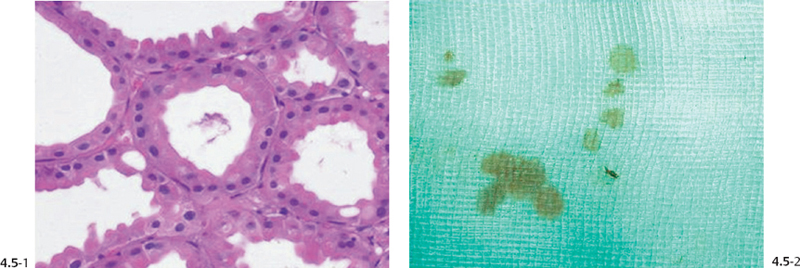
Fibrocystic change is a clinically and radiologically detectable form of ANDIs (Aberrations of Normal Development and Involution 1), which includes apocrine metaplasia, cysts, ductectasia, and fibrosis. The apocrine metaplastic cells produce a proteinaceous fluid which dilates the TDLUs and the adjoining ducts, most often producing cysts. This excess fluid may result in spontaneous nipple discharge through multiple duct openings in the nipple, often bilaterally. The high protein content and cellular debris give the fluid a cloudy, turbid appearance in varying shades of green, gray, yellow, or milky. Calcified crystals (so-called psammoma bodies) may precipitate in the dilated acini and may occasionally be detectable on the mammogram.
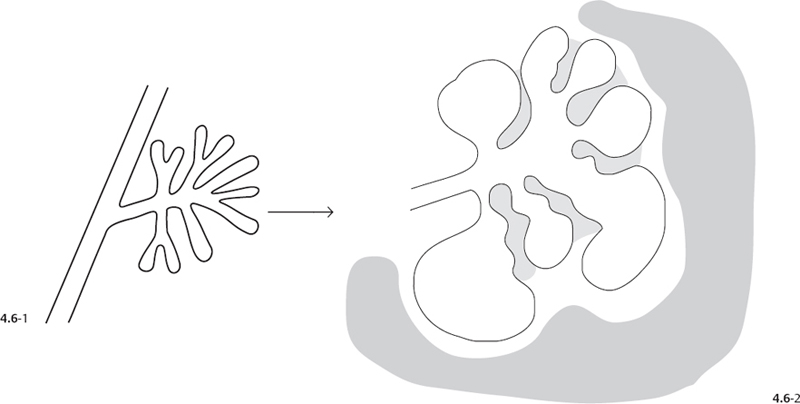
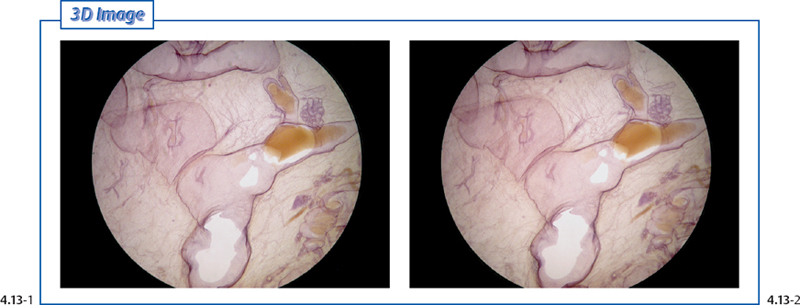
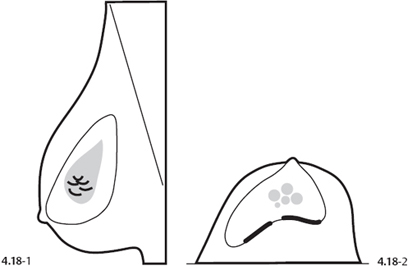
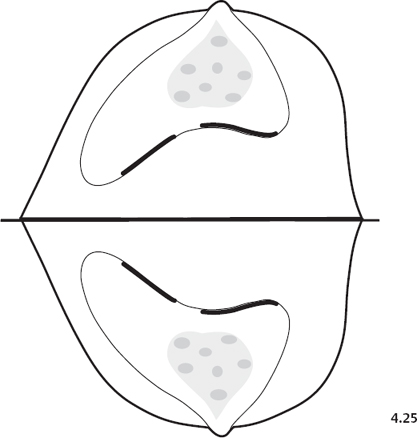
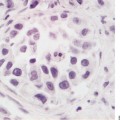
Explanatory Illustration of the Pathophysiological Process Leading to the Formation of Teacup-like Calcifications in Fibrocystic Change
Figs. 4.17-1 to 8 This composite of images illustrates the underlying pathophysiology of fibrocystic change and demonstrates how the characteristic mammographic image of the “teacup-like” calcifications is formed in the two orthogonal projections.2,3 When viewing calcifications on the mammogram, the most helpful approach is first to imagine their anatomical location in terms of the 3D subgross images and then to attempt to determine the pathological process that has formed them. This stepwise analytical process, which combines the mammogram first with subgross, 3D pathology and then with conventional, 2D pathology, will enable the radiologist to achieve a more specific differential diagnosis.
Comment
When teacup-like calcifications are seen on the mammogram, either as single or multiple clusters or diffusely scattered, the finding indicates fibrocystic change with no mammographic sign of malignancy.
Comparative Mammographic-Histological Demonstration of the Sediment Resulting in Teacup-like Calcifications
Comparative Galactographic-Subgross 3D Histological Demonstration of Fibrocystic Change
The resolving power of mammography and galactography allows visualization of structural changes such as distention and distortion of ducts and TDLUs by pathological processes. Subgross, 3D histology visualizes the same structural changes. This makes it a more useful teaching aid for the imager than is conventional histology, which demonstrates cellular details but is less effective at illustrating the three-dimensional aspects.
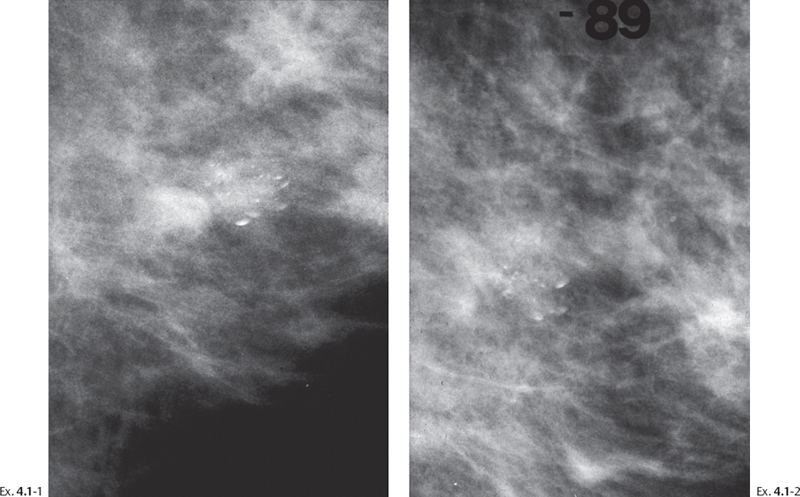
Demonstration of the Natural History of Focal Fibrocystic Change with Calcifications
When the mammographic finding is only a cluster of teacup-like calcifications, the diagnosis of benign fibrocystic change can be made with confidence. The number and density of these benign-type calcifications may increase, decrease, or remain unchanged at serial mammographic examinations. Since malignant-type calcifications may also either increase or decrease in number and density, or even remain unchanged for years, the differential diagnostic value of such changes over time is unreliable. Numerous supporting examples appear in this book (Examples 1.1, p. 10; 2.2, p. 28; 2.7, p.43; 2.14, p. 77; 2.15, p. 84; 2.16, p. 90); in Breast Cancer: The Art and Science of Early Detection with Mammography. Perception, Interpretation, Histopathological Correlation (Figures 6.51, p. 214; 6.52, p. 215; 6.61, pp. 228-9) and in Breast Cancer: Early Detection with Mammography. Casting Type Calcifications: Sign of a Subtype with Deceptive Features (Examples 2.2, p. 80; 2.3, p. 86; 2.4, p. 90; 2.10, p. 118; 2.11, p. 124; 4.4, p. 206; 5.2, p. 238).
Conclusion:
Changes in the appearance of calcifications at follow-up mammography do not constitute a reliable diagnostic criterion for the exclusion of malignancy.
The following two examples demonstrate temporal changes in the mammographic appearance of calcifications associated with fibrocystic change.
Example 4.1
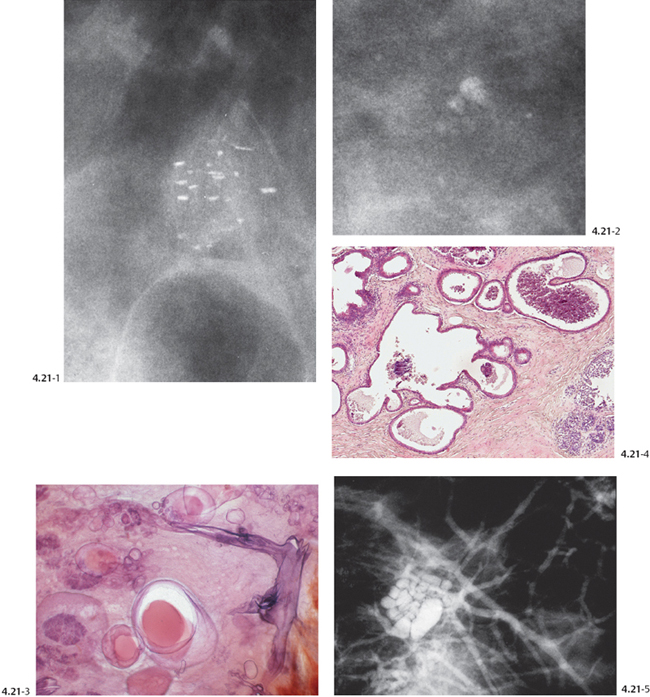
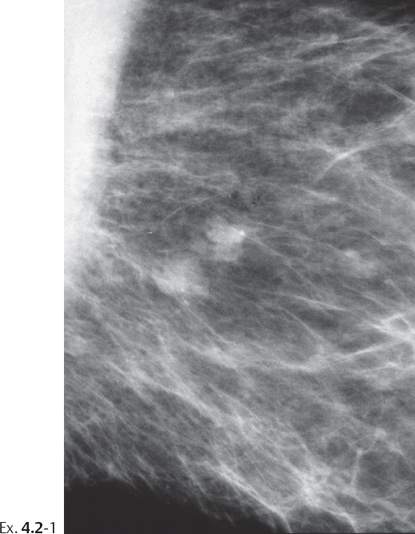
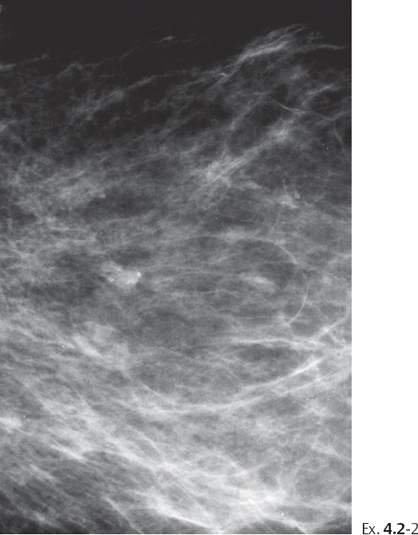
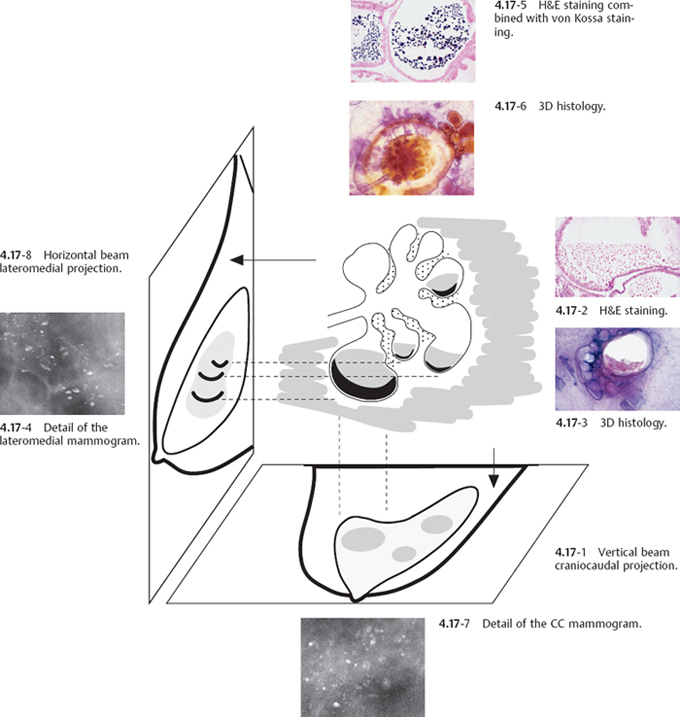
Example 4.2
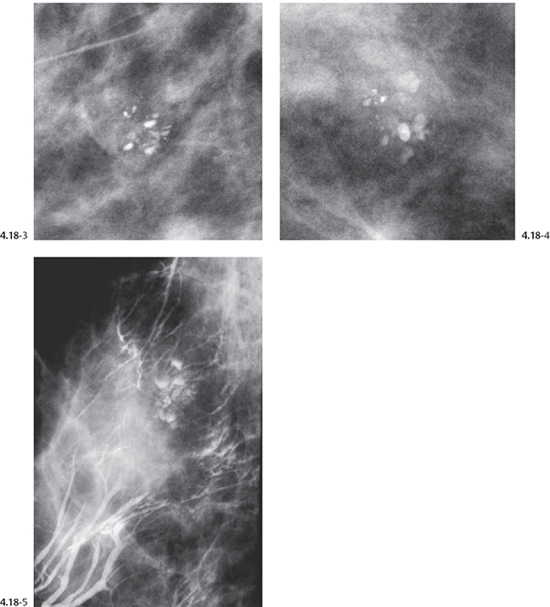
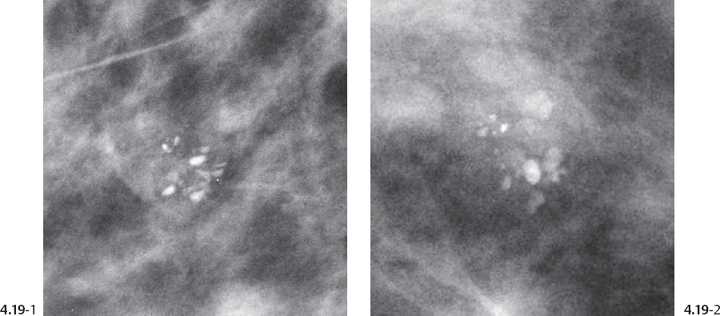
Ex. 4.2-3 to 5 Microfocus magnification images demonstrate the individual,de-novo,irregular calcifications within cystically dilated acini. As illustrated on the 3D histological image (Ex. 4.2-6), the calcifications fill in the unevenly distended acini.
Comment
Fibrocystic change with or without associated calcifications is the most frequently occurring hyperplastic breast change and the most frequent cause of call-backs from screening. When the mammographic signs are unequivocal, it is safe to return these women to regular screening. If doubt exists, large-bore percutaneous needle biopsy is the procedure of choice. Short-term follow-up does not solve the diagnostic problem.
Demonstration of the Bilateral, Extensive Fibrocystic Change with Calcifications
When the mammographic finding consists of bilateral, multiple clusters of teacup-like calcifications that give the impression of being diffusely scattered, the most probable diagnosis is benign fibrocystic change. However, when there are large variations in the size, density, and shape of the calcifications associated with fibrocystic change, percutaneous or surgical biopsy is indicated.
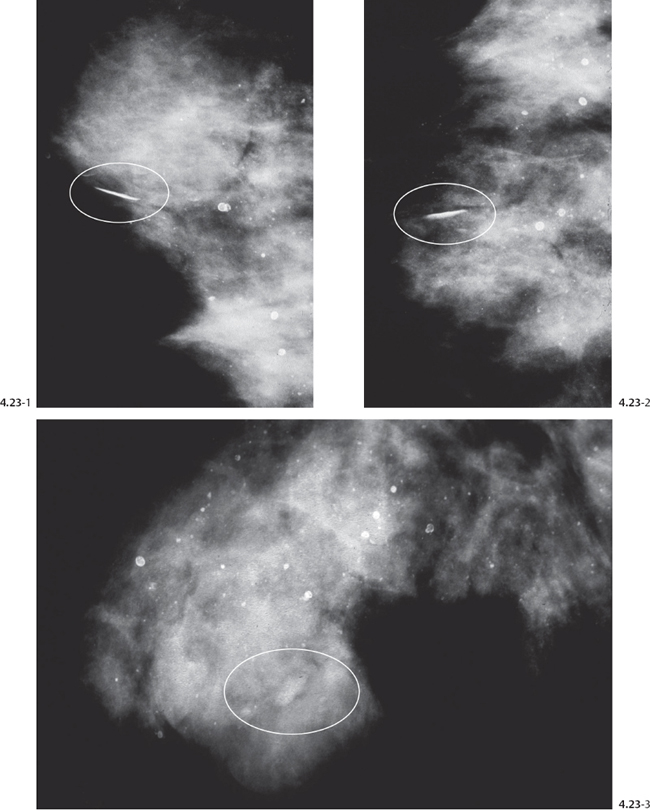
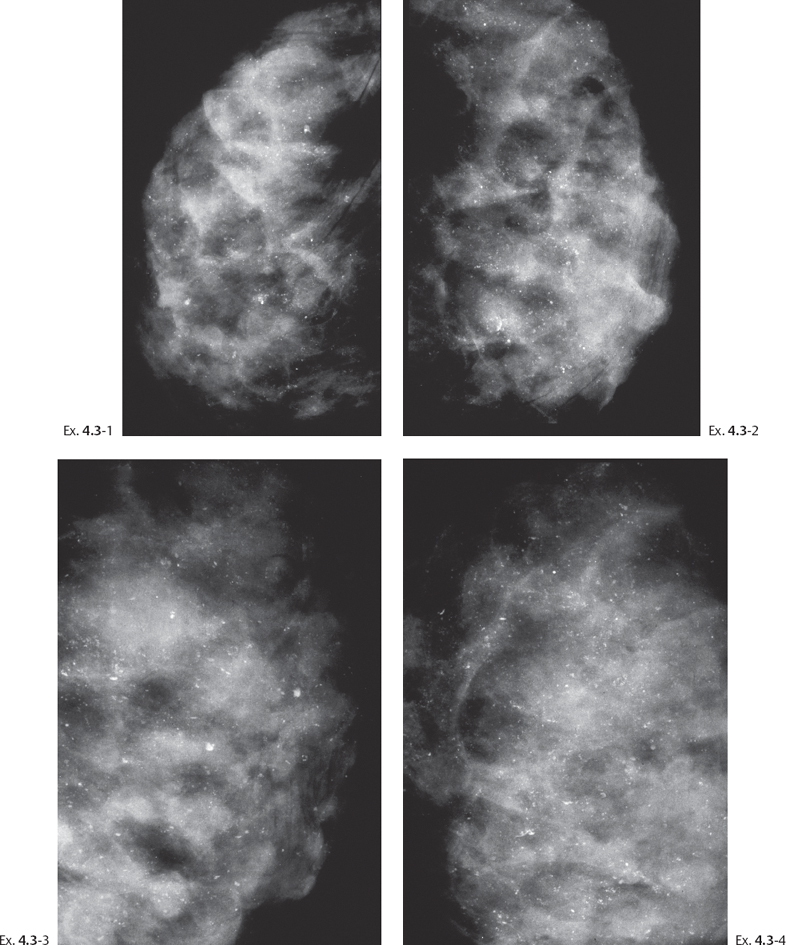
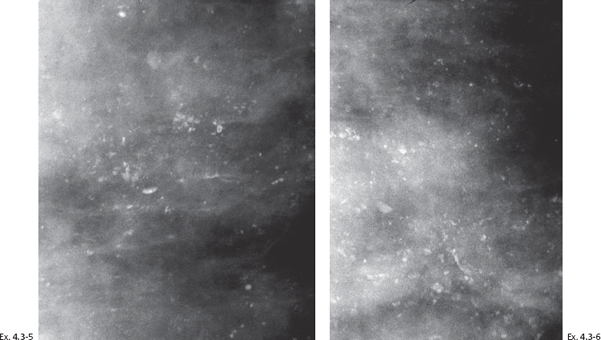
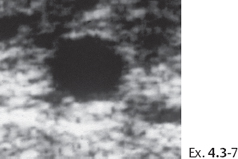
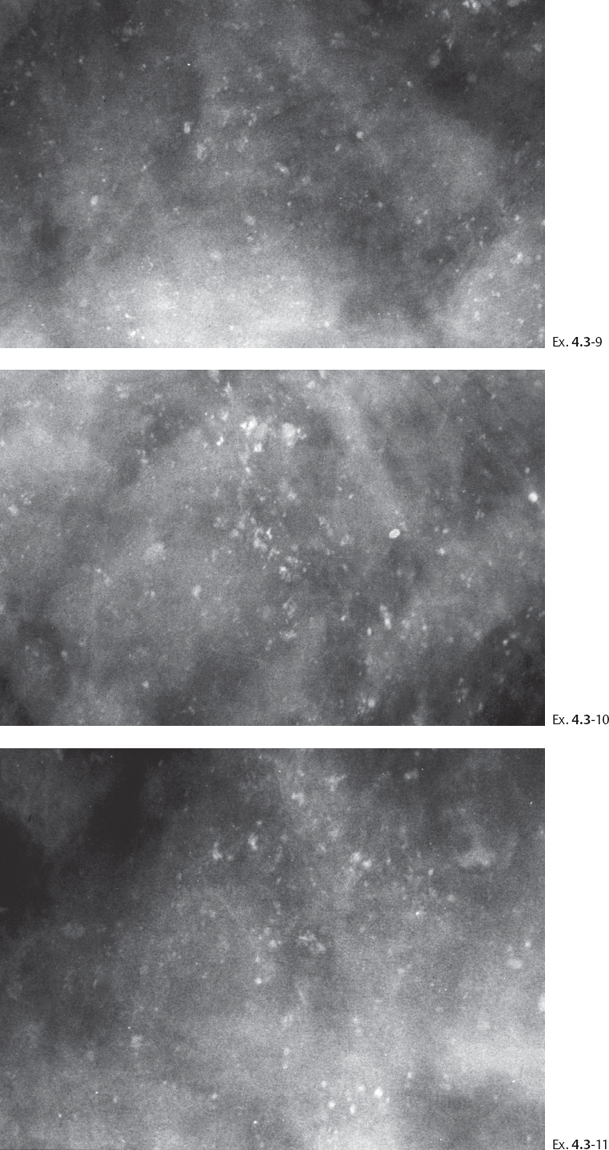
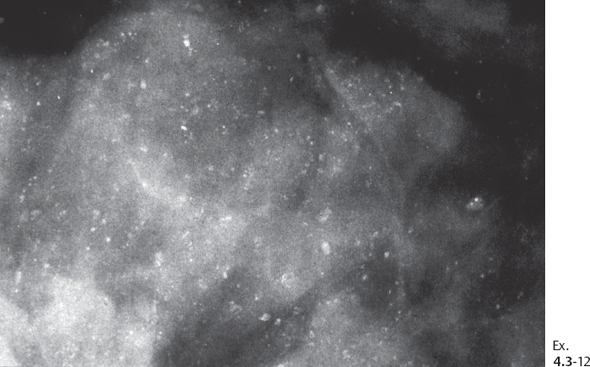
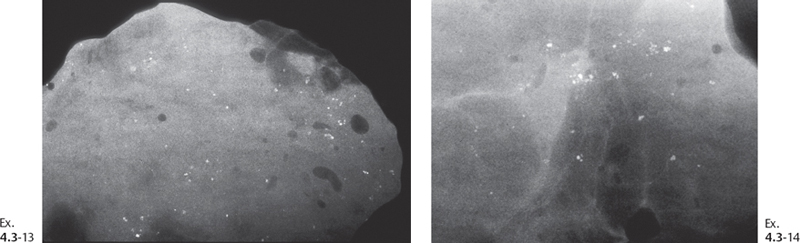
Example 4.3
A 54-year-old woman, screening examination.
Demonstration of the Bilateral, Extensive Fibrocystic Change with Calcifications
Demonstration of the Bilateral, Extensive Fibrocystic Change with Calcifications
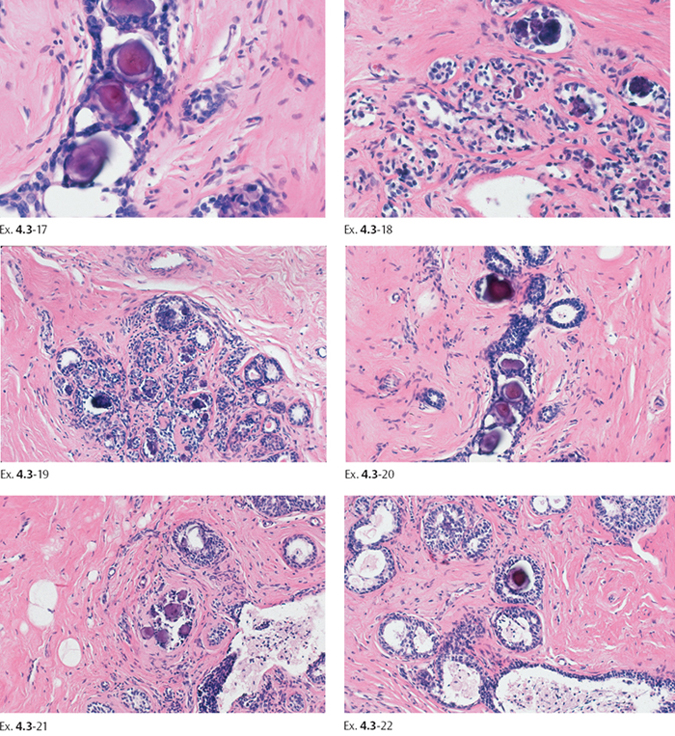
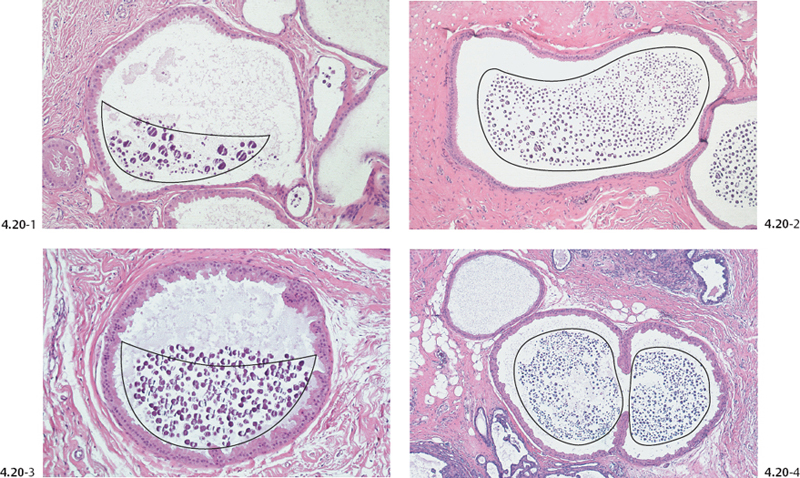
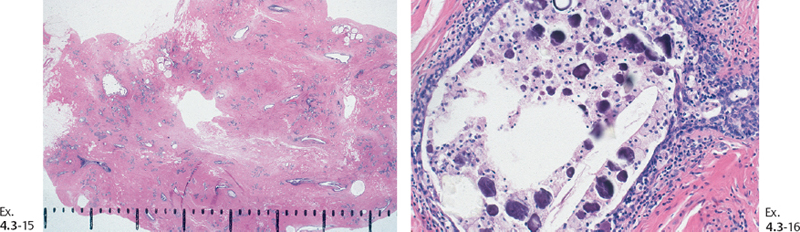
Ex. 4.3-17 to 22 A series of low- and medium-power histological images showing involutional changes associated with psammoma body-like calcifications. No histological signs of malignancy were found. Ex. 4.3-15 & 16 are tissue samples from the right breast; Ex. 4.3-17 to 22 are tissue samples from the left breast.
Demonstration of the Three Types of Calcifications Occurring in Fibrocystic Change
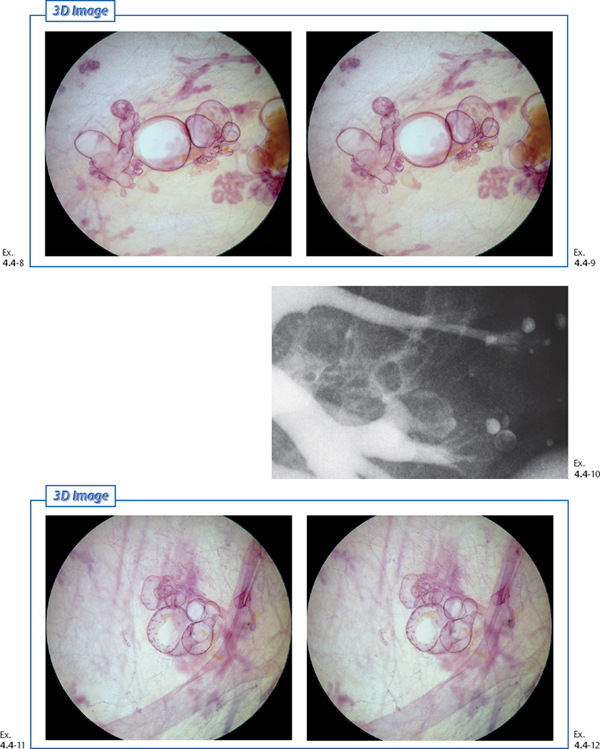
Example 4.4
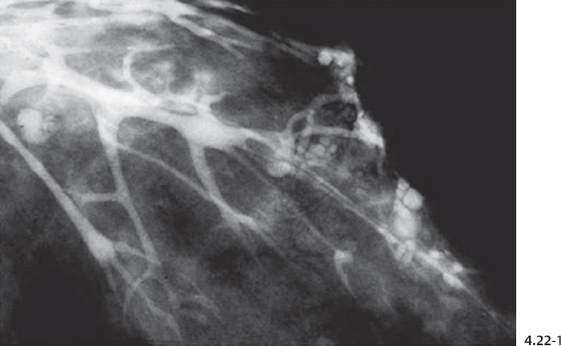
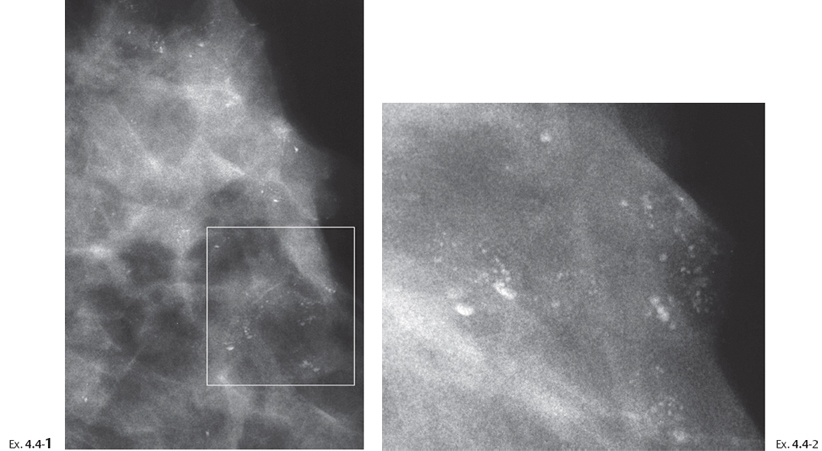
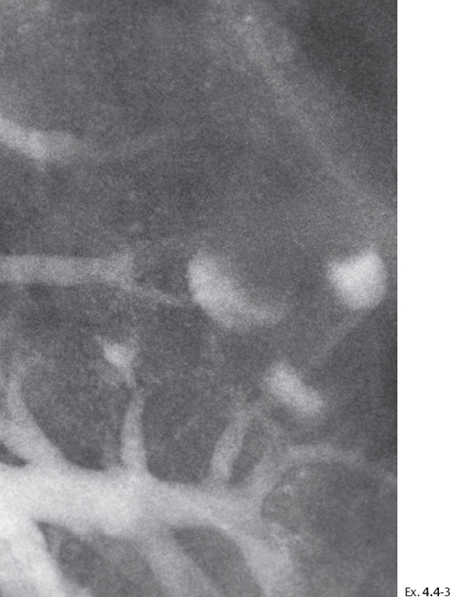
A 44-year-old woman presented with greenish discharge from the left nipple. Following the mammographic work-up, galactography was performed to elucidate the cause of the discharge.
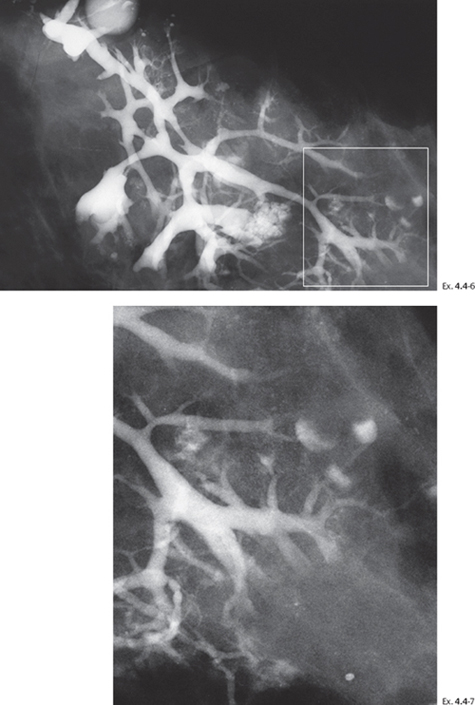
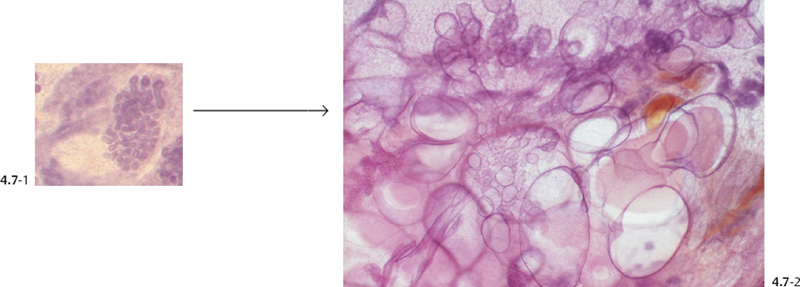
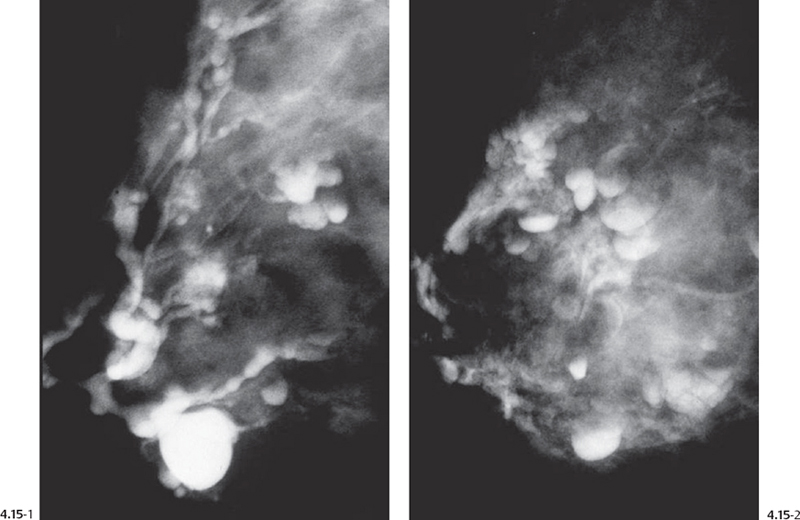
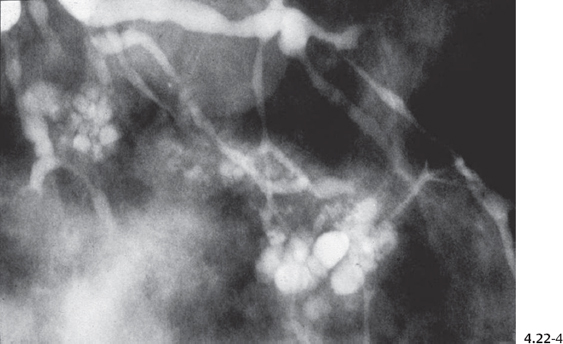
Ex. 4.4-6 & 7 The galactogram outlines the entire lobe with its dilated ducts. Some of the TDLUs are also cystically dilated.
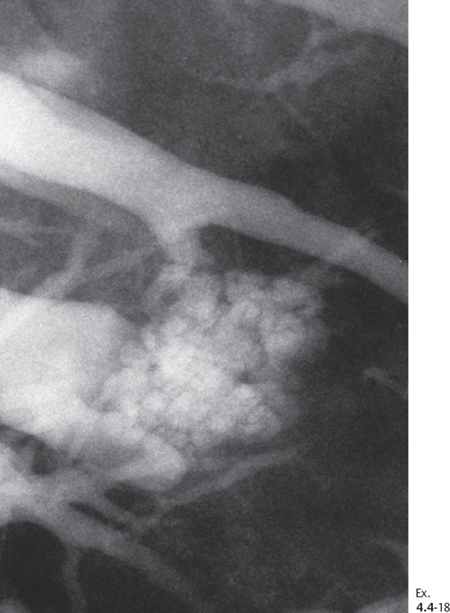
Demonstration of the Three Types of Calcifications Occurring in Fibrocystic Change
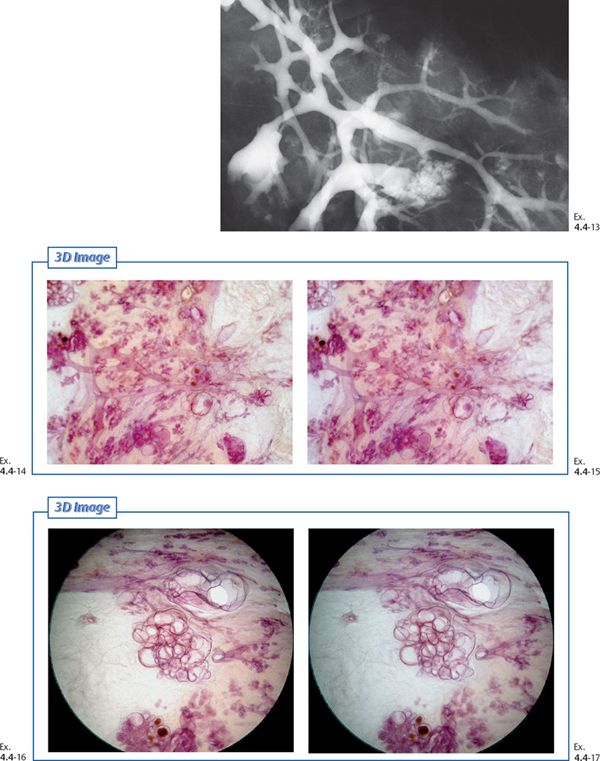
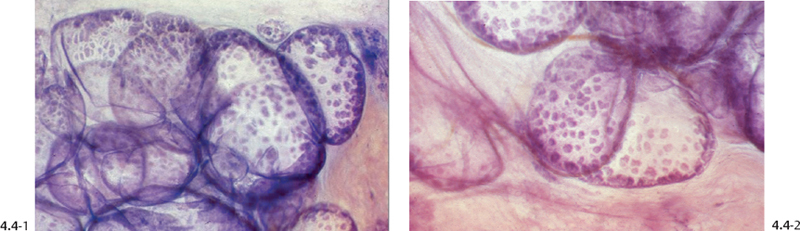
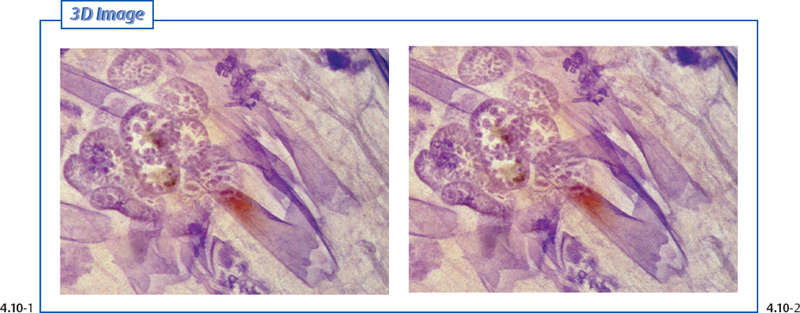
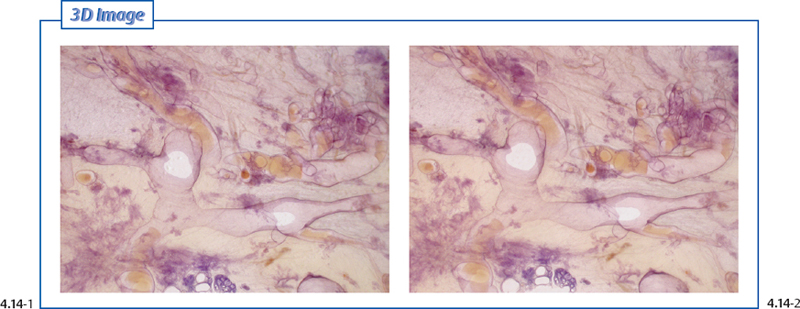
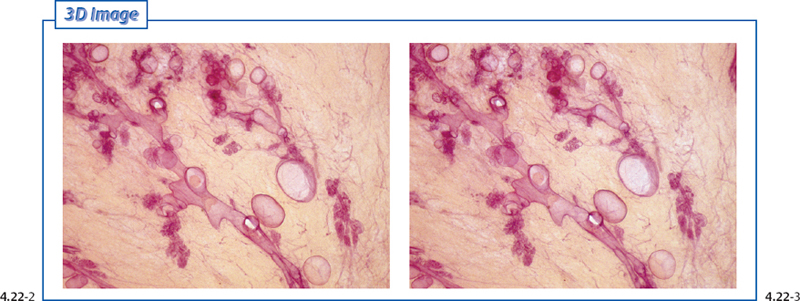
Ex. 4.4-13 to 17 Galactographic/3D histological correlation of fibrocystic change with ductectasia, multiple cystically dilated TDLUs and associated fibrosis.
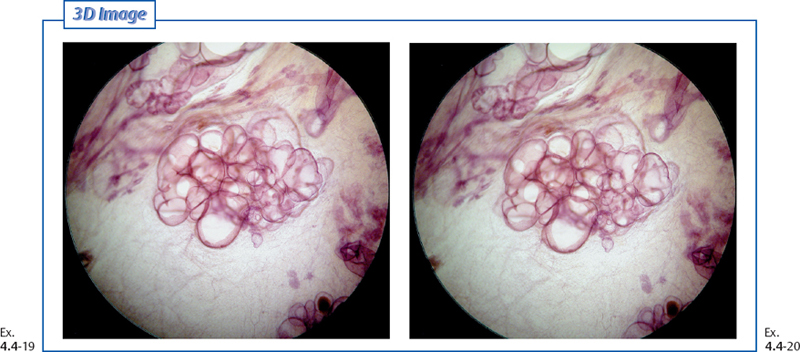
Demonstration of the Three Types of Calcifications Occurring in Fibrocystic Change
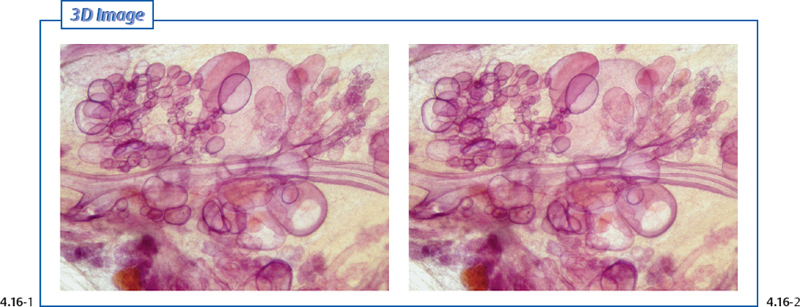
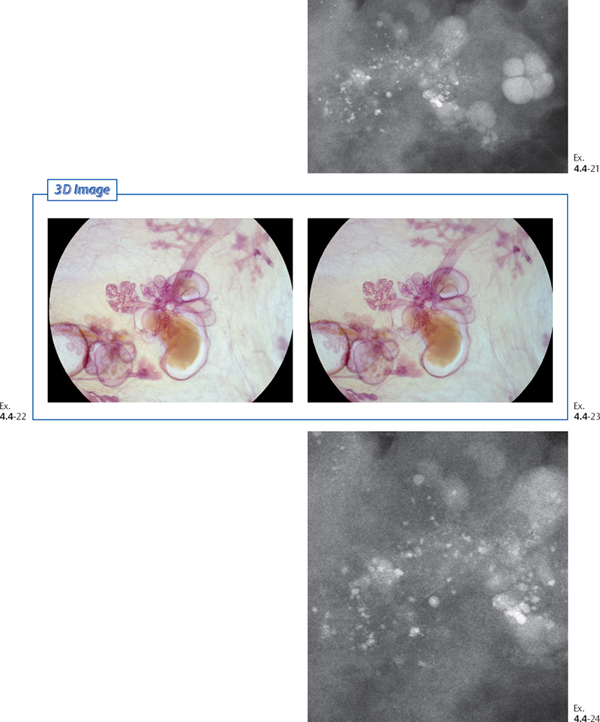
The most frequently occurring is the psammoma bodylike calcification. Their summation appears on the mammogram as sediments, teacup-like or rounded/oval calcifications, causing minimal differential diagnostic problems (Ex. 4.4-21 to 24).
Demonstration of the Three Types of Calcifications Occurring in Fibrocystic Change
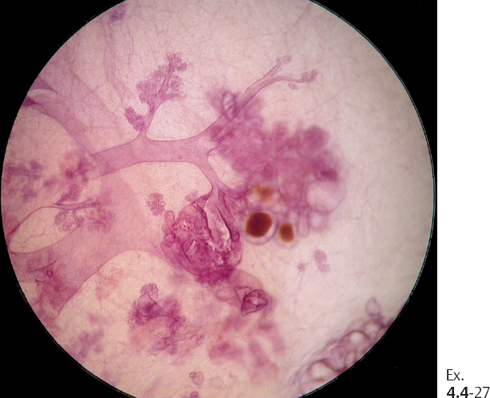
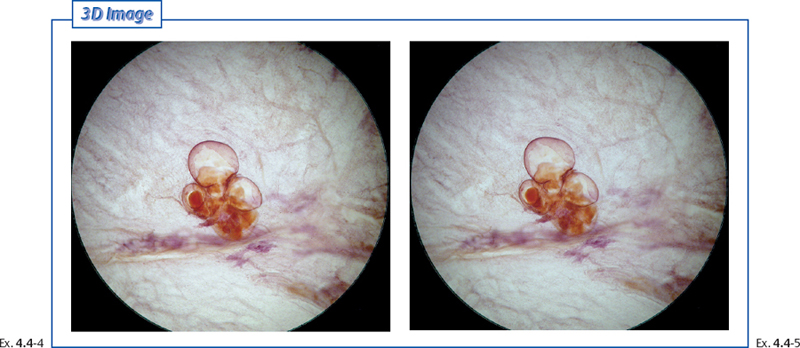
Ex. 4.4-27 Subgross, 3D histological image of the distended TDLU, corresponding to the TDLU shown in Ex. 4.4-8 & 9. Some of the acini are fluid-filled; others contain cell proliferation, preventing the contrast medium from filling the TDLU.
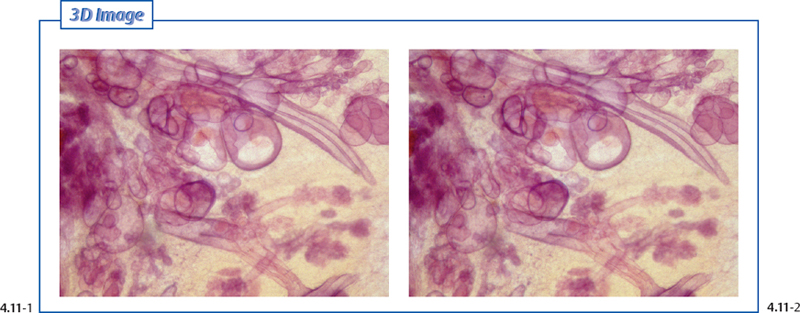
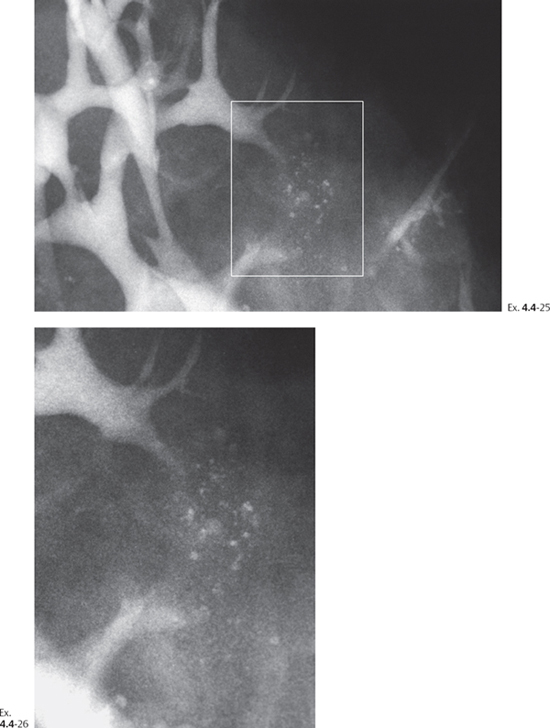
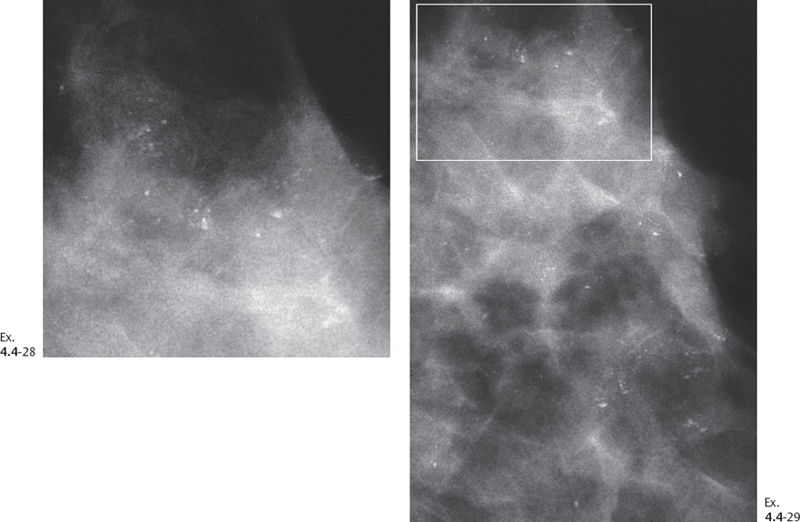
Whenever amorphous calcifications (see p. 17) are formed in the breast tissue, their mammographic image may resemble the crushed stone-like calcifications associated with malignant processes. In these cases biopsy becomes necessary for the correct diagnosis (Ex. 4.4-28 to 34).
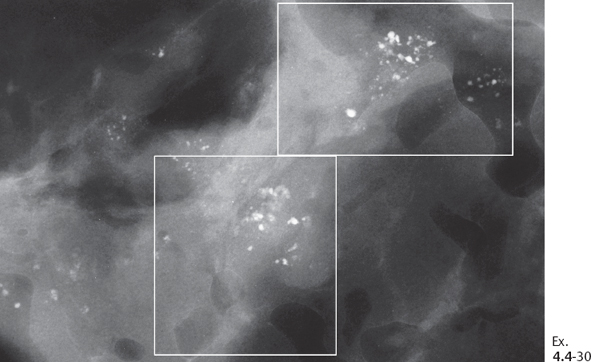
Ex. 4.4-30 Specimen radiograph. The suspicious clusters of calcifications have been surgically removed. Microfocus magnification images of the clusters within the rectangles are correlated with histological images in Ex. 4.4-32 & 33.
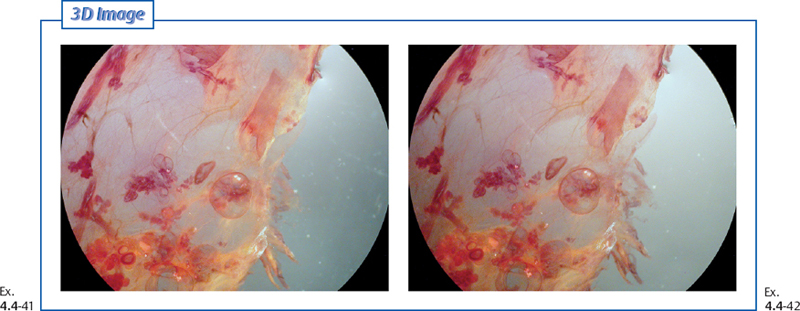
Demonstration of the Three Types of Calcifications Occurring in Fibrocystic Change
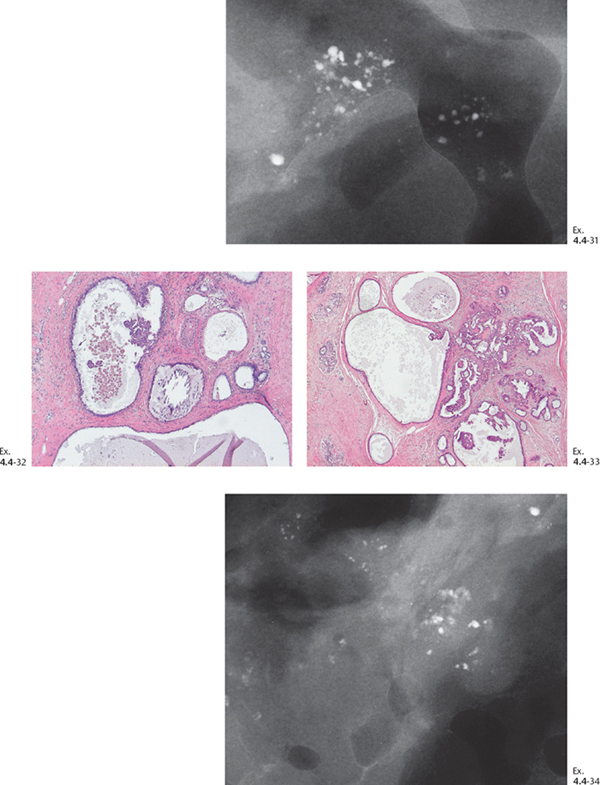
Ex. 4.4-31 to 34 Magnified views of the areas outlined by rectangles in Ex. 4.4-30. Surprisingly, amorphous calcifications were found within the cyst fluid at histology (32, 33) (ovals), which explains the presence of crushed stone-like calcifications on the mammograms.
Demonstration of the Three Types of Calcifications Occurring in Fibrocystic Change
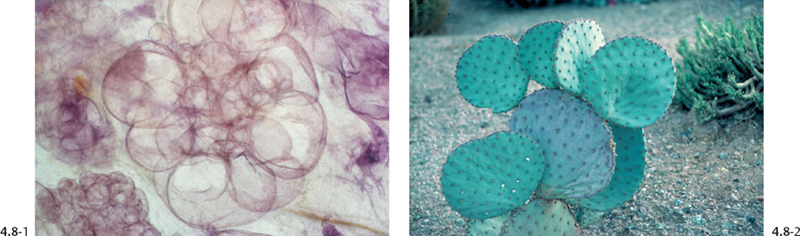
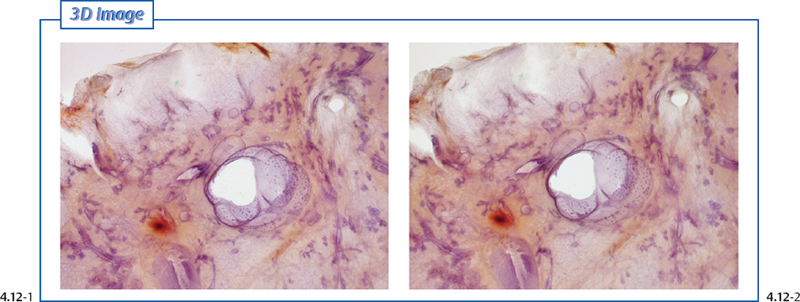
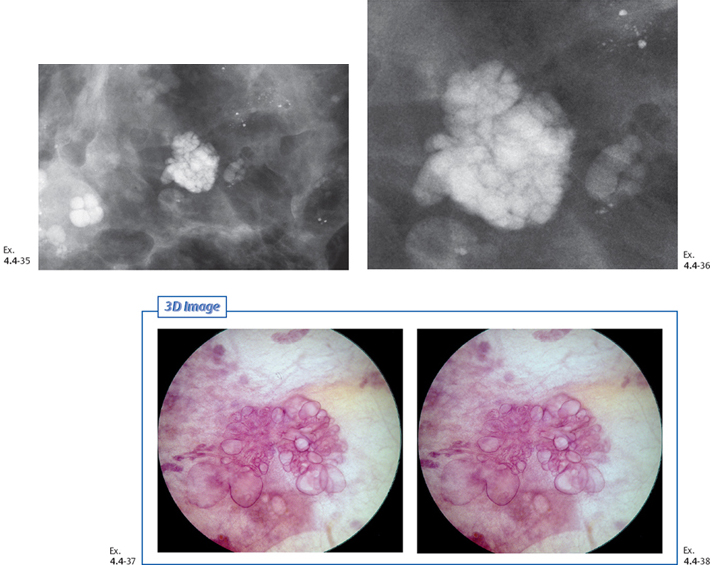
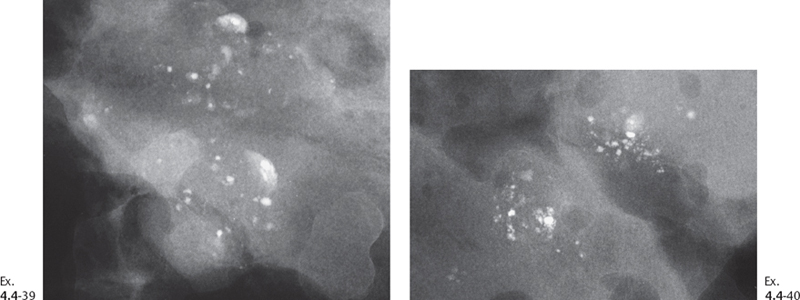
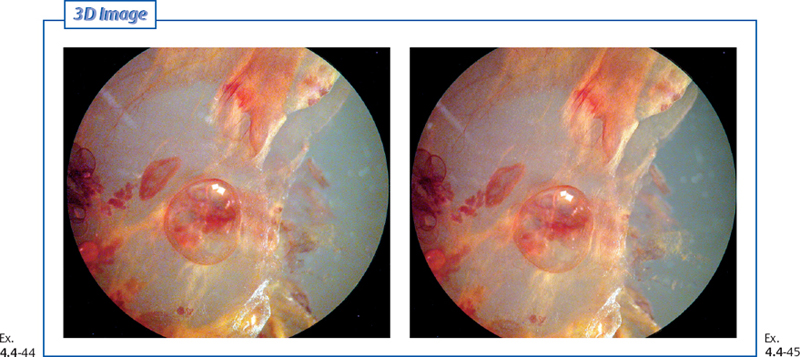
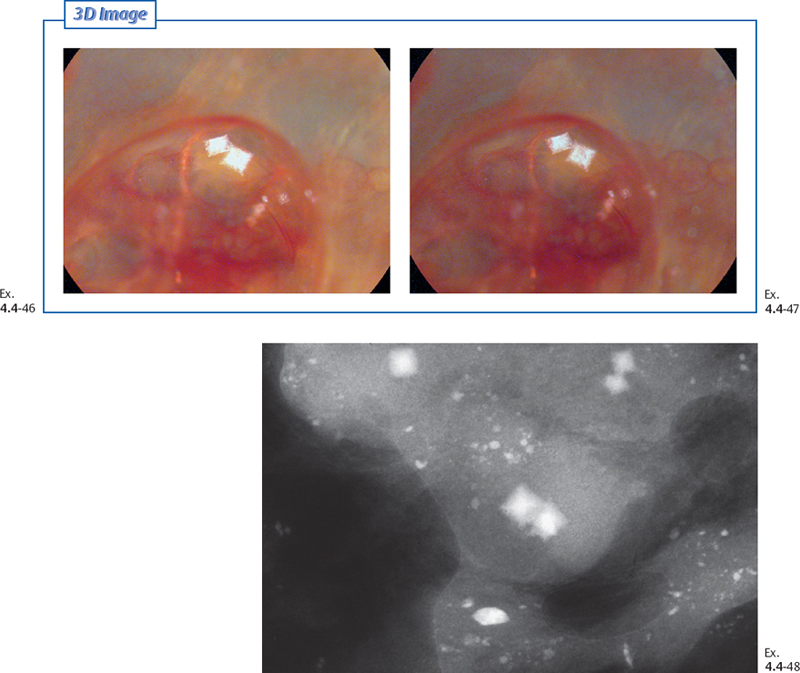
The third type of calcification associated with benign fibrocystic change, which may be confused with the crushed stone-like calcifications, are those caused by calcium oxalate crystals. These may cause differential diagnostic problems.
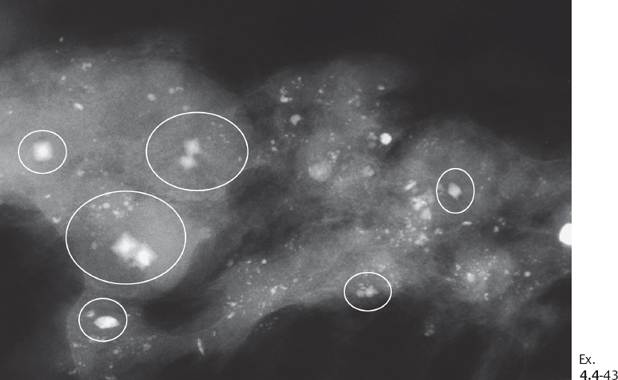
Ex. 4.4-43 Specimen slice radiograph containing octahedron-shaped calcium oxalate crystals, termed weddellite (ovals). Some of these crystals have an irregular form and are difficult to distinguish from crushed stone-like calcifications.4,5
Demonstration of the Three Types of Calcifications Occurring in Fibrocystic Change
The name “weddellit” originates from calcium oxalate crystals discovered in sediment samples from the Weddell Sea in Antarctica.4 The sea was named after the British explorer and seal hunter James Weddell (1787-1834), who explored the southern seas on the brigantine Jane
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree